Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 49 nº 1 - Jan. /Feb. of 2016
Vol. 49 nº 1 - Jan. /Feb. of 2016
|
LETTER TO THE EDITOR
|
|
Tracheobronchopathia osteochondroplastica: computed tomography, bronchoscopy and histopathological findings |
|
|
Autho(rs): Gabriela Maria Ribeiro e Ribeiro; Marcelo Ricardo Canuto Natal; Eduardo Felipe Silva; Sabrina Cardoso Freitas; Waldete Cabral Moraes; Fernanda Cunha Maciel |
|
|
Dear Editor,
A 41-year-old man with history of recurrent airways infection since his childhood, with chronic coughing and voice hoarseness for seven years. The patient was referred to undergo laryngotracheobronchoscopy that revealed the presence of whitish nodular lesions on the anterolateral walls of the trachea and at the most proximal portion of the main bronchi, whose material was sent for histopathological analysis (Figures 1A and 1B). Computed tomography (CT) showed tiny, subcentimeter, submucosal, sessile nodules, some of them calcified, at the different levels of the trachea, with predominance in the two lower thirds of the trachea, and also in the right main bronchus. No significant luminal narrowing was observed and, typically, the posterior membranous wall of the trachea was spared (Figures 1C and 1D). The patient remains under clinical follow-up with management of symptoms. 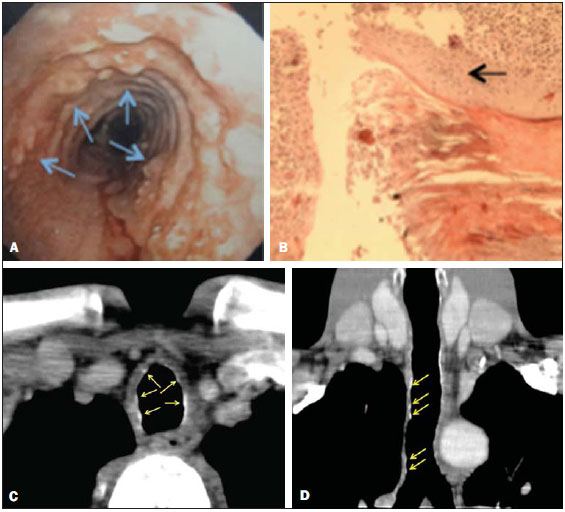 Figure 1. A: Laryngotracheobronchoscopy: whitish nodules on the anterolateral walls of the trachea (arrows). B: Histopathology. HE, 20×. Foci of squamous metaplasia in the trachea (arrow). C,D: Axial, contrastenhanced chest CT (C) and coronal reformation (D) showing micronodules, some of them calcified, on the anterolateral walls of the trachea (arrows). Tracheobronchopathia osteochondroplastica is a rare chronic benign disease, with male prevalence (male:female = 3:1), and predominantly manifesting between the fifth and seventh decades of life(1,2). Association with several factors has been reported, as follows: chronic infections; chemical or medicamentous agents; degenerative tissue alterations; calcium and phosphorus metabolism disorders; and amyloidosis(3,4). The disease is generally asymptomatic(1,2,5,6), and therefore, in most cases, the diagnosis is based on incidental findings at bronchoscopy performed to investigate other diagnoses or with therapeutic purposes, or even in series of necropsy(1). In cases of symptomatic disease, cough is the main finding, present in about 66% of cases. Generally, laryngotracheobronchoscopy raises the diagnostic suspicion and the classical finding is the presence of whitish, smooth and hard nodules, typically on the cartilaginous walls of the tracheal rings and of the proximal portions of the primary bronchi(7,8). The CT contributes to confirm the diagnosis(4) on the basis of its findings, namely, thickening of the inner surface of the tracheal cartilage with irregular, sessile nodular lesions, either calcified or not, focal or diffuse, sparing the posterior (membranous) trachea and leading to luminal narrowing in the affected areas(1,5,6,8,9). CT is very sensitive to detect the typical calcification of the nodules, to define the extent and distribution of tracheobronchial stenosis, as well as to characterize complications such as atelectasis, bronchiectasis, postobstructive pneumonia(5,10). Histopathological analysis shows that nodules correspond to submucosal osteocartilaginous growths. There are variable combinations of fibrotic, cartilaginous, bone, hematopoietic tissue and mineralized acellular protein matrix. The epithelium lining such nodules may be normal, or present with inflammatory or metaplastic appearance(5,8). Some authors consider that bronchoscopic and radiological findings are sufficient to establish the diagnosis, particularly in cases where it is difficult to perform biopsy(1,5,8). The prognosis is good in most of cases and treatment only will be requested in case of complications, principally tracheal and/or bronchial stenosis(11). REFERENCES 1. Bioque JC, Feu N, Rubio JM, et al. Tracheobronchopathia osteochondroplastica - clinical study and follow-up in nine cases. Journal of Bronchology. 2001;8:78-83. 2. Pinto JA, Silva LC, Perfeito DJP, et al. Osteochondroplastic tracheobronchopathy: report on 02 cases and bibliographic review. Braz J Otorhinolaryngol. 2010;76:789-93. 3. Williams SM, Jones ET. General case of the day. Tracheobronchopathia osteochondroplastica. Radiographics. 1997;17:797-9. 4. Faig-Leite FS, Defaveri J. Traqueobroncopatia osteocondroplástica em portador de tumor de Klatskin: relato de caso e revisão da literatura. J Bras Patol Med Lab. 2008;44:459-62. 5. Sá JM, Almeida J, Amado J, et al. Traqueobroncopatia osteocondroplástica - experiência de uma unidade de broncologia. Rev Port Pneumol. 2002;VIII:329-39. 6. Webb EM, Elicker BM, Webb WR. Using CT to diagnose nonneoplastic tracheal abnormalities: appearance of the tracheal wall. AJR Am J Roentgenol. 2000;174:1315-21. 7. Prince JS, Duhamel DR, Levin DL, et al. Nonneoplastic lesions of the tracheobronchial wall: radiologic findings with bronchoscopic correlation. Radiographics. 2002;22 Spec No:S215-30. 8. Khan AM, Klapper P, Jain VR, et al. Tracheobronchopathia osteochondroplastica: an entity diagnosed on bronchoscopy. Journal of Bronchology. 2006;13:99-101. 9. Kwong JS, Müller NL, Miller RR. Diseases of the trachea and mainstem bronchi: correlation of CT with pathological findings. Radiographics. 1992;12:645-57. 10. Marchiori E, Pozes AS, Souza Junior AS, et al. Alterações difusas da traquéia: aspectos na tomografia computadorizada. J Bras Pneumol. 2008;34:47-54. 11. Grenier PA, Beigelman-Aubry C, Brillet PY. Nonneoplastic tracheal and bronchial stenoses. Radiol Clin North Am. 2009;47:243-60. Hospital de Base do Distrito Federal (HBDF), Brasília, DF, Brazil Mailing Address: Dra. Gabriela Maria Ribeiro e Ribeiro Rua Gomes de Carvalho, 1005, ap. 3110, Vila Olímpia São Paulo, SP, Brazil, 04547-004 E-mail: gabiribeiroeribeiro@yahoo.com.br |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554