Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 51 nº 5 - Sep. / Oct. of 2018
Vol. 51 nº 5 - Sep. / Oct. of 2018
|
LETTERS TO THE EDITOR
|
|
Osteomyelitis of the maxilla caused by Actinomyces sp. |
|
|
Autho(rs): Lívia de Oliveira Antunes1; Rafael da Silveira Borges1; Wania Vasconcelos de Freitas1; Simone Rachid de Souza2; Diogo Goulart Corrêa3 |
|
|
Dear Editor,
We report the case of a 76-year-old female patient with diabetes and hypertension that were not being treated on a regular basis. She had undergone a tooth extraction, then continued to feel pain and had a persistent low fever, even during the course of oral antibiotic therapy. Over the following months, she lost multiple, contiguous, teeth at the previously manipulated site. Computed tomography for investigation of bone involvement showed soft-tissue density that was poorly defined, indicating bone erosion in the left maxilla, extending to the maxillary sinus, and palatal fistula. A biopsy of the lesion showed mixed inflammatory infiltrate with granulation tissue (visualized with hematoxylin-eosin staining) and actinomycete colonies permeating the bone tissue (visualized with Grocott’s staining), which allowed us to make a diagnosis of osteomyelitis caused by Actinomyces sp. (Figure 1). 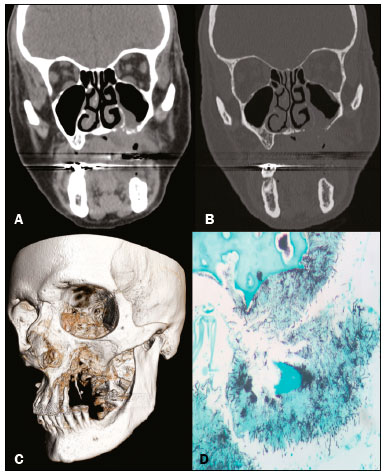 Figure 1. Computed tomography of the facial sinuses, with a soft-tissue window (A) and a bone window (B), reconstructed in the coronal plane, showing a soft-tissue density lesion eroding the maxilla, the floor of the maxillary sinus, and the left side of the palate, as well as forming a fistula from the oral cavity to the nasal cavity and to the left maxillary sinus. Three-dimensional reconstruction of a computed tomography scan (C), showing bone erosion in the maxilla and left palate. Grocott’s staining (D) showing colonies of filamentous Actinomyces bacteria interspersed with bone tissue (magnification, ×400). Actinomycosis is a chronic suppurative infection caused by the Gram-positive bacillus Actinomyces, the species Actinomyces israelii, which is a member of the endogenous flora often found in the teeth, oropharynx, gastrointestinal tract, and female genital tract, being the most common agent in humans(1). The most commonly affected area is the cervicofacial region (in 50-65% of cases), followed by the thorax (in 15-30%) and the abdomen/pelvis (in 20%). However, within the cervicofacial region, the maxilla is the least commonly affected site, accounting for only 0.5-9.0% of cases in the head and neck. Bone involvement is even more rare, osteomyelitis being sporadic or secondary to infection at primary sites(2-4). Risk factors for cervicofacial involvement include inadequate oral hygiene, trauma to the oral mucosa, chronic tonsillitis, otitis, mastoiditis, and osteonecrosis induced by radiotherapy or bisphosphonates. It is of note that, different than what is observed for the other affected sites, cervicofacial infection with Actinomyces sp. occurs more commonly in patients who are immunocompetent(2,3). In its acute form, actinomycosis usually manifests as edema of the soft tissues, together with the formation of masses and abscesses, evolving, chronically, to dissemination of the infection to the adjacent soft tissues, then the fascial planes, externalizing itself through fistulas of the skin and paranasal sinuses. However, it is rarely seen in combination with osteomyelitis(3). On computed tomography, actinomycosis appears as a mass with ill-defined borders, soft-tissue density, and contrast enhancement, together with fluid collections and fistulas. The differential diagnosis includes fungal ulcers, carcinoma, idiopathic midline granuloma, and osteomyelitis of the maxilla caused by other germs(5). In the histopathological analysis, hematoxylin-eosin staining reveals chronic abscess with polymorphonuclear leukocytes, granulation tissue and fibrosis, Grocott’s staining revealing colonies of bacilli forming “sulfur granules”, which represent tangled filaments of Actinomyces, present in abscesses, exudates of the sinus tract, or tissues infiltrated by the lesions(3,6). Penicillin G is the drug of choice for the treatment of actinomycosis, requiring long courses of antibiotic therapy. Surgical management is reserved for the drainage of bulky abscesses, marsupialization of chronically infected sinus tracts, excision of fibrotic lesions, and debridement of necrotic bone tissue(2). Therefore, despite its rarity, it is important to bear actinomycosis of the maxilla in mind as a differential diagnosis, mainly in cases of aggressive lesions of the mouth related to the abovementioned predisposing factors. REFERENCES 1. Crossman T, Herold J. Actinomycosis of the maxilla - a case report of a rare oral infection presenting in general dental practice. Br Dental J. 2009;206:201-2. 2. Valour F, Sénéchal A, Dupieux C, et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014;7:183-97. 3. Heo SH, Shin SS, Kim JW, et al. Imaging of actinomycosis in various organs: a comprehensive review. Radiographics. 2014;34:19-33. 4. Sezer B, Akdeniz BG, Günbay S, et al. Actinomycosis osteomyelitis of the jaws: report of four cases and a review of the literature. Journal of Dental Sciences. 2017;12:301-7. 5. Meethal AC, Pattamparambath M, Balan A, et al. Actinomycotic osteomyelitis of the maxilla - a delusive presentation. J Clin Diagn Res. 2016;10:ZJ01-3. 6. Elder DE, Elenitsas R, Johnson BL Jr, et al. Lever''s histopathology of the skin. 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009. 1. Hospital Casa de Portugal, Rio de Janeiro, RJ, Brazil 2. Hospital Federal do Andaraí, Rio de Janeiro, RJ, Brazil 3. Hospital Casa de Portugal e Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil Correspondence: Dra. Lívia de Oliveira Antunes Rua Gustavo Sampaio, 88, ap. 902, Leme Rio de Janeiro, RJ, Brazil, 22010-010 E-mail: li_antunes@hotmail.com |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554