
 |
|
João Vitor de Oliveira1,a; Alexandre Peroni Borges2,b; Rodrigo Menezes Jales1,c; Konrado Tenorio2,d; Eduardo Miquelino de Oliveira Junior2,e
DOI: 10.1590/0100-3984.2025.0070
e20250070
Publish in: November 28 2025
ABSTRACT
OBJECTIVE: To determine whether the degree of microvascular flow on Doppler ultrasound correlates with the aggressiveness of prostate cancer, as defined by the Gleason score.
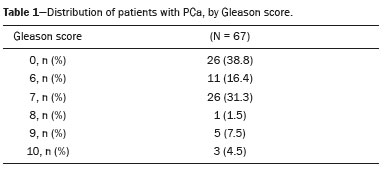
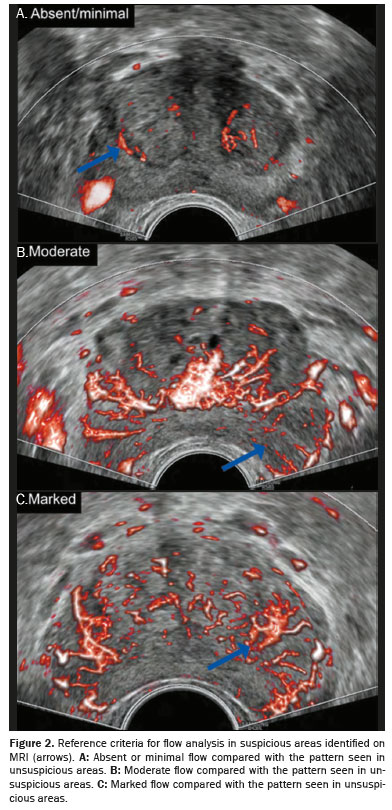
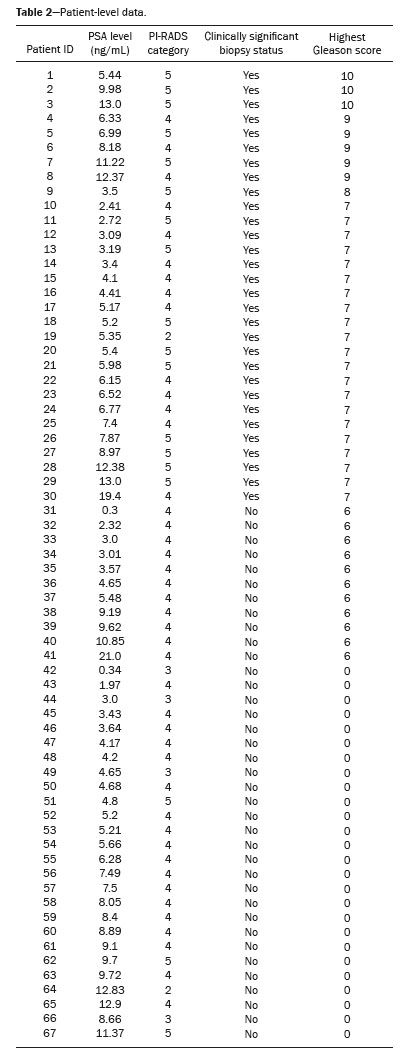
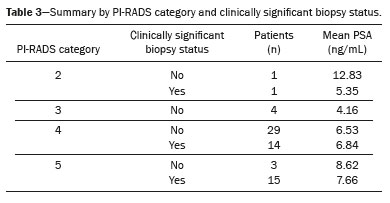
MATERIALS AND METHODS: This was a prospective cohort study including 88 patients evaluated between November 2023 and July 2024. We included men between 48 and 85 years of age with a prostate-specific antigen (PSA) level between 0.3 ng/mL and 21.0 ng/mL and an imaging finding with Prostate Imaging-Reporting and Data System (PI-RADS) category between 2 and 5. Patients with indeterminate biopsy results were excluded, as were those for whom PSA values were missing, those who did not undergo microvascular Doppler assessment, and those previously diagnosed with prostate cancer. In each case, we performed systematic 10-core transrectal biopsy, guided by 1.5-T magnetic resonance imaging–ultrasound fusion, as well as performing Doppler ultrasound with microvascular flow imaging. Vascularization was qualitatively assessed and categorized as absent/minimal, moderate, or marked. The Gleason score was classified as clinically significant (≥ 7) or not (≤ 6)..
RESULTS: A significant association was found between the degree of microvascular flow and the Gleason score (p = 0.0384). Spearman's correlation was moderate (r = 0.377), and Kendall's tau was 0.300, indicating a positive relationship between higher microvascular flow and greater tumor aggressiveness.
CONCLUSION: Microvascular Doppler shows potential as a complementary tool in prostate biopsy, enabling more precise targeting of regions with increased vascularity, which might be associated with greater tumor aggressiveness.
Keywords: Prostatic neoplasms; Ultrasonography, Doppler; Neoplasm grading; Biopsy, needle; Neoplasms/diagnosis.
RESUMO
OBJETIVO: Avaliar se há correlação entre o grau de fluxo microvascular ao Doppler e a agressividade do câncer de próstata definida pelo escore de Gleason.
MATERIAIS E MÉTODOS: Estudo de coorte prospectivo com 88 pacientes entre novembro de 2023 e julho de 2024. Foram incluídos homens entre 48 e 85 anos, com PSA entre 0,3 e 21 ng/mL e laudos PI-RADS 2 a 5. Excluíram-se pacientes com biópsia indeterminada, PSA ausente, sem Doppler microvascular ou com diagnóstico prévio de câncer de próstata. Realizou-se biópsia transretal sistemática com 10 fragmentos, guiada por fusão com ressonância magnética (1,5-T) e ultrassonografia com Doppler de fluxo microvascular. A vascularização foi avaliada qualitativamente e o fluxo foi categorizado como ausente/mínimo, moderado ou acentuado. O escore de Gleason foi classificado como clinicamente significativo (≥ 7) ou não significativo (≤ 6).
RESULTADOS: Houve associação significativa entre o grau de fluxo microvascular e o escore de Gleason (p = 0,0384). A correlação de Spearman foi moderada (r = 0,377) e o tau de Kendall foi de 0,300, indicando relação positiva entre maior grau de fluxo e maior agressividade tumoral.
CONCLUSÃO: O Doppler microvascular demonstrou potencial como ferramenta complementar à biópsia prostática, permitindo direcionamento mais preciso para regiões com maior vascularização, possivelmente associadas a tumores mais agressivos.
Palavras-chave: Neoplasias da próstata; Ultrassonografia Doppler; Gradação de tumores; Biópsia por agulha; Neoplasias/diagnóstico.
INTRODUCTION
Prostate cancer (PCa) became the second leading cause of cancer-related death among adult men worldwide in 2022(1). In Brazil, it was responsible for 16,429 deaths that same year(2), whereas 31,620 PCa-related deaths were recorded in the United States in 2019(3).
Currently, prostate-specific antigen (PSA) testing and digital rectal examination are recommended for PCa screening. Magnetic resonance imaging (MRI) techniques are also employed to differentiate cancerous from non-cancerous tissues, improving diagnostic accuracy(4,5).
Transrectal ultrasound-guided biopsy remains a cost-effective and widely available diagnostic technique. New ultrasonographic techniques, such as microvascular flow (MVF) imaging, enable detailed visualization of blood flow in small vessels—particularly in areas around and including tumors, which tend to be more vascularized(6). Evidence suggests that such vascular patterns are also associated with tumor aggressiveness in renal, hepatic, and cervical cancer(7–9).
The objective of this study was to determine whether the degree of MVF on Doppler ultrasound correlates with the aggressiveness of PCa, as defined by the Gleason score.
MATERIALS AND METHODS
This was a prospective cohort study with non-randomized exposure categorization, conducted in the city of Campinas, Brazil, from November 2023 to July 2024. A total of 88 patients were eligible for inclusion. Patients were included if they me the following criteria: being a male; being 48–85 years of age; having a PSA level between 0.3 ng/mL and 21.0 ng/mL; and having an imaging finding assigned a Prostate Imaging-Reporting and Data System (PI-RADS) category between 2 and 5. Patients with indeterminate biopsy results were excluded, as were those for whom PSA values were missing, those who did not undergo microvascular Doppler assessment, and those previously diagnosed with PCa. Thus, 21 patients were excluded. Therefore, the final sample comprised 67 patients.
Procedure
Patients were placed in the left lateral position under anesthesia. Systematic biopsy was performed with 10 cores using an 18-G tru-cut needle via the transrectal route. The MRI scans (minimum 1.5-T) were fused with real-time ultrasound images acquired by using a high-resolution ultrasound system (RS85 Prestige; Samsung Medison Co Ltd, Seoul, South Korea). Microvascular Doppler ultrasound was applied to the MRI-identified suspicious area (Figure 1). All procedures were performed by an operator with over 15 years of experience.
Received in
July 9 2025.
Accepted em
September 20 2025.
Publish in
November 28 2025.
