Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 1 - Jan. /Feb. of 2010
Vol. 43 nº 1 - Jan. /Feb. of 2010
|
CASE REPORT
|
|
Pseudotumoral mesenteric panniculitis: tomographic findings in a case |
|
|
Autho(rs): Eduardo Miranda Brandão, Thales Paulo Batista, Jonas José da Silva Júnior, Francisco Igor Bulcão de Macêdo, Paulo Henrique Domingues Miranda Brandão |
|
|
Keywords: Sclerosing mesenteritis, Mesenteric panniculitis, Pseudotumor, Pancreas |
|
|
Abstract:
IMaster in Surgery, Oncologist Surgeon, Professor in the Discipline of Oncology at Faculdade de Ciências Médicas - Universidade de Pernambuco (FCM-UPE), Recife, PE, Brazil
INTRODUCTION Mesenteric panniculitis is an inflammatory reaction of the mesentery pathologically characterized by different degrees of fat necrosis, chronic inflammatory infiltrate and proliferation of collagenous fibrous tissue. The clinical presentation is variable and only in few cases the disease presents in the form of abdominal pseudotumors(1). In such cases, the final diagnosis is based on laparotomy and histological confirmation, but presents a favorable prognosis and rarely leads to death. The present report is aimed at describing a rare case of mesenteric panniculitis that initially presented as a pseudotumor involving the peripancreatic region with emphasis to tomographic findings.
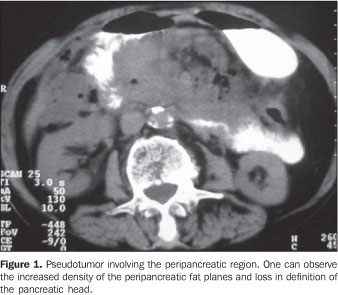
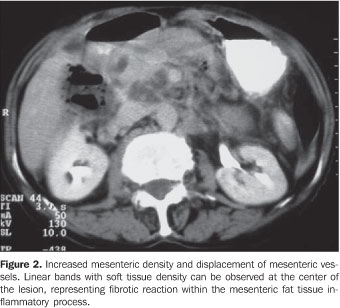
CASE REPORT A 73-year-old female patient initially diagnosed with abdominal tumor was referred for oncologic evaluation due to an intense and persistent epigastric pain in association with occasional nausea and vomiting for the past 30 days. Additionally, the patient reported recurrent and low fever, anorexia and a non-quantified weight loss. She also reported a similar, but less intense and self-limited event four months ago, however no significant comorbidity was observed. On physical examination, a 15 cm in diameter painful partially mobile, ill-defined epigastric tumor was palpated. Neither significant lymph nodes enlargement nor relevant findings were observed at gynecological and rectal examination. Abdominal ultrasound (US) showed an agglomeration of thickened intestinal loops in the left hypochondrium, besides an abdominal computed tomography (CT) study revealed increased density of peripancreatic fat planes with loss in the definition of the pancreatic head (5.2 × 4.9 × 3 cm) (Figure 1). Other findings, i.e densification of the mesentery and displacement of mesenteric vessels, besides thickening of intestinal loops and subtle ascites are showed on Figure 2.
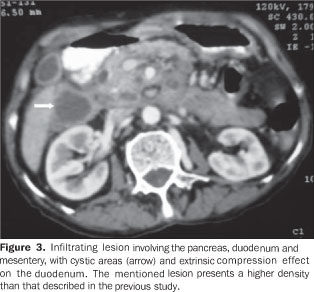
All laboratory tests including amylase and lipase measurements and tumor markers were within normal limits, i.e. CEA = 0.655 U/ml and CA19.9 = 21.3 U/ml. Upper digestive endoscopy demonstrated extrinsic compression of the second portion of the duodenum without mucosal involvement, while colonoscopy demonstrated a concentric, abrupt narrowing of the transverse colon near the splenic angle. The muscosa of this region presented hyperemia and was friable. Biopsy was performed during the examination. The attempt to collect a specimen for biopsy by means of percutaneous puncture was unsuccessful and while waiting for the biopsy to be performed the patient progressed with constipation, recurrent low fever, anorexia and vomiting in association with significant decrease in the volume of the abdominal mass at the daily clinical examinations. During the work-up serial amylase measurements remaided normal and a new CT was ordered and showed an ill-defined, infiltrating lesion located in the retroperitoneum and anterior pararenal space, involving the pancreas, duodenum and mesentery. Additionally, focal areas of liquefaction and involvement without invasion of mesenteric vessels, besides the effect of extrinsic compression on the duodenum were observed (Figure 3).
An exploratory laparotomy was performed and demonstrated a small amount of citrine fluid in the pelvis and a tumor-like fat accumulation with an intense edema in the mesenteric root. Also, there was a fibrotic involvement of the transverse mesocolon causing lumen stenosis in the region near the splenic angle, and periduodenal fibrotic reaction with bridles to the parietal peritoneum of the right hypochondrium. After the opening of the epiploon retrocavity and subsequent Kocher-Vautrin and Cattell-Braasch maneuvers, the normal macroscopic aspect of the whole pancreas could be observed. Lysis of the bridles and adhesions were performed to clear the transverse colon lumen, with abdominal fluid drainage and freezing biopsy of the mesenteric tumor-like lesion which demonstrated an inflammatory and fibrotic component with no neoplastic involvement. The patient was given antibiotics for 48 hours and symptomatic medication for five additional days, with progressive improvement. She was discharged at the day 32 (5th postoperative day) and remains asymptomatic after 12-month follow-up. Neither aerobic bacterial growth nor the presence of neoplastic cells was found at the abdominal fluid analysis. Histology of specimens taken during colonoscopy demonstrated only an inflammatory infiltrate mimicking a mild chronic colitis. Finally, the biopsy of the mesenteric tumor-like lesion described a miscellaneous fat necrosis, chronic inflammatory infiltrate and different degrees of fibrosis in the several samples.
DISCUSSION Mesenteric panniculitis represents a rare, non-specific inflammatory reaction of the mesentery whose etiology still remains unknown. Only in few cases, the disease presents in the form of abdominal pseudo-tumors(1,2). Histologically, mesenteric lipodystrophy, mesenteric panniculitis and retractile mesenteritis have been considered as progressive stages of a single mesenteric inflammatory and non-specific process, characterized by a mix of variable degrees of fat necrosis, chronic inflammatory infiltrate and fibrosis(1-3). These three main terms characterize the predominance of each of such components, respectively, in the different phases of the disease. However, considering that a certain degree of these three components is found in all of the cases, considering their progressive character for mesenteric fibrosis, the term "sclerosing mesenteritis" is generically considered as most appropriate(1,3). The most frequent clinical findings include pain and abdominal mass(1,2), generally in association with other non-specific, constitutional signs and symptoms(2). Laboratory and sonographic findings are equally non-specific(1,2). Barium studies demonstrate only indirect signs of parietal involvement with preserved mucosal pattern. On the other hand, computed tomography presents a good anatomopathological correlation and is frequently employed in the diagnosis and follow-up of these cases. Also, magnetic resonance imaging presents additional benefits because of the better characterization of tissues and non-invasiveness in the evaluation of small-caliber vessels(2), which can also be achieved with multi-detector computed tomography with intravenous contrast injected by an infusion pump. The main findings in the tomographic evaluation of mesenteric panniculitis are the following: presence of heterogeneous mass with thickened fat density, displacement and ectasia of mesenteric vessels, intestinal loops distortion and presence of a tumor pseudocapsule. Other findings include increased mesenteric density, cysts development, fat ring sign, calcifications and lymph nodes enlargement(1,2,4,5). Mesenteric panniculitis can be satisfactorily studied with abdominal CT as method of choice(4), the findings depending on the disease stage(2). At the acute and subacute phases of lipodystrophy and panniculitis, there is a predominance of heterogeneous mass effect with a slightly increased fat density as a result of the inflammatory process, and without direct vessels involvement, besides development of linear bands resulting from the fibrotic retraction. On the other hand, at the chronic phase of the disease, such masses acquire a more homogeneous appearance and increased density typical of fibrotic reaction(2). The fat ring sign and the tumor pseudo-capsule represent the preservation of the fat adjacent to the mesenteric vessels and the development of peripheral bands with soft tissue density separating the healthy mesentery from the inflammatory process, respectively. Both strongly suggest the diagnosis of mesenteric panniculitis, however these findings tend to disappear with the progression of the fibrotic process(2). Furthermore, for the correct diagnosis of this disease, it is necessary to rule out the presence of pancreatitis, intestinal inflammatory disease and Weber-Christian disease(2). The differential diagnoses also must include Whipple's disease, carcinoid tumors, inflammatory paseudotumors, leiomyosarcoma, abscesses, hematomas, fatty neoplasms, mesenteric carcinomatosis, Non-Hodgkin lymphoma, retroperitoneal fibromatosis, secondary fibrosing peritonitis, mesenteric edema and other causes of intestinal obstruction(1-3) . Many treatment methods have been employed, but none of them have shown to be indistinctly appropriate(1,2,4,5). The role of surgery remains restricted to biopsies and management of complications(2). In most of cases, the patients progress with complete or partial resolution of the condition with the process stabilization, with very rare cases of fatal outcome(1-3). Considering the non-specific characteristics of this condition, the diagnosis of pseudotumoral mesenteric panniculitis requires laparotomy and biopsies for clinical, radiological, surgical and histological correlation(1,3). However, the knowledge of clinical and radiological characteristics can avoid unnecessary surgeries, considering the favorable clinical course of the disease in most of cases. In the present report, the appropriate correlation of clinical, radiological, surgical and histological findings has led to the diagnosis of mesenteric panniculitis with a tendency to progress to fibrosis where, except for the tumor pseudocapsule, all the mentioned tomographic findings were observed.
REFERENCES 1. Sheikh RA, Prindiville TP, Arenson D, et al. Sclerosing mesenteritis seen clinically as pancreatic pseudotumor: two cases and a review. Pancreas. 1999;18:316-21. [ ] 2. Moreira LBM, Pinheiro RA, Melo ASA, et al. Paniculite mesentérica: aspectos na tomografia computadorizada. Radiol Bras. 2001;34:135-40. [ ] 3. Emory TS, Monihan JM, Carr NJ, et al. Sclerosing mesenteritis, mesenteric panniculitis and mesenteric lipodystrophy: a single entity? Am J Surg Pathol. 1997;21:392-8. [ ] 4. Varela C, Fuentes M, Rivadeneira R. Procesos inflamatorios del tejido adiposo intraabdominal, causa no quirúrgica de dolor abdominal agudo: hallazgos en tomografía computada. Rev Chil Radiol. 2004;10:28-34. [ ] 5. Martínez Odriozola P, García Jiménez N, Cabeza García S, et al. Mesenteritis esclerosante. A propósito de dos casos con diferente forma de presentación clínica. An Med Interna (Madrid). 2003;20:254-6. [ ] Received February 20, 2008. * Study developed at the Center of Oncology of Hospital Universitário Oswaldo Cruz - Universidade de Pernambuco (CEON/HUOC-UPE), Recife, PE, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554