ABSTRACT
A typical approach for many cardiovascular surgical procedures is median sternotomy. Despite advances in surgical techniques and postoperative care, complications still occur in 0.5–5.0% of cases. Radiological assessment of the chest after sternotomy is a challenge, because normal findings resulting from surgical trauma can resemble complications. This pictorial essay aims to provide an overview of normal postoperative imaging findings and the spectrum of complications that can arise, including surgical material-related issues, hematomas, bone complications, and infections. Diagnosis and management require careful interpretation of imaging studies, considering the recovery timeline and clinical status of the patient. With the increasing number of cardiothoracic surgical procedures, this is essential knowledge for radiologists, allowing them to contribute to an accurate diagnosis and the appropriate management of patients.
Keywords:
Sternotomy; Postoperative complications; Diagnostic imaging; Mediastinitis; Surgical wound infection.
RESUMO
Uma abordagem típica para muitas cirurgias cardiovasculares é a esternotomia mediana. Mesmo com os avanços nas técnicas cirúrgicas e nos cuidados pós-operatórios, complicações ainda ocorrem em 0,5–5% dos casos. A avaliação radiológica do tórax após esternotomia é um desafio, pois os achados normais decorrentes do trauma cirúrgico podem se assemelhar a complicações. Este ensaio iconográfico tem como objetivo fornecer uma visão geral dos achados normais de imagem no pós-operatório e do espectro de complicações que podem surgir, incluindo complicações relacionadas a materiais cirúrgicos, hematomas, complicações ósseas e infecções. O diagnóstico e o manejo requerem uma interpretação cuidadosa dos estudos de imagem, considerando o tempo de recuperação do paciente e seu estado clínico. Com o aumento do número de procedimentos cirúrgicos cardiotorácicos, este é um conhecimento essencial aos radiologistas, para que possam contribuir para um diagnóstico adequado e o manejo correto dos pacientes.
Palavras-chave:
Esternotomia; Complicações pós-operatórias; Diagnóstico por imagem; Mediastinite; Infecção da ferida cirúrgica.
INTRODUCTION
Median sternotomy is the standard surgical approach for various cardiovascular conditions. Despite advances in surgical techniques and postoperative care, complications occur in 0.5–5.0% of cases. Such complications fall into four main categories: surgical material-related complications; hematoma; bone complications; and infections. Because clinical symptoms are frequently nonspecific, imaging is crucial for the postoperative evaluation and detection of these complications(1,2). This pictorial essay aims to depict the normal imaging appearance and the main complications following median sternotomy.
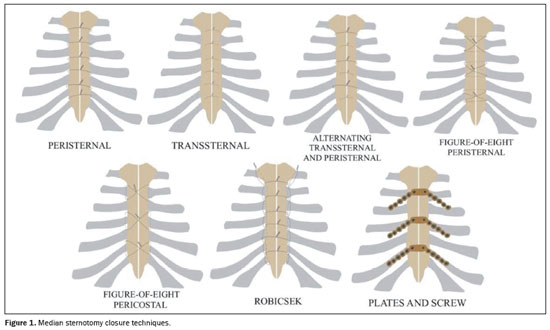
STERNOTOMY CLOSURE TECHNIQUES
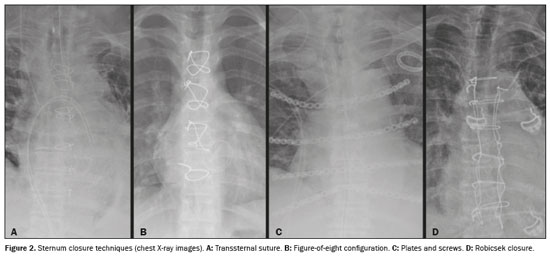
For sternotomy closure, two configurations—the transsternal–peristernal; and the single transsternal—are commonly used for their stiffness, ease of revision, and cost-effectiveness. However, they carry risks like wire fracture and pose challenges in cases involving osteoporotic bone. For revision sternotomy or in patients with osteoporosis, the Robicsek procedure may be applied, providing stability by reinforcing lateral portions of the sternum. The figure-of-eight configuration is another option for sternal closure. In patients at high risk for mediastinitis, plates and screws offer more rigid fixation(1–3), as illustrated in Figures 1 and 2.
Interpreting imaging studies in the first 2–3 weeks after sternotomy is challenging because normal healing findings can resemble complications like mediastinitis. Such findings include the following (Figure 3): edema (fat stranding); hypodense (fluid) or hyperdense (blood) accumulations in the presternal or retrosternal compartments; pneumomediastinum; and sternal separation. A pneumomediastinum should be reabsorbed within 1–2 weeks, while edema and fluid or blood accumulations usually resolve within 2–3 weeks. Sternal gaps of up to 4 mm can persist for up to 12 months without indicating sternal non-union, and callus formation can begin in postoperative month 3
(1,4).
FINDINGS OF POSTOPERATIVE COMPLICATIONS
Surgical material-related complications
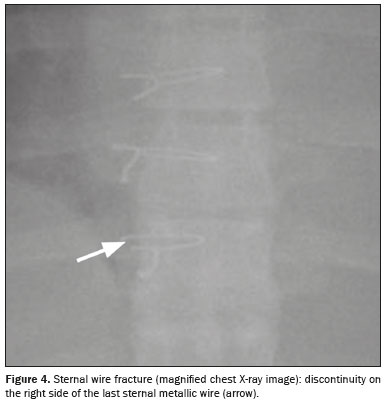
Sternal wire fracture – Sternal wire fractures have an estimated incidence of 2–3%. They are identified on radiographs as a focal defect (Figure 4). If there is uncertainty, a computed tomography (CT) scan may be performed
(1).
Sternal wire migration and dehiscence – In sternal wire migration, wires remain intact, with radiographs showing lateral displacement. Dehiscence involves sternal separation, with intact sternal wires migrating along with the displaced sternal fragment, typically within 1–40 days after surgery, with an incidence of 1–3%. This may lead to serious complications, including infection and wire displacement towards the aorta. Risk factors include age > 60 years, osteopenia, postoperative infection, and diabetes. Radiographic findings may precede the clinical diagnosis by 3–6 days, and lateral displacement (of 2 cm on average) of two or more sternal wires is usually observed in cases of sternal dehiscence (Figure 5). In some cases, a midsternal lucent stripe thicker than 3 mm is seen. Because X-rays offer limited bone assessment, CT may be necessary
(1,2,5).
Gossypiboma – Intrathoracic gossypiboma refers to a foreign object, like a mass of cotton matrix or a sponge, left within the thoracic cavity during surgery, surrounded by a foreign body reaction. Patients may be asymptomatic or present with chest pain, cough, dyspnea, or hemoptysis. On CT, a gossypiboma typically appears as a homogeneous or, more commonly, heterogeneous, rounded or oval mass with regular contours, with or without peripheral enhancement (Figure 6). Other potential imaging features include a wrinkled appearance, hyperdense linear image (radiopaque marker), spongiform appearance, and areas of high and low attenuation
(6).
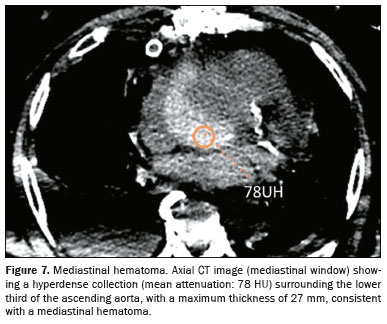
HematomaHematomas usually occur in the early postoperative period after median sternotomy, developing in the prevascular mediastinum or chest wall. The pathophysiological mechanism is multifactorial. Operations on large vascular structures, traumatic sternal fracture, increased intrathoracic pressure, anticoagulation, and other factors may be implicated. On CT, hematomas usually correspond to well-circumscribed hyperdense collections (Figure 7). Surgical re-exploration may be required in cases of significant bleeding, rapid expansion, or a significant mass effect
(1,2).
Bone complications
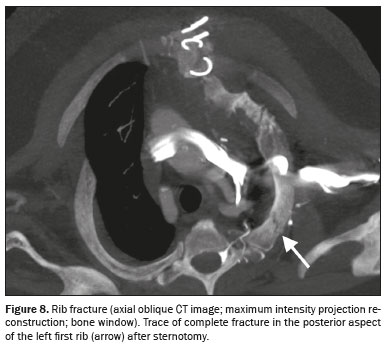
Fractures – Bone fractures occur in up to 13% of patients, usually involving the posterior portion of the 1st or 2nd ribs (Figure 8), and are associated with excessive intraoperative retraction and obesity. Cartilaginous fractures can also occur
(1).
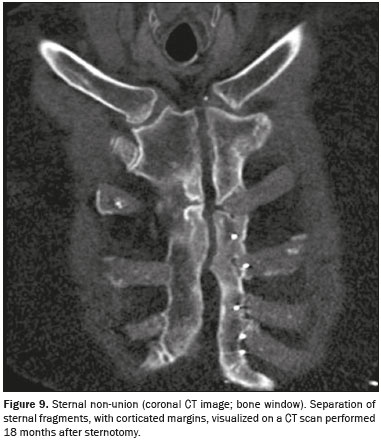
Sternal non-union – Sternal non-union (with an incidence of 0.5–3.0%) is defined as the failure of sternal fragments to fuse. Risk factors include osteoporosis, chest irradiation, corticosteroid use, obesity, and internal mammary artery harvest
(1). Clinically, it presents with a “clicking” sound and more than 3 months of sternal instability without associated infection. On CT, a sternal gap can be seen to have well-corticated edges
(2), as shown in Figure 9. Transverse fractures and floating bone fragments may also be seen. Up to 50% of patients show a sternal gap within the first six months post-sternotomy, which is not indicative of a pathological process. Therefore, in the absence of symptoms, a diagnosis of sternal non-union should be considered only > 12 months after sternotomy
(1).
Infections
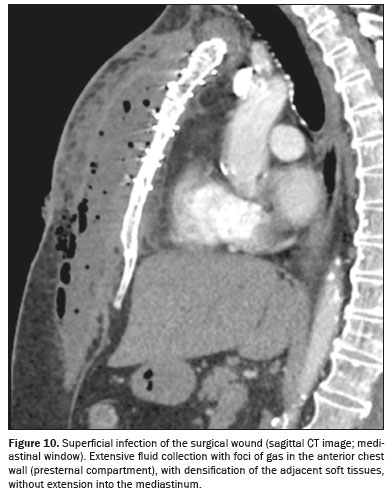
Superficial infection – Superficial wound infection (with an incidence of 0.5–8.0%) involves the skin, subcutaneous tissue, and pectoralis fascia. Symptoms include erythema, fever, purulent drainage, and sternal instability. A CT scan can reveal subcutaneous emphysema, fat stranding, and fluid collections limited to the chest wall (Figure 10). Treatment involves intravenous injection of antibiotics and local care
(7–10).
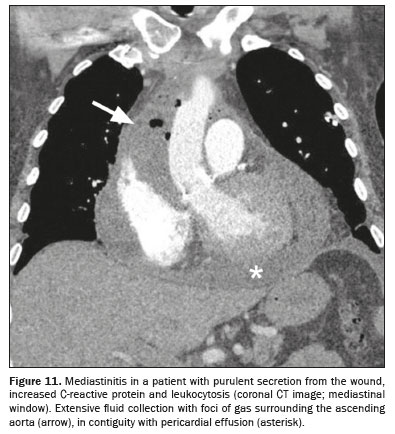
MediastinitisMediastinitis, which has an incidence of 0.4–5.0%, is a potentially fatal complication, associated with a mortality rate of 12–50%
(8). Risk factors include diabetes, obesity, excessive cauterization, prolonged surgery, and internal mammary artery harvest
(1). When there is suspicion of early mediastinitis (within the first 2–3 weeks), the clinical manifestation is crucial, given that CT may be inconclusive during this period, with normal postoperative findings resembling pathological ones. Signs and symptoms include fever, leukocytosis, sternal pain/instability, and purulent drainage
(9). After 21 days, CT findings such as mediastinal fluid collections (including complex fluid collections), mediastinal fat densification, and pneumomediastinum (Figure 11) become more specific for the diagnosis of mediastinitis
(4). Other signs include sternal diastasis, osteomyelitis, mediastinal lymphadenopathy, pleural/pericardial effusion, and pulmonary consolidation
(8–10). Management involves surgery and long-term antibiotic use
(1).
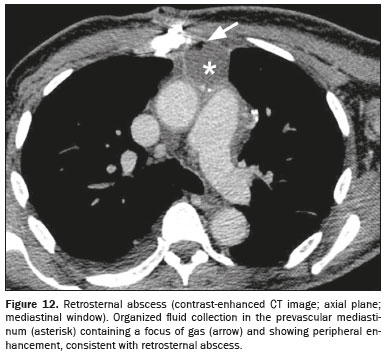
Retrosternal abscessRetrosternal abscess is defined as an infected encapsulated fluid collection in the prevascular mediastinum that arises weeks (or months) after sternotomy. It occurs due to hematogenous spread or contiguity.
Staphylococcus spp. are the most common pathogens. On CT, it appears as a hypodense fluid collection with thick or irregular peripheral enhancement and adjacent fat stranding, with or without foci of gas (Figure 12). Fistulous tracts to the skin, pericardium, or pleura may develop. In case of uncertainty, percutaneous needle aspiration may be performed to differentiate an abscess from a sterile postoperative seroma or hematoma. Definitive treatment often requires surgical exploration and drainage
(1,2).
OsteomyelitisPost-sternotomy osteomyelitis is a serious complication, with an incidence of 0.5–5.0% and an associated mortality rate of up to 29%, that may arise weeks, months, or years after the surgery.
Staphylococcus spp. are the main causative agents
(1,2). In the recent postoperative period, the diagnosis is challenging because of the usual sternal irregularities caused by surgical manipulation
(2). Findings on CT include bone erosion/sclerosis, periosteal reaction, and cortical destruction (Figure 13). Sequestrum, involucrum, abscess, and sinus tract formation may also occur. Osteomyelitis is often associated with sternal wound dehiscence or sternal non-union. Magnetic resonance imaging is the gold standard imaging modality for the diagnosis of osteomyelitis, enabling the detection of pathological bone marrow signal intensity, which includes hypointensity on T1-weighted images and hyperintensity on T2-weighted images (Figure 14), although its effectiveness can be limited by metal artifacts. Serial CT scans, in conjunction with the clinical and laboratory status of the patient, are often useful for diagnosis. Treatment includes antibiotics, drainage of collections, debridement of necrotic tissue, removal of infected sternal hardware, negative-pressure wound therapy, and chest wall reconstruction
(1,2).
CONCLUSIONRadiological evaluation of the chest after sternotomy is challenging for radiologists because normal findings due to surgical trauma can resemble complications. The image interpretation should take into consideration the recovery timelines (Figure 15), as well as the clinical and laboratory status of the patient. This approach is essential to achieve an accurate diagnosis and to inform decisions regarding the appropriate management of post-sternotomy complications.
REFERENCES1. Hota P, Dass C, Erkmen C, et al. Poststernotomy complications: a multimodal review of normal and abnormal postoperative imaging findings. AJR Am J Roentgenol. 2018;211:1194–205.
2. Young A, Goga U, Aktuerk D, et al. A radiologist’s guide to median sternotomy. Clin Radiol. 2024;79:33–40.
3. Raman J, Song DH, Bolotin G, et al. Sternal closure with titanium plate fixation—a paradigm shift in preventing mediastinitis. Interact Cardiovasc Thorac Surg. 2006;5:336–9.
4. Yamashiro T, Kamiya H, Murayama S, et al. Infectious mediastinitis after cardiovascular surgery: role of computed tomography. Radiat Med. 2008;26:343–7.
5. Dell’Amore A, Congiu S, Campisi A, et al. Sternal reconstruction after post-sternotomy dehiscence and mediastinitis. Indian J Thorac Cardiovasc Surg. 2020;36:388–96.
6. Machado DM, Zanetti G, Araujo Neto CA, et al. Thoracic textilomas: CT findings. J Bras Pneumol. 2014;40:535–42.
7. Singh K, Anderson E, Harper JG. Overview and management of sternal wound infection. Semin Plast Surg. 2011;25:25–33.
8. Siciliano RF, Medina ACR, Bittencourt MS, et al. Derivation and validation of an early diagnostic score for mediastinitis after cardiothoracic surgery. Int J Infect Dis. 2020;90:201–5.
9. Macedo CA, Baena MES, Uezumi KK, et al. Acute mediastinitis: multidetector computed tomography findings following cardiac surgery. Radiol Bras. 2008;41:269–73.
10. Jolles H, Henry DA, Roberson JP, et al. Mediastinitis following median sternotomy: CT findings. Radiology. 1996;201:463–6.
BP Medicina Diagnóstica, Hospital Beneficência Portuguesa de São Paulo, São Paulo, SP, Brazil
a.
https://orcid.org/0000-0003-4846-2602 b.
https://orcid.org/0000-0001-8768-8204 c.
https://orcid.org/0009-0005-0458-7579 d.
https://orcid.org/0000-0003-0886-5394Correspondence: Dr. Bruno Lima Moreira
Rua Maestro Cardim, 476, ap. 12, Bela Vista
São Paulo, SP, Brazil, 01323-000
Email:
limamoreiramed@gmail.com
Received in
August 21 2024.
Accepted em
November 12 2024.
Publish in
February 6 2025.

 |
|