
 |
|
Luciana Paula Benício Arcasa; Felipe Carlos Dias Arcasb; Laís Regiane da Silva Concilioc; Marina Amarald
DOI: 10.1590/0100-3984.2024.0089
e20240089
Publish in: July 25 2025
INTRODUCTION
Temporomandibular disorders (TMDs) encompass two major groups of conditions: those that affect the joint and those that affect the muscles. The maximum mouth opening is one of the parameters employed to assess adequate function and is a diagnostic indicator of a TMD(1). In joint-related TMDs, limited mouth opening can be associated with disc displacement without reduction, whereas it can be due to pain or fear of pain in muscle-related TMDs.
The main complementary examination for the evaluation of joint disorders is magnetic resonance imaging (MRI), which is the gold-standard imaging examination for the evaluation of TMDs. Joint dynamics should be evaluated at different degrees of mouth opening(2,3). However, keeping the mouth of a patient sufficiently open during the MRI examination can be challenging, and inappropriate management can hinder the diagnosis.
STATE OF THE TECHNIQUE
In joint-related TMDs, internal disorders of the temporomandibular joint (TMJ) are classified according to the Diagnostic Criteria for Temporomandibular Disorders as follows(4): disc displacement with reduction (DD+R); DD+R with intermittent locking; disc displacement without reduction (DDwoR); DDwoR with limited mouth opening (DDwoR+L); and DDwoR without limited mouth opening. Although DD+R is the most common disc disorder of the TMJ, DDwoR+L has been associated with major, irreversible damage to the TMJ.
In the TMJ, DDwoR+L can trigger pain and degenerative processes. Degenerative processes have been shown to be 60% more common in young patients with DDwoR+L than in those without limited mouth opening(5). In children, the increased risk of degeneration is even more critical, making early diagnosis and treatment imperative(6).
Of treatment-seeking patients, approximately 65% have joint-related and muscle-related conditions, 5% have only joint-related TMD, 13% have only muscle-related TMD, and the remainder have another condition(7). For evaluating TMJs, MRI is the imaging examination of choice and, according to the Diagnostic Criteria for Temporomandibular Disorders, should be performed to confirm clinical diagnoses. Soft and hard joint tissues, as well as the dynamics of joint movement, can be evaluated by MRI in different weightings (T1, proton density, and T2 with fat suppression), with the mouth closed, half-open, or open(8). However, in several situations, such as myalgia, because of pain or fear of pain, the patient often does not open their mouth correctly, making it difficult to arrive at an accurate diagnosis.
The examination is currently performed with devices of pre-established sizes or disposable syringes to keep the mouth open during the examination. However, in addition to causing patient discomfort, the lack of standardization can compromise the quality of the results, making it impossible to reproduce them, which would be of great value for follow-up, and generating uncertainty regarding the maximum mouth opening during the procedure.
Proposed device
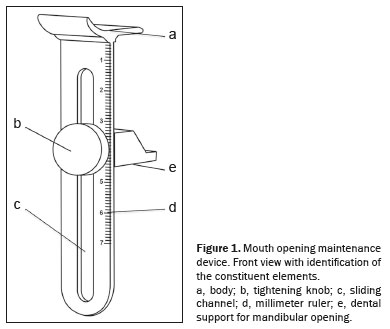
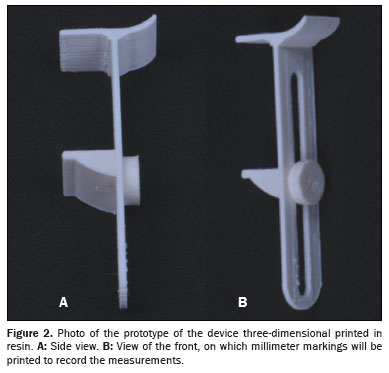
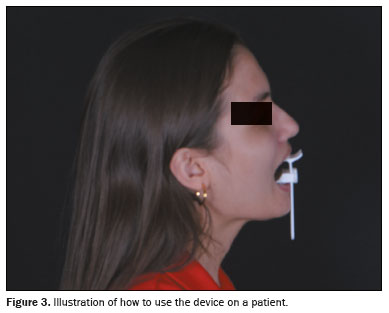
Figure 1 illustrates the proposed device, consisting of the body (a) with a tightening knob (b) that moves through a channel (c) to be adjusted to the mouth opening selected by the professional, guided by a lateral millimeter ruler (d) and a support for mandibular opening inserted between the teeth (e). This device can be used as a sliding caliper to measure the range of mouth opening with the lateral ruler, and these characteristics make it easy to use without the need for specific training. Figure 2 shows a prototype of the device, three-dimensional printed in resin, for an initial evaluation. Figure 3 shows how the proposed device is used in order to measure mouth opening and keep the mouth open during an MRI examination.
Received in
February 28 2025.
Accepted em
April 28 2025.
Publish in
July 25 2025.
