Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 49 nº 6 - Nov. / Dec. of 2016
Vol. 49 nº 6 - Nov. / Dec. of 2016
|
LETTER TO THE EDITOR
|
|
Renal lymphangiectasia: know it in order to diagnose it |
|
|
Autho(rs): Andréa Farias de Melo Leite1; Bruna Venturieri1; Rosana Gonçalves de Araújo1; Eduardo Just Costa e Silva1; Jorge Elias Junior2 |
|
|
Dear Editor,
Here, we report the case of a 9-year-old girl with hyperparathyroidism. Ultrasound showed renal cysts and increased echogenicity of the parenchyma in both kidneys. The diagnostic hypothesis was hyperparathyroidism secondary to chronic/polycystic kidney disease. The patient presented with gradually worsening kidney function and hypertension, and new imaging scans were requested. The ultrasound showed anechoic, multiloculated images in the pyelocaliceal region of both kidneys, and perirenal, subcapsular cysts. A computed tomography (CT) scan was acquired, although no contrast agent was used, which precluded an accurate characterization. Nevertheless, the CT scan revealed changes similar to those observed on ultrasound. We also performed magnetic resonance imaging (MRI), which showed pyelocaliceal, perirenal cysts, with altered intensity of the signal of the renal parenchyma and loss of corticomedullary differentiation (Figure 1A), confirming, in conjunction with the clinical and biochemical data, the diagnosis of renal lymphangiectasia (RL). 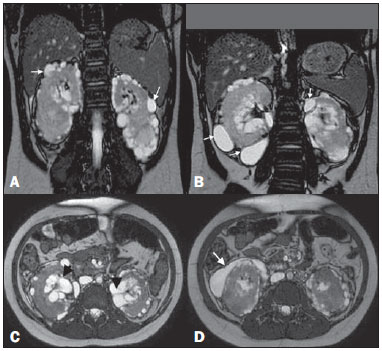 Figure 1. A: Coronal T2-weighted MRI sequence showing a loss of corticomedullary differentiation in both kidneys and multiple cystic lesions, with thin walls, located in the cortex (arrows). B: Cystic formations in the subcapsular cortex (arrows). C: Axial T2-weighted MRI sequence showing cysts located in the renal sinuses (arrowheads) and perinephric spaces, simulating pelvic dilatation. D: The same images simulating cystic collections in the subcapsular cortex (arrow). RL is a rare benign disease that occurs because of miscommunication between the renal lymphatic drainage system and the retroperitoneal lymphatic system(1). As a result, there is accumulation of lymph in the renal lymph ducts, making them ectatic and forming simple or multiloculated, typically asymmetric and bilateral, collections in the pyelocaliceal, perinephric, or parenchymal regions, although, in some cases, only a part of one kidney is affected (Figure 1—B,C). There is no predilection for a given gender or age group. As of 2005, only 40 cases had been described(1,2). In most cases, RL is an incidental finding, with or without signs and symptoms of pain, increased abdominal volume, hematuria, ascites, edema of the lower limbs, hypertension, erythrocytosis with renal vein thrombosis, and, rarely, chyluria(3). Such manifestations can be explained by the distention of the renal fascia and compression of the renal parenchyma by cysts, fistulization to the pelvic cavity, and changes in the renin-angiotensin system(2–4). In rare cases, chronic kidney disease has been reported(5). To our knowledge, there have been no specific reports of clinical evolution to hyperparathyroidism, although a relationship with chronic kidney disease can be assumed. A CT scan can reveal expansive perirenal formations with fluid attenuation, bounded by the renal fascia, that conform to (and do not invade) the adjacent structures. Those formations can compress the kidney cortex, expand the sinus and distort the calyceal system. In some cases, small, predominantly peripheral, hypodense collections can be seen, with attenuation values of 0–15 HU(3). There may be thickening of the renal fasciae and retroperitoneal collections crossing the midline at the level of the renal hilum. After the administration of iodine contrast, there is no enhancement of the collections or of the walls of the cystic formations(6). In MRI, the cysts exhibit a low signal on T1-weighted sequences—although the signal strength can be increased if there is bleeding(6)—and a more intense signal on T2-weighted sequences, without enhancement. In addition, RL can be diagnosed on MRI scans by identifying perirenal lymphatic collections with inversion of the corticomedullary signal intensity(1,4), as depicted in Figure 1—B,C,D. To suggest a diagnosis of RL, as well as to devise a treatment strategy and to prevent complications, it is essential to understand the radiological aspects of the disease and to differentiate it from other conditions that mimic cystic kidney disease. Although the combination of RL and renal failure is rare, knowledge of that association is also important to prevent comorbid conditions that can evolve with this complication, such as obesity and high blood pressure. REFERENCES 1. Rastoji R, Rastogi V. Computed tomographic scan in the diagnosis of bilateral renal lymphangiectasia. Saudi J Kidney Dis Transpl. 2008;19: 976–9. 2. Ashraf K, Raza SS, Ashraf O, et al. Renal lymphangiectasia. Br J Radiol. 2007;80:e117–8. 3. Vega J, Santamarina M. Linfangiectasia renal unilateral. Caso clínico. Rev Méd Chile. 2012;140:1312–5. 4. Restrepo JM, Amaya JEL, Sepúlveda NA, et al. Renal lymphangiectasia: MDCT and MRI findings. Rev Colomb Radiol. 2011;22:1–8. 5. Ueda S, Yanagida H, Sugimoto K, et al. Chronic renal insufficiency in a boy with cystic renal lymphangiectasia: morphological findings and longterm follow-up. Clin Nephrol. 2007;68:416–21. 6. Vasconcelos RA, Pereira ES, Bauab Jr T, et al. Renal lymphangiectasia: incidental finding at multislice computed tomography and literature review. Radiol Bras. 2012;45:178–80. 1. Instituto de Medicina Integral Professor Fernando Figueira de Pernambuco (IMIP), Recife, PE, Brazil 2. Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil Mailing address: Dra. Andréa Farias de Melo Leite Rua Laura Campelo, 130, Torre Recife, PE, Brazil, 50710-270 E-mail: andreafariasm@gmail.com |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554