Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 48 nº 6 - Nov. / Dec. of 2015
Vol. 48 nº 6 - Nov. / Dec. of 2015
|
ORIGINAL ARTICLE
|
|
Compressive neuropathy of the first branch of the lateral plantar nerve: a study by magnetic resonance imaging |
|
|
Autho(rs): Rogéria Nobre Rodrigues1; Alexia Abuhid Lopes1; Jardélio Mendes Torres2; Marina Franco Mundim3; Lênio Lúcio Gavio Silva3; Breno Rabelo de Carvalho e Silva4 |
|
|
Keywords: Abductor digiti quinti muscle; Baxter; Lateral plantar nerve; Inferior calcaneal nerve; Atrophy. |
|
|
Abstract: INTRODUCTION
Heel pain is a very common complaint in orthopedic offices. The Brazilian radiological literature has recently been concerned with the relevant role played by imaging methods in the improvement of the diagnosis in the musculoskeletal system(1-15). Thalamic pain presents a wide spectrum of differential diagnosis including plantar fasciitis, fat pad involvement, stress fracture, enthesopathy and inflammatory arthropathy(16). One of the most common causes of chronic pain is entrapment of the first branch of the lateral plantar nerve, a condition that is known as Baxter's neuropathy(17,18). It is believed that approximately 20% of cases of pain in the medial region of the heel are associated with neuropathy of that nerve(19-22). Generally, the nerve to the abductor digiti quinti (ADQ) muscle originates as first branch of the lateral plantar nerve (82.1%) that divides itself at the level of the medial malleolus, but presents with some anatomical variations. In 11.7% of cases, such nerve may present as a direct branch from the posterior tibial nerve, or even originate from a common branch with the posterior branch to the lateral plantar nerve and with the medial calcaneal branch (4.1%) or in a branch in common with the posterior branch to the plantar square (2.1%)(23). The nerve follows the medial pathway along the long plantar ligament to the lateral, between the abductor hallucis muscle and the medial calcaneal tuberosity, inserting into the proximal aspect of the ADQ muscle (Figure 1). 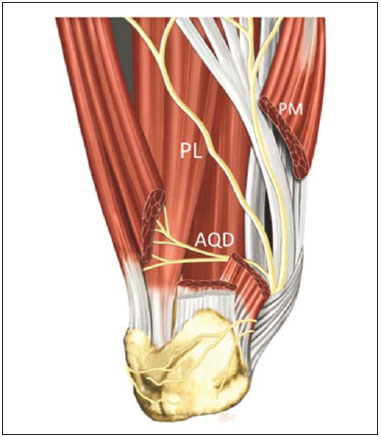 Figure 1. PM, medial plantar nerve; PL, lateral plantar nerve; AQD, abductor digiti quinti nerve. The nerve to the ADQ is mixed and originates motor nerves to the ADQ and, occasionally, to the short flexor of the digits and plantar square muscle, as well as sensory branches to the calcaneal periosteum, long plantar ligament and adjacent skin(24). Any situation determining increased volume in the region of the nerve might cause a focal compressive effect with consequential neuropathy. At clinical evaluation, the symptoms may not be distinguished from plantar fasciitis and, frequently, both conditions overlap(25). ADQ muscle weakness may be present in chronic cases, with decreased fifth toe abduction strength determined by the muscle degeneration. Magnetic resonance imaging (MRI) may be used to detect alterations associated with ADQ muscle denervation(18,26). The presence of such a muscle atrophy observed at MRI reflects a chronic compression of the inferior calcaneal nerve and contributes to the clinical diagnosis of Baxter's neuropathy(19). The literature suggests two possible sites of nerve entrapment which could result in Baxter's neuropathy, as follows: the first one, in patients with altered biomechanics, such as excessive pronation, since the nerve may be compressed in the movement of lateral rotation between the plantar square and abductor hallucis muscles(24); and second, either the nerve may be compressed as it passes anteriorly to the medial calcaneal tuberosity, or interfere mechanically with the plantar calcaneal spur(17,25,27,28) (Figure 2). 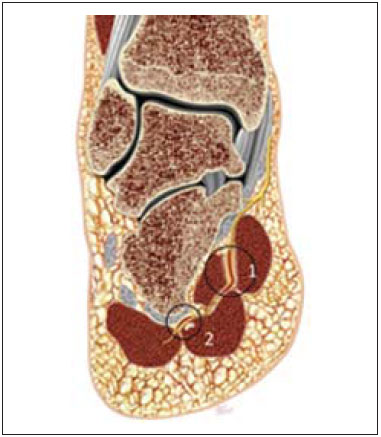 Figure 2. Two possible sites of nerve entrapment: 1 – in the nerve pathway between the deep fascia of the abductor muscle of the hallux and the medial plantar margin of the plantar square muscle; 2 – distally, in the nerve pathway along the medial calcaneal tuberosity. The present study is aimed at evaluating the prevalence of MRI findings associated with compression of the first branch of the lateral plantar nerve in patients with chronic heel pain manifesting by complete selective atrophy of the ADQ muscle. MATERIALS AND METHODS Retrospective, analytical, and cross-sectional study of 90 patients with diagnosis of. grade IV atrophy of ADQ muscle (according to Goutallier and Bernageau classification(29)) with mean age of 49.2 years, submitted to hindfoot MRI in a high field 1.5 T apparatus with fast spin echo, sagittalT1-weighted sequences and proton density (PD) with fat suppression, and axial and coronal/oblique PD T2-weighted sequences with fat suppression. After intravenous paramagnetic contrast injection, coronal and sagittal T1-weighted sequences with fat suppression were acquired. Only patients classified with grade IV atrophy of ADQ muscle (complete fatty muscle atrophy) were considered for evaluation. Amongst the evaluated patients, 21.2% were men with mean age of 42.1 years, and 78.8% were women with mean age of 56.3 years. RESULTS Atrophy of the ADQ muscle was most prevalent in women - 71 cases (78.8%) -, with a high prevalence in this group at the age ranges from 40 to 50 years (45.9%) and 50-60 years (38.3%), and p < 0.01 in both groups as demonstrated on Figure 3. On the other hand, no statistically significant difference was observed in the prevalence of atrophy of the ADQ muscle, as demonstrated on Figure 4. 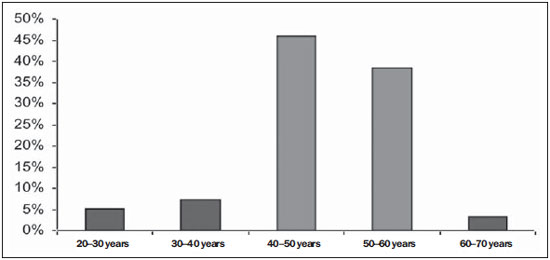 Figure 3. High prevalence of abductor digit quinti atrophy in patients aged between 40 and 50 years (45.9%) and between 50 and 60 years (38.3%). 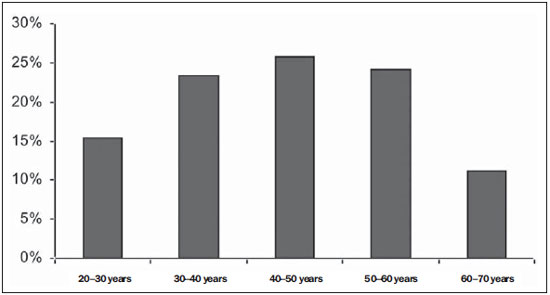 Figure 4. No statistically significant difference was observed as regards prevalence of ADQ muscle atrophy in male individuals. A strong correlation (p < 0.01) between grade IV atrophy of the ADQ muscle and plantar fasciitis and hindfoot varicosities in 21.2% and 16.8% of patients, respectively, considering isolated factors determining neural compression (Table 1). 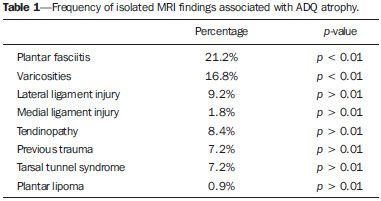 In the female group, plantar fasciitis and ankle varicosities were determinant as statistically significant (p < 0.01), while in the male group only the trauma factor was apparently reliable as an isolated factor of compressive neural injury (Table 2). 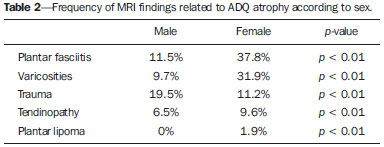 DISCUSSION MRI has shown to be an invaluable investigative method to detect muscle alterations associated with denervation. It is the most sensitive method to detect involvement of muscle tissues as compared with ultrasonography and computed tomography. Because of its noninvasive nature and capacity to demonstrate anatomical details, this method presents some advantages as compared with electromyography(30). Acute and subacute muscle denervation is more appropriately evaluated at fluid-sensitive MRI sequences such as PD/T2-weighted sequences with fat suppression or STIR sequences, showing increased signal intensity within the muscle belly as compared with the normal muscle, corresponding to neurogenic muscle edema(30,31) (Figure 5). The enhancement of the muscle by gadolinium also occurs either in the acute or subacute phase of denervation(30). In compressive Baxter's neuropathy, muscle edema occurs selectively inside the ADQ muscle and potentially in the short flexor muscle of the toes and plantar square muscle, depending on the anatomical variation in the patient. Chronic denervation leads to muscle atrophy and subsequent irreversible fat infiltration. Such findings are clearly depicted at T1-weighted images without fat suppression(30,31) (Figure 6). Typically, atrophy and fat infiltration occur homogeneously in the muscle belly. On the other hand, in the presence of double or redundant innervation, such changes either may not occur or occur heterogeneously(30). 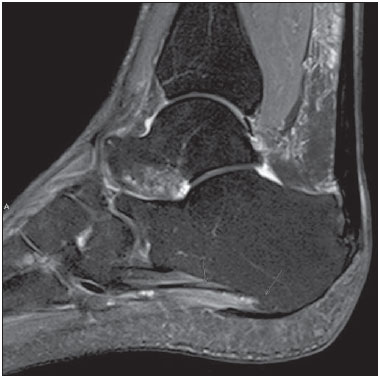 Figure 5. Sagittal MRI DP-weighted sequence with fat suppression showing signs of plantar fasciitis and abnormality in the signal of ADQ muscle fibers, that is hyperintense, corresponding to a pattern of edema resulting from acute denervation. 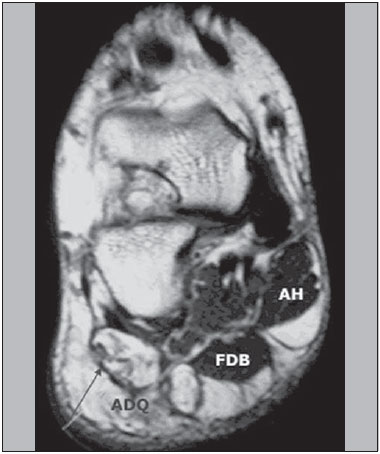 Figure 6. Coronal MRI T2-weighted image without fat saturation showing significant volumetric reduction of the ADQ muscle, with complete fatty infiltration of its fibers (grade IV) secondary to chronic denervation (> 1 year). It is estimated that in 20% of patients with chronic hell pain such condition is related to compression of the abductor digiti quinti nerve(32). In a study evaluating the association between ADQ atrophy and MRI findings of potential causes, there was a strong correlation between muscle atrophy and plantar fasciitis and calcaneal spur. However, the patients considered in such study presented with any degree of ADQ muscle atrophy(33). In the present study, the authors have selected only patients with grade IV atrophy, unequivocally evidencing the presence of compressive neuropathy. Chronic plantar fasciitis and local varicosities represented the findings most frequently associated with entrapment of the abductor digiti quinti nerve. Initially, heel pain should be treated with conservative measures, including the use of a nocturnal orthosis, therapeutic footwear, physical therapy, anti-inflammatory drugs and corticoid infiltration(16,34,35). As the pain becomes chronic, over a period longer than six month and without any improvement with the conservative treatment, the hypothesis of compression of the first branch of the lateral plantar nerve should be considered. In such cases, the patients may benefit from surgical decompression of the region(16,35-37) by endoscopic approach(16,36), radiofrequency ablation techniques(34) or open surgery. CONCLUSION Atrophy of the ADQ muscle is strongly associated with neuropathic compression of the first branch of the lateral plantar nerve. MRI is considered to be a noninvasive and highly accurate diagnostic method to evaluate grade IV atrophy of ADQ muscle and other associated diseases. REFERENCES 1. Terazaki CRT, Trippia CR, Trippia CH, et al. Synovial chondromatosis of the shoulder: imaging findings. Radiol Bras. 2014;47:38-42. 2. Arend CF. The carpal boss: a review of different sonographic findings. Radiol Bras. 2014;47:112-4. 3. Arend CF. Sonography of the iliotibial band: spectrum of findings. Radiol Bras. 2014;47:33-7. 4. Nakamura SA, Lorenzato MM, Engel EE, et al. Incidental enchondromas at knee magnetic resonance imaging: intraobserver and interobserver agreement and prevalence of imaging findings. Radiol Bras. 2013;46:129-33. 5. Souza CG, Gasparetto EL, Marchiori E, et al. Pyogenic and tuberculous discitis: magnetic resonance imaging findings for differential diagnosis. Radiol Bras. 2013;46:173-7. 6. Machado BB, Lima CMAO, Junqueira FP, et al. Magnetic resonance imaging in intersection syndrome of the forearm: iconographic essay. Radiol Bras. 2013;46:117-21. 7. Alves MPT, Fonseca COP, Granjeiro JM, et al. Carpal tunnel syndrome: comparative study between sonographic and surgical measurements of the median nerve in moderate and severe cases of disease. Radiol Bras. 2013;46:23-9. 8. Simão MN, Helms CA, Richardson WJ. Magnetic resonance imaging findings of disc-related epidural cysts in nonsurgical and postoperative microdiscectomy patients. Radiol Bras. 2012;45:205-9. 9. Chojniak R, Grigio HR, Bitencourt AGV, et al. Percutaneous computed tomography-guided core needle biopsy of soft tissue tumors: results and correlation with surgical specimen analysis. Radiol Bras. 2012;45:259-62. 10. Cotta AC, Melo RT, Castro RCR, et al. Diagnostic difficulties in osteoid osteoma of the elbow: clinical, radiological and histopathological study. Radiol Bras. 2012;45:13-9. 11. Tavares Júnior WC, Faria FM, Figueiredo R, et al. Bone attrition: a cause of knee pain in osteoarthritis. Radiol Bras. 2012;45:273-8. 12. Jacob Jr C, Barbosa DM, Batista PR, et al. Thoracolumbar burst fracture: what the radiologist should know. Radiol Bras. 2012;45:101-4. 13. Moura MVT. Trapped periosteum in a distal femoral physeal injury: magnetic resonance imaging evaluation. Radiol Bras. 2012;45:184-6. 14. Bayerl JS, Oliveira ARN, Peçanha PM, et al. Osteomyelitis of the wrist in a patient with disseminated paracoccidioidomycosis: a rare presentation. Radiol Bras. 2012;45:238-40. 15. Arend CF. Tenosynovitis and synovitis of the first extensor compartment of the wrist: what sonographers should know. Radiol Bras. 2012;45:219-24. 16. Thomas JL, Christensen JC, Kravitz SR, et al. The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. J Foot Ankle Surg. 2010;49(3 Suppl):S1-19. 17. Baxter DE, Thigpen CM. Heel pain - operative results. Foot Ankle. 1984;5:16-25. 18. Recht MP, Grooff P, Ilaslan H, et al. Selective atrophy of the abductor digiti quinti: an MRI study. AJR Am J Roentgenol. 2007;189:W123-7. 19. Delfaut EM, Demondion X, Bieganski A, et al. Imaging of foot and ankle nerve entrapment syndromes: from well-demonstrated to unfamiliar sites. Radiographics. 2003;23:613-23. 20. Oztuna V, Ozge A, Eskandari MM, et al. Nerve entrapment in painful heel syndrome. Foot Ankle Int. 2002;23:208-11. 21. Przylucki H, Jones CL. Entrapment neuropathy of muscle branch of lateral plantar nerve: a cause of heel pain. J Am Podiatry Assoc. 1981;71:119-24. 22. Baxter DE. Release of the nerve to the abductor digiti minimi. In: Kitaoka HB, editor. Master techniques in orthopaedic surgery. The foot and ankle. Philadelphia, PA: Lippincott Williams & Wilkins; 2002. p. 359. 23. del Sol M, Olave E, Gabrielli C, et al. Inervation of the abductor digiti minimi muscle of the human foot: anatomical basis of the entrapment of the abductor digiti minimi nerve. Surg Radiol Anat. 2002;24:18-22. 24. Rondhuis JJ, Huson A. The first branch of the lateral plantar nerve and heel pain. Acta Morphol Neerl Scand. 1986;24:269-79. 25. Offutt S, DeHeer P. How to address Baxter's nerve entrapment. Podiatry Today. 2004;17:52-8. 26. Alshami AM, Souvlis T, Coppieters MW. A review of plantar heel pain of neural origin: differential diagnosis and management. Man Ther. 2008;13:103-11. 27. Donovan A, Rosenberg ZS, Cavalcanti CF. MR imaging of entrapment neuropathies of the lower extremity. Part 2. The knee, leg, ankle, and foot. Radiographics. 2010;30:1001-19. 28. Louisia S, Masquelet AC. The medial and inferior calcaneal nerves: an anatomic study. Surg Radiol Anat. 1999;21:169-73. 29. Lippe J, Spang JT, Leger RR, et al. Inter-rater agreement of the Goutallier, Patte, and Warner classification scores using preoperative magnetic resonance imaging in patients with rotator cuff tears. Arthroscopy. 2012;28:154-9. 30. Kim SJ, Hong SH, Jun WS, et al. MR imaging mapping of skeletal muscle denervation in entrapment and compressive neuropathies. Radiographics. 2011;31:319-32. 31. Fleckenstein JL, Watumull D, Conner KE, et al. Denervated human skeletal muscle: MR imaging evaluation. Radiology. 1993;187:213-8. 32. Shon LC, Easley ME. Chronic pain. In: Myerson MS, editor. Foot and ankle disorders. Philadelphia, PA: WB Saunders; 2000. p. 815-81. 33. Chundru U, Liebeskind A, Seidelmann F, et al. Plantar fasciitis and calcaneal spur formation are associated with abductor digiti minimi atrophy on MRI of the foot. Skeletal Radiol. 2008;37:505-10. 34. Cozzarelli J, Sollitto RJ, Thapar J, et al. A 12-year long-term retrospective analysis of the use of radiofrequency nerve ablation for the treatment of neurogenic heel pain. Foot Ankle Spec. 2010;3:338-46. 35. Baxter DE, Pfeffer GB. Treatment of chronic heel pain by surgical release of the first branch of the lateral plantar nerve. Clin Orthop Relat Res. 1992;(279):229-36. 36. Mesmar M, Amarin Z, Shatnawi N, et al. Chronic heel pain due to the entrapment of the first branch of the lateral plantar nerve: analysis of surgical treatment. Eur J Orthop Surg Traumatol. 2010;20:563-7. 37. Goecker RM, Banks AS. Analysis of release of the first branch of the lateral plantar nerve. J Am Podiatr Med Assoc. 2000;90:281-6. 1. MDs, Musculoskeletal Radiologists, Axial Medicina Diagnóstica, Belo Horizonte, MG, Brazil 2. MD, Orthopedist, Head of the Foot Surgery Group at Santa Casa de Belo Horizonte, Professor at Faculdade de Ciências Médicas de Minas Gerais (FCMMG), Belo Horizonte, MG, Brazil 3. MDs, Radiologists, Axial Medicina Diagnóstica, Belo Horizonte, MG, Brazil 4. MD, Physician Assistant, Axial Medicina Diagnóstica, Belo Horizonte, MG, Brazil Mailing Address: Dra. Rogéria Nobre Rodrigues Rua Gonçalves Dias, 2867, Santo Agostinho Belo Horizonte, MG, Brazil, 30140-093 E-mail: rnobre@terra.com.br Received December 23, 2013. Accepted after revision May 7, 2015. Study developed at Axial Medicina Diagnóstica, Belo Horizonte, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554