Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 3 - May / June of 2009
Vol. 42 nº 3 - May / June of 2009
|
CASE REPORT
|
|
Venous aneurysm at the splenomesenteric confluence at the level of portal vein emergence: a case report |
|
|
Autho(rs): Mário Müller Lorenzato, Enrico Granzotto, André Della Barba Barros, Natasha Zacharias Arruda Silveira, Pedro Henrique Raffa de Souza |
|
|
Keywords: Aneurysm, Portal vein, Splenic vein, Mesenteric veins |
|
|
Abstract:
ITitular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MD, Radiologist at Documenta Clínica Radiológica, Ribeirão Preto, SP, Brazil
INTRODUCTION Aneurysms at the splenoportomesenteric junction constitute a rare clinical entity, with a case of splenic vein aneurysm being first described in the literature in 1953 by Lowenthal & Jacob(1). Only 40 cases have been described to date. Aneurysms etiology still remains unknown, and their origin may be congenital or acquired(2). This entity may be asymptomatic or can lead to severe conditions such as colicky abdominal pain, jaundice and digestive bleeding secondary to portal hypertension. Chronic liver disease, portal hypertension, trauma or inflammation constitute contributing factors in cases of secondary aneurysms(2,3). Vessel wall weakening due to trauma, inflammatory conditions such as pancreatitis or local degenerative alterations have also been implicated in the genesis of splenic vein dilatation. The diagnosis is usually achieved by B-mode or color Doppler ultrasonography, computed tomography and magnetic resonance imaging. Invasive procedures such as venous phase mesenteric arteriography or splenoportography may aid the diagnosis(4).
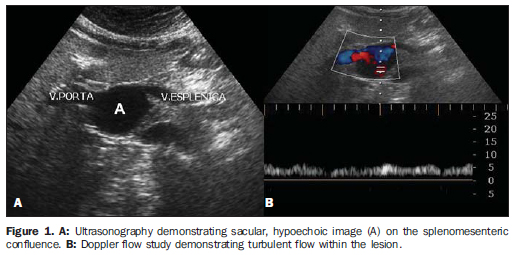
CASE REPORT A female, caucasian, 62-year-old patient coming from Ribeirão Preto, SP, Brazil, with diabetes mellitus was referred for investigation of abdominal mesogastric pain by ultrasonography and later by computed tomography. At ultrasonography, a sacular, hypo-echoic image was observed in the splenomesenteric junction. Doppler flow study demonstrated a venous pattern of the blood flow and turbulent venous flow within the lesion (Figure 1).
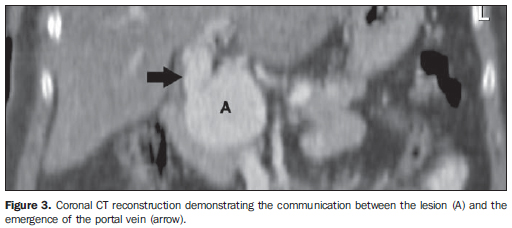
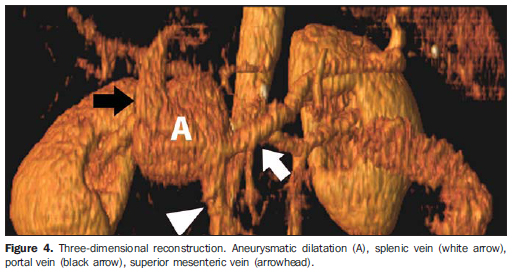
With the progress of the investigation, the patient underwent computed tomography scan that demonstrated a 5.2 × 4.0 cm round-shaped formation in the confluence of the splenic and superior mesenteric veins at the level of the portal vein emergence, with vascular pattern enhancement. This mass caused compression over the pancreatic head, inferior vena cava and right renal vein (Figures 2, 3 and 4).
Clinical evaluation ruled out portal hypertension, hepatopathies or jaundice as clinical or laboratory findings, thus a cause for these alterations has not been found.
DISCUSSION Venous aneurysms are atypical malformations rarely found in the usual clinical practice. Most of times, these lesions are located in the cervical region and lower limbs(5); and among visceral aneurysms, those affecting the portal venous system are the most frequently found(4,6,7). The etiology of splenoportomesenteric confluence aneurysms still remains unknown, and congenital and acquired causes such as portal hypertension, cirrhosis, inflammation, arteriovenous fistulas and previous trauma have been postulated for this abnormality(2,4,7). However, not all the patients with portal hypertension develop aneurysmatic dilatations, so it seems there may be a multifactorial mechanism of action. With regard to clinical manifestations, most splenic vein aneurysms are asymptomatic, constituting incidental findings in abdominal investigations(4). The natural history and behavior of splenoportomesenteric axis aneurysms still remain unknown. Complications such as rupture, thrombosis, compression of adjacent structures and gastrointestinal bleeding secondary to esophageal varices have been described in the literature.
CONCLUSION Splenoportomesenteric axis aneurysms have been already considered extremely rare, but currently constitute a well documented clinical entity, although representing only 3% of the cases of venous system aneurysms(8). The diagnosis can be achieved by color Doppler study demonstrating the venous flow within the aneurysmatic cavity, except in the case of thrombosis. Contrast-enhanced helical computed tomography, besides providing information on the mass and adjacent structures, can offer three-dimensional images, allowing an accurate diagnosis(9). The choice of conservative or surgical management depends on several factors. For the majority of authors, in cases of portal hypertension, the most appropriate treatment seems to be the placement of a portosystemic shunt(4). Controversy emerges in cases where portal hypertension is not present. In the present case, the gastric surgeon decided for an expectant strategy, with periodic imaging follow-up, considering that the patient presented intermittent clinical signs, without any other findings.
REFERENCES 1. Lowenthal M, Jacob H. Aneurysm of splenic vein. Report of a case. Acta Med Orient. 1953;12:170-4. [ ] 2. Barzilai R, Kleckner MS Jr. Hemocholecyst following ruptured aneurysm of portal vein: report of a case. AMA Arch Surg. 1956;72:725-7. [ ] 3. Glazer S, Gaspar MR, Esposito V, et al. Extrahepatic portal vein aneurysm: report of a case treated by thrombectomy and aneurysmorraphy. Ann Vasc Surg. 1992;6:338-43. [ ] 4. Bernal C, Ocaña J, Gandarias C, et al. Aneurismas de la vena esplénica. A propósito de un caso y revisión de la literatura. Angiología. 2001;53: 28-32. [ ] 5. Calligaro KD, Ahmad S, Dandora R, et al. Venous aneurysms: surgical indications and review of the literature. Surgery. 1995;117:1-6. [ ] 6. Fulcher A, Turner M. Aneurysms of the portal vein and superior mesenteric vein. Abdom Imaging. 1997;22:287-92. [ ] 7. Brock PA, Jordan PH Jr, Barth MH, et al. Portal vein aneurysm: a rare but important vascular condition. Surgery. 1997;121:105-8. [ ] 8. Gallego C, Velasco M, Marcuello P, et al. Congenital and acquired anomalies of the portal venous system. Radiographics. 2002;22:141-59. [ ] 9. Pinto OL, Tornin OS, Botelho RA, et al. Aneurisma de artéria hepática simulando lesão em cabeça de pâncreas: relato de caso. Radiol Bras. 2005;38:467-70. [ ] Received August 30, 2007. * Study developed at Documenta Clínica Radiológica, Ribeirão Preto, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554