Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 2 - Mar. / Apr. of 2009
Vol. 42 nº 2 - Mar. / Apr. of 2009
|
ORIGINAL ARTICLE
|
|
Tomographic findings of lobar consolidation in primary pulmonary tuberculosis |
|
|
Autho(rs): Bruno Alberto Falcão Pereira, Solange Gonçalves David de Macêdo, Renata do Amaral Nogueira, Lola Celeste Pantoja Castiel, Cláudia Renata Rezende Penna |
|
|
Keywords: Pulmonary tuberculosis, Child, Computed tomography |
|
|
Abstract:
IPost-graduate in Radiology and Imaging Diagnosis by Santa Casa da Misericórdia do Rio de Janeiro, Rio de Janeiro, RJ, Brazil, MD, Resident at Hôpital Européen Georges Pompidou, Paris, France
INTRODUCTION Tuberculosis still remains as a relevant cause of morbi-mortality worldwide, particularly in developing countries. Children represent a risk group, especially those under the age of five(1-3). In this age range, the most frequent presentation of this condition is primary pulmonary tuberculosis, and most commonly radiological findings include: lymph node enlargement, parenchymal disease, atelectasis, pleural effusion and miliary disease(4,5). Establishing a diagnosis of primary pulmonary tuberculosis in children represents a challenging task for several reasons. Most of times, the patients are asymptomatic at the moment of the diagnosis, bacteriological confirmation is hardly achieved because of the difficulty the sputum collection, and positive gastric lavages are found in a small number of cases. Other relevant aspects to be taken into consideration in the diagnostic investigation are the following: epidemiological history of recent exposure to the bacillus, tuberculin test (PPD) and chest radiography(4,6,7). Chest computed tomography presents advantages over conventional radiography and can detect tuberculosis in patients with normal or equivocal chest radiographs(1). The present study is aimed at describing tomographic findings of primary pulmonary tuberculosis initially manifesting as lobar consolidation.
MATERIALS AND METHODS The present study was developed in the Hospital Municipal Jesus, a reference in pediatrics in the State of Rio de Janeiro, Brazil. In the period between 2002 and 2006, tomographic findings of four children in the age range between 3 and 14 months with primary pulmonary tuberculosis initially manifested as lobar consolidation were retrospectively evaluated. The children were clinically evaluated, with investigation of possible previous contact with tuberculosis, tuberculin test, culture of gastric and bronchoalveolar aspirates for tubercle bacillus and human immunodeficiency virus (HIV) serum test, besides imaging investigation. Chest radiography and computed tomography were requested as a diagnostic complementation for the clinical suspicion of pulmonary tuberculosis. The following aspects were analyzed on the computed tomography images: - Consolidation pattern (presence of cavitation, calcifications and hypodense areas compatible with caseous necrosis); - pattern and distribution of nodular opacities; - mediastinal or hilar lymphadenopathy, with or without the presence of central necrosis and/or peripheral calcification; - complications such as masslike effect, airway stenosis, atelectasis, pleural effusion and miliary disease. The pseudotumoral aspect was taken into consideration for consolidations with or without masslike effect with enhancement after contrast injection without the presence of air bronchogram(1). Bronchogenic dissemination was reported for air-space nodules, centrilobular nodules and tree-in-bud pattern(8). The terms utilized in the present paper follow the recommendations of the Consenso Brasileiro sobre a Terminologia dos Descritores de Tomografia Computadorizada do Tórax (Brazilian Consensus on Terminology Used to Describe Computed Tomography of the Chest)(9,10).
RESULTS The study sample included three girls and one boy in the age range between 3 and 14 months, three of them with malnutrition. History of cough and fever for at least one month was present in all of the four children (Table 1). All of them had been vaccinated with BCG at their first weeks of life and none was HIV-positive.
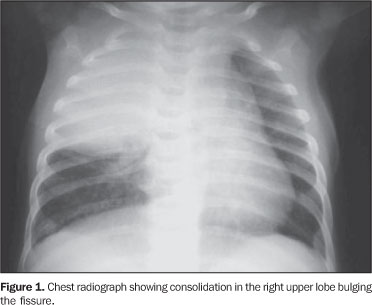
The diagnosis of tuberculosis was achieved with a positive culture of bronchoalveolar lavage in two of the children and positive culture of gastric aspirate in all of them; three patients presented with tuberculin skin test with an area of induration of 14 mm or greater (strong reactor); two of them had previous contact with household members diagnosed with pulmonary tuberculosis; initially, the four children had been unsuccessfully treated for pneumonia and, only after institution of specific therapy presented remission of symptoms and radiological aspects. All of the children were initially evaluated by chest radiography presenting lobar consolidation, bulging fissure similar to Klebsiella pneumonia, with no significant respiratory symptom. The investigation was extended with chest computed tomography for evaluation of parenchymal lesions characteristics (Tables 2 and 3).
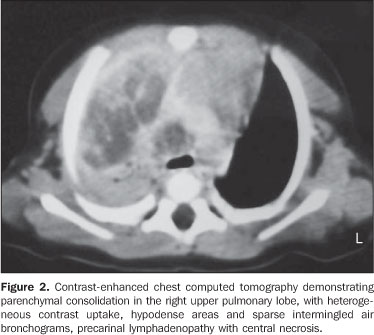
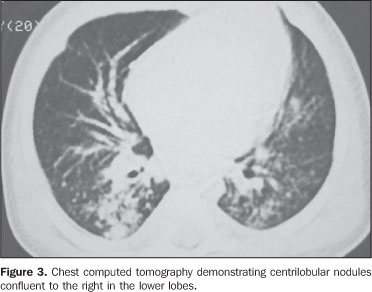
Case 1 - M.I.C., three-month-old female patient with chest radiograph demonstrating right upper lobe consolidation and nodular opacity in the pulmonary basis and right paracardiac nodular opacity (Figure 1). Tomographic findings included consolidations with sparse air bronchograms and subtle calcifications, irregular hypodense areas and a single cavitation; confluent signs of bronchogenic dissemination at right in the lower lobes; centrally hypodense precarinal and infracarinal lymph nodes with no calcification (Figures 2 and 3).
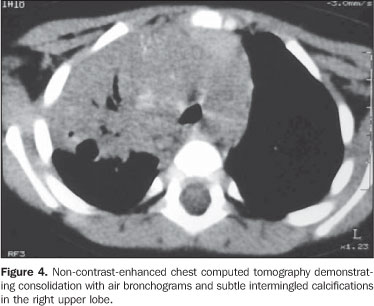
Case 2 - N.O.C., 11-month-old male patient presented lobular consolidation (right upper lobe) on chest radiograph. Computed tomography demonstrated consolidation in the right upper lobe with air bronchograms, hypodense areas, single cavitation and subtle, intermingled calcifications; signs of bronchogenic dissemination in the right lower lobe; cantrally hypodense infracarinal lymphadenopathy (Figure 4).
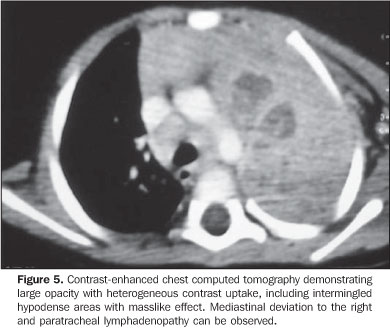
Case 3 - M.E.S., 14-month-old female patient with chest radiograph demonstrating pulmonary hyperaeration and consolidation in the left upper lobe, with tracheal compression and deviation to the right. Tomographic findings demonstrated a large opacity with intermingled hypodense areas with a masslike effect, without air bronchogram, calcifications or cavitations. Other findings were: mediastinal deviation to the right, reduction in the left source bronchus caliber and atelectasis, rare centrilobular opacities in the left lower lobe, small nodule in the left upper lobe and lymphadenomegaly with central hypodensity determining infracarinal widening (Figure 5).
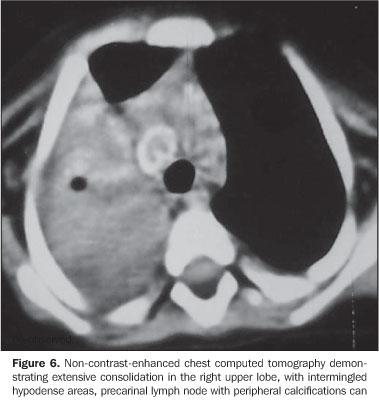
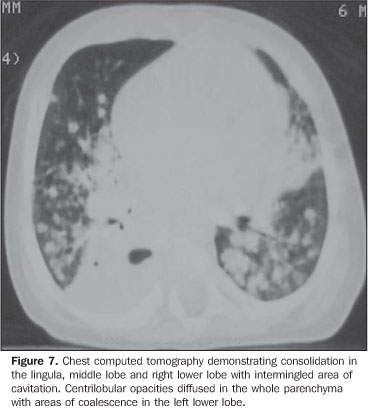
Case 4 - K.V., six-month-old female patient. Chest radiograph with consolidation in the left upper lobe, hyperinsuflation of the left lung and nodular opacities in the right lung basis and the whole left lung. Chest computed tomography demonstrated extensive consolidation in the right upper lobe with air bronchograms intermingled with hypodense areas, consolidation in the lingula, middle lobe and right lower lobe with intermingled areas of cavitation, diffused centrilobular opacities in the whole parenchyma with areas of coalescence in the lower lobes, atelectasis of the lingula, precarinal, infracarinal and para-hilar lymph nodes at right, with central hypodensity and peripheral calcification(s) (Figures 6 and 7).
DISCUSSION Most pulmonary tuberculosis cases observed in children are primary tuberculosis. The primoinfection is initiated with bacilli deposition in the pulmonary alveoli. This process produces a focal alveolar consolidation corresponding to the primary focus that is not always visualized on chest radiographs(1). This consolidation focus may develop and affect a segment of the whole lobe. The infection may disseminate from the primary focus to the central lymph nodes through lymphatic pathways resulting in regional lymphadenomegaly. The primary focus and the enlarged lymph nodes are called Ranke complex. In most of cases, parenchymal lesions and lymphadenomegaly present spontaneous resolution(1,7,11,12). In some cases, particularly involving infants, the lymph nodes continue to enlarge progressing up to caseous necrosis. This enlargement may result in regional bronchus compression causing stenosis, obstruction and emphysema. Additionally, inflamed lymph nodes may perforate adjacent bronchus and discharge caseous material into the bronchial tree, causing bronchogenic dissemination and/or focal or lobar pneumonia(1,7,12). The most frequent radiological findings in primary pulmonary tuberculosis of children are lymph node enlargement, parenchymatous disease, atelectasis, pleural effusion and military disease(4). In a tomographic study involving 25 children with ages up to 12 months, Kim et al.(1) have observed consolidation in 100% of patients, 59% with masslike presentation, 41% with necrosis, and 21% with cavitation intermingled with consolidation. Bronchogenic dissemination was found in 41% of cases. Parenchymal calcifications could be observed six months after, during the treatment(1,2). In another study(7), evaluating radiological patterns in 60 children aged up to 12 months, consolidation has been found in about 90% of them, a half with lobar involvement and 23% with cavitations. Leung et al.(4), analyzing chest radiographs of 191 patients in the age range between 20 days to 15 years, observed that the prevalence of parenchymal infiltration has reached 51% for children aged under three, and that hilar or mediastinal lymphadenopathy would be the most frequent abnormality in this age range(4), representing the second disease progression site(4,12). Parenchymal lesions would be most frequently found in children aged between 4 and 15 (88%) and would be seen as interstitial, alveolar or mixed opacities(4). Also, there are studies in the literature reporting masslike presentation without satellite lymphadenopathy(6) in children aged under two, which would be even more uncommon. In the cases described in the present study with four children aged under 14 months, the most frequent radiological pattern was lobar consolidation with calcifications, cavitations with intermingled necrotic areas in association with fissure bulging. Signs of bronchogenic dissemination and lymph node enlargement were observed in all of them. pseudotumoral consolidation with masslike effect was observed in one case. Infracarinal was the preferential localization of lymphadenopathy. All of the lymph nodes presented central caseous necrosis and, in two cases peripheral calcification was observed. Atelectasis and emphysema were observed in two patients. Miliary disease and pleural effusion were not observed in the cases included in the present study. Parenchymal calcifications were observed in three of the four cases in the present study, before specific treatment institution. In the studies reviewed(1,4,12), this finding was observed only during the follow-up of the patients along a period of more than ten months. However, Marais et al.(12) report that this finding may be observed at a short time interval in younger children, so the presence of calcifications may be related to the immunological response and to the time of the disease progression associated with the institution of specific therapy, allowing the utilization of this finding as an additional positive criterion for tuberculosis.
CONCLUSION In the present cases, the authors observed that primary pulmonary tuberculosis manifested with lobar consolidation is seen with characteristic images at computed tomography such as cavitations, hypodense areas and calcifications intermingled with consolidation. The association between lymphadenopathies with central necrosis and signs of bronchogenic dissemination reinforces the diagnosis of tuberculosis.
REFERENCES 1. Kim WS, Choi J, Cheon JE, et al. Pulmonary tuberculosis in infants: radiographic and CT findings. AJR Am J Roentgenol. 2006;187:1024-33. [ ] 2. Amodio J, Abramson S, Berdon W. Primary pulmonary tuberculosis in infancy: a resurgent disease in the urban United States. Pediatr Radiol. 1986;16:185-9. [ ] 3. Sant'Anna CC, Hijjar MA. Recente contribuição da Organização Mundial de Saúde para o controle da tuberculose na infância. Rev Saúde Pública. 2007;41(Supl. 1):117-20. [ ] 4. Leung AN, Müller NL, Pineda PR, et al. Primary tuberculosis in childhood: radiographic manifestations. Radiology. 1992;182:87-91. [ ] 5. Leung AN. Pulmonary tuberculosis: the essentials. Radiology. 1999;210:307-22. [ ] 6. Cherian MJ, Dahniya MH, al-Marzouk N, et al. Primary pulmonary tuberculosis presenting as mass lesions and simulating tumours in children. Australas Radiol. 1998;42:309-12. [ ] 7. Lamont AC, Cremin BJ, Pelteret RM. Radiological patterns of pulmonary tuberculosis in the paediatric age group. Pediatr Radiol. 1986;16:2-7. [ ] 8. Campos CA, Marchiori E, Rodrigues R. Tuberculose pulmonar: achados na tomografia computadorizada de alta resolução do tórax em pacientes com doença em atividade comprovada bacteriologicamente. J Pneumol. 2002;28:23-9. [ ] 9. Pereira-Silva JL, Kavakama J, Terra Filho M, et al. Consenso brasileiro sobre a terminologia dos descritores de tomografia computadorizada do tórax. J Bras Pneumol. 2005;31:149-56. [ ] 10. Souza Jr AS, Araujo Neto C, Jasinovodolinsky D, et al. Terminologia para a descrição de tomografia computadorizada de tórax (sugestões iniciais para um consenso brasileiro). Radiol Bras. 2002; 35:125-8. [ ] 11. Kim WS, Moon WK, Kim IO, et al. Pulmonary tuberculosis in children: evaluation with CT. AJR Am J Roentgenol. 1997;168:1005-9. [ ] 12. Marais BJ, Gie RP, Schaaf HS, et al. A proposed radiological classification of childhood intra-thoracic tuberculosis. Pediatr Radiol. 2004;34:886-94. [ ] Received October 30, 2008. * Study developed at Hospital Municipal Jesus, Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554