Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 3 - May / June of 2009
Vol. 42 nº 3 - May / June of 2009
|
ORIGINAL ARTICLE
|
|
Radiomorphological study of the peroneus longus tendon adjacent to the cuboid bone |
|
|
Autho(rs): Carlos Eduardo Affonso Grinbaum, Antonio Vitor de Abreu, Rodrigo Oliveira Carvalho de Aguiar, Emerson Leandro Gasparetto, Hilton Augusto Koch |
|
|
Keywords: Peroneus longus, Os peroneum, Sesamoid |
|
|
Abstract:
ISpecialist in Human Anatomy, Fellow Master degree, Faculdade de Medicina daUniversidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil
INTRODUCTION The peroneus longus muscle originates at the head and the upper two thirds of the lateral surface of the fibula body and inserts itself at the lateral face of the base of the first metatarsal and medial cuneiform, at the mid foot region(1). This muscle assists in the plantar flexion of the first radius forefoot pronation and eversion, and acts as a secondary plantar flexor of the ankle(2). Its tendon originates in the lower third of the leg, at the posterolateral region of the ankle, and runs around three bony prominences on its way to the foot: the first at the ankle, posterior to the lateral malleolus and the tendon of the peroneus brevis muscle; the second at the calcaneus, around the fibular tubercle; and the third, inferiorly to the cuboid bone. This last curve is sharper, with approximately 90º, changing its course from a vertical to a horizontal direction(3). Studies have demonstrated that tendons that change their course are more prone to injury, therefore morphologic adaptations are important to enable the body segment to withstand the compression and traction forces generated in these areas(4,5), like in the more distal curvature of the peroneus longus muscle. Another study even describes the presence of an incomplete synovial joint (without a disc) in this region, called fibulo-cuboid joint, separated from the tendinous sheath of the peroneus longus muscle(6). Additionally, the presence of fibrocartilaginous tissue within this portion of the tendon is described, with the possible presence of an accessory intratendineal ossicle, the os peroneum(3,4,7). The function and origin of this ossicle are controversial, as well as its incidence, that range from 2.3% to 90% among the authors(2-9). A research about anthropologic anatomy proposes that this ossicle is a remnant of early primates, and is losing its function in humans due to the bipedal posture(10). Meanwhile, some studies correlate this ossicle with an increased incidence of tendon-specific conditions(11-13). Thus, a better understanding of this tendinous portion of the peroneus longus is indeed necessary. The present study is aimed at describing the morphological aspects and radiographically evaluating the segment of the peroneus longus tendon adjacent to the cuboid bone, in cadavers, and reporting the incidence of a fibular ossicle, in some cases with the help of histological analysis.
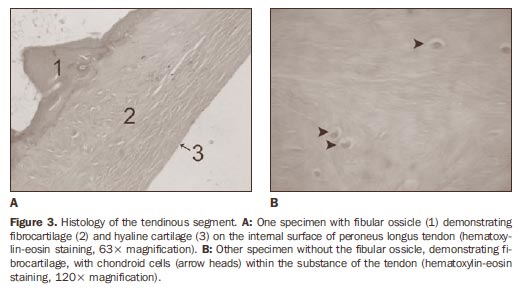
MATERIALS AND METHODS Fifty tendinous specimens measuring approximately 5 cm in length were collected from the fibulo-cuboid region of 50 cadaver feet (48 male and 2 female), with ages at death ranging from 20 to 70 years. The specimens were preserved in a 10% formalin solution. Tendons presenting tears or degeneration with a loss of > 50% in caliber at macroscopic inspection were excluded from the study. The research was developed with approval by the Committee for Ethics in Research of the institution. Radiographic study was performed in order to detect the presence of the ossicle in this tendinous segment. The tendons were grouped on x-ray film, with the surface adjacent to the cuboid bone turned upwards. The x-ray tube was positioned one meter away from the film, where the radiographs were taken. With these results, the tendons were divided into three groups: 1) tendons with fibular ossicle; 2) tendons without fibular ossicle; 3) doubtful cases where a poorly defined increase in density was observed, without a clear evidence of ossification. A longitudinal section of all the tendons were also macroscopically evaluated along their whole length. In the cases where the ossicle presence was doubtful, microscopic studies were performed with hematoxylin-eosin staining with 16, 63 and 120-fold magnification. Morphology, macro- and microscopic characteristics were analyzed and compared with the initial radiographic study. A parallel microscopic analysis was performed in one tendon with the fibular ossicle, in order to illustrate this fibulo-cuboid relation (see Figure 3).
RESULTS The harvested tendinous segments presented a macroscopic flat, spindle-shaped morphology, with internally concave and externally convex surfaces. Another morphological characteristic observed in all of the specimens was a tendinous dilatation, exactly in the passage at the groove of the cuboid bone, which measured approximately 3 cm in length, 2 cm in width and 1 cm in thickness (Figure 1). Radiographically, the ossicle was demonstrated in 13 tendons (26% - group 1), absence of ossification was observed in 29 (58% - group 2) and doubtful cases in 8 tendons (16% - group 3) (Figure 2). After macroscopic lon-gitudinal section in all groups, the results of previous radiographic analysis were confirmed for groups 1 and 2. However, in group 3, the absence of ossification was demonstrated in five cases, and presence in only one case. The doubt remained in two tendons, whose microscopic analysis demonstrated absence of ossification. The final result of the study demonstrated the presence of the fibular ossicle in 14 tendons (28%). In 36 tendons (72%) the accessory bone could not be visualized. During the histological study of these two doubtful tendons and one segment with the accessory ossicle, the presence of fibrocartilaginous tissue was identified in the segment. Chondrocytes and matrix associated with collagen fibers were also observed (Figure 3). The distal and proximal tendon stumps showed microscopic characteristics typical of tendinous tissue, but on the internal surface of the tendon, hyaline cartilage was demonstrated at histology.
DISCUSSION The peroneus longus tendon is exposed to trauma and degeneration, especially in the region where it bends around the cuboid bone(14,15). Anatomical adaptations, such as the formation of a focal fibrocartilaginous area(16) are important to reduce friction and to resist compression and traction forces(4). Compressive forces may be responsible for this type of tissue differentiation, replacing the healthy tendinous tissue for fibrocartilage, with production of proteoglycans that retain water, increasing the resistance of the tendon against external forces. Some studies have demonstrated that the tendon composition is variable in areas of change in direction, especially around bone structures, particularly in the peroneus longus around the cuboid bone(4,5). This fibrocartilaginous differentiation and mechanical forces may predispose to the development of ossification, and consequently, to the formation of a fibular ossicle(17). Studies about the fibular ossicle are not recent, defining this condition in the peroneus longus tendon as being a sesamoidtype bone(18). A morphological study has demonstrated the presence of fibrocartilaginous tissue in the fibular tendon adjacent to the cuboid bone that may ossify and become an ossicle(19). Testut & Latarget(16) have also mentioned this fibrocartilaginous structure susceptible to ossification. The reported incidence of fibular ossicle is variable, from 8.5% to 26% in anatomical re-search(8,20), and from 2.3% to 9% in radiological studies(7,8). In fact, part of the difference between the rates of incidence of fibular ossicle at radiological and morphological studies may be explained by sudden occurrence of calcification non-identifiable by radiography, or by less-than-optimal exposure, without inclusion of oblique view instead of dorsoplantar view (7). Oyedele et al. have demonstrated the presence of this accessory ossicle in 90% of South African specimens, by means of cadaver dissection, suggesting that environmental and ethnical factors may be associated with the incidence of this ossicle(9). Many authors agree that the presence of the fibular ossicle is actually not a mechanical advantage, and may indeed predispose the tendon to injury(11-13,21-24). The fibular ossicle may appear as a consequence of an intense friction between the tendon and the cuboid bone, inducing the ossification of the fibrocartilaginous tissue. A comparative study has speculated that this ossicle is a structure that is disappearing in humans, being present in 100% of the primates to facilitate the peroneus longus in the abduction of the hallux, important for the tweezer-like movement of the fingers in these species(10). Hyaline cartilage was found on the cuboid surface of the tendon in the cuboid groove, as reported by previous studies(4,6) and corroborated by the present study. Ebraheim et al. have described the presence of a separate synovial joint between the cuboid and the peroneus longus tendon, without communication with the tendinous sheath, called peroneal-cuboid joint(6). The present study evaluated only qualitative histological aspects of the peroneus longus tendon articular surface, and not the presence of such joint. The present study faced some limitations; in situ radiographic study could not be performed to correlate the incidence of the fibular ossicle with the dissected specimens. Also, the radiographic study could have been performed with mammographic films and equipment, the ideal combination to investigate small calcifications. Besides that, only two doubtful specimens were submitted to histological study. Finally, considering that the present study was developed with cadaver specimens, the loss of the previous clinical history as regards diseases on the lateral region of the feet may have affected the final results.
CONCLUSION All the specimens included in the present study demonstrated focal tendon thickening in the region of curvature under the cuboid. However, after quantitative analysis, of the two specimens submitted to histological study, it was observed that the tendon was composed of fibrocartilage, and covered by hyaline cartilage on the c surface adjacent to the cuboid bone. Thus, the fibular ossicle was observed in 26% (13/50) of the specimens on the radiological study, and in 28% (14/50) of the specimens morphologically evaluated (macroand microscopy). There was disagreement over one specimen that was doubtful on the radiological study and positive for the presence of the ossicle at macroscopic evaluation.
REFERENCES 1. Warwick R, Williams PL. Gray's Anatomy. 35th ed. Philadelphia: WB Saunders; 1973. [ ] 2. Brandes CB, Smith RW. Characterization of patients with primary peroneus longus tendinopathy: a review of twenty-two cases. Foot Ankle Int. 2000;21:462-8. [ ] 3. Sarrafian SK. Anatomy of the foot and ankle. Descriptive, topographic, functional. Philadelphia: Lippincott; 1983. [ ] 4. Benjamin M, Qin S, Ralphs JR. Fibrocartilage associated with human tendons and their pulleys. J Anat. 1995;187(Pt 3):625-33. [ ] 5. Benjamin M, Ralphs JR. Fibrocartilage in tendons and ligaments - an adaptation to compressive load. J Anat. 1998;193(Pt 4):481-94. [ ] 6. Ebraheim NA, Lu J, Haman SP, et al. Cartilage and synovium of the peroneocuboid joint: an anatomic and histological study. Foot Ankle Int. 1999;20:108-11. [ ] 7. Mellado JM, Ramos A, Salvadó E, et al. Accessory ossicles and sesamoid bones of the ankle and foot: imaging findings, clinical significance and differential diagnosis. Eur Radiol. 2003;13 Suppl 4:L164-77. [ ] 8. Clanton TO, Schon LC. Athletic injuries to the soft tissues of the foot and ankle. In: Mann RA, Coughlin MJ, editors. Surgery of the foot and ankle. 6th ed. London: Mosby; 1993. p. 1125-6. [ ] 9. Oyedele O, Maseko C, Mkasi N, et al. High incidence of the os peroneum in a cadaver sample in Johannesburg, South Africa: possible clinical implications? Clin Anat. 2006;19:605-10. [ ] 10. Le Minor JM. Comparative anatomy and significance of the sesamoid bone of the peroneus longus muscle (os peroneum). J Anat. 1987;151:85-99. [ ] 11. Brigido MK, Fessell DP, Jacobson JA, et al. Radiography and US of os peroneum fractures and associated peroneal tendon injuries: initial experience. Radiology. 2005;237:235-41. [ ] 12. Peacock KC, Resnick EJ, Thoder JJ. Fracture of the os peroneum with rupture of the peroneus longus tendon. A case report and review of the literature. Clin Orthop Relat Res. 1986;(202): 223-6. [ ] 13. Truong DT, Dussault RG, Kaplan PA. Fracture of the os peroneum and rupture of the peroneus longus tendon as a complication of diabetic neuropathy. Skeletal Radiol. 1995;24:626-8. [ ] 14. O'Donnell P, Saifuddin A. Cuboid oedema due to peroneus longus tendinopathy: a report of four cases. Skeletal Radiol. 2005;34:381-8. [ ] 15. Sammarco GJ. Peroneus longus tendon tears: acute and chronic. Foot Ankle Int. 1995;16:245-53. [ ] 16. Testut L, Latarjet A. Tratado de anatomía humana. Barcelona: Salvat; 1959. [ ] 17. Sarin VK, Carter DR. Mechanobiology and joint conformity regulate endochondral ossification of sesamoids. J Orthop Res. 2000;18:706-12. [ ] 18. Anatomical Society. Collective investigations, sesamoids in the gastrocnemius and peroneus longus. J Anat Physiol. 1897;32:182-6. [ ] 19. Schaeffer JP. Morris' Human anatomy. 11th ed. New York: The Blakiston Company; 1953. [ ] 20. Benninghoff G. Anatomia generale, anatomia speciale dell'apparato locomotore. In: Benninghoff G, Goerttler K, editors. Benninghoff-Goerttler Trattato di anatomia umana funzionale. Padova: Piccin Editore; 1978. p. 432-3. [ ] 21. Patterson MJ, Cox WK. Peroneus longus tendon rupture as a cause of chronic lateral ankle pain. Clin Orthop Relat Res. 1999;(365):163-6. [ ] 22. Rosenberg ZS, Beltran J, Bencardino JTM, et al. From the RSNA Refresher Courses. Radiological Society of North America. MR imaging of the ankle and foot. Radiographics. 2000;20 Spec No: S153-79. [ ] 23. Peterson JJ, Bancroft LW. Os peroneal fracture with associated peroneus longus tendinopathy. AJR Am J Roentgenol. 2001;177:257-8. [ ] 24. Dombek MF, Lamm BM, Saltrick K, et al. Peroneal tendon tears: a retrospective review. J Foot Ankle Surg. 2003;42:250-8. [ ] Received October 9, 2008. * Study developed at Universidade Federal do Rio de Janeiro dade de Medicina da Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. (UFRJ), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554