Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 48 nº 3 - May / June of 2015
Vol. 48 nº 3 - May / June of 2015
|
LETTER TO THE EDITOR
|
|
Doege-Potter syndrome |
|
|
Autho(rs): Bruno Lima Moreira; Marlon Augusto Schiocchet Monarim; Ricardo Francisco Tavares Romano; Leandro Accardo Mattos; Giuseppe D'Ippolito |
|
|
Dear Editor,
A male, 81-year-old patient admitted because of a progressive increase of the abdominal volume for five months, in association with daily episodes of sudden sweating with syncope. Physical examination revealed the presence of a palpable mass in the right flank and hypogastrium. Computed tomography (CT) (Figures 1A and 1B) demonstrated a voluminous, predominantly solid, expansile retroperitoneal mass in the right hemiabdomen, with lobulated contours and heterogeneous density, measuring 19.0 × 15.0 × 12.0 cm. The upper portion of the mass exhibited heterogeneous enhancement delimiting areas of necrosis or cystic/myxoid degeneration, while the lower portion was less vascularized. Neither calcification nor fat were observed. At magnetic resonance imaging (MRI) (Figures 1C and 1D), the lesion exhibited heterogeneous signal intensity on T2-weighted image, with areas of high signal intensity and a focus of marked low signal intensity located between the superior and inferior portions. At T1-weighted image, the mass was subtly heterogeneous, with no fatty or hematic contents. The lower portion of the lesion presented diffusion restriction. After intravenous contrast injection (gadolinium), the mass exhibited enhancement similar to the one above described for CT. 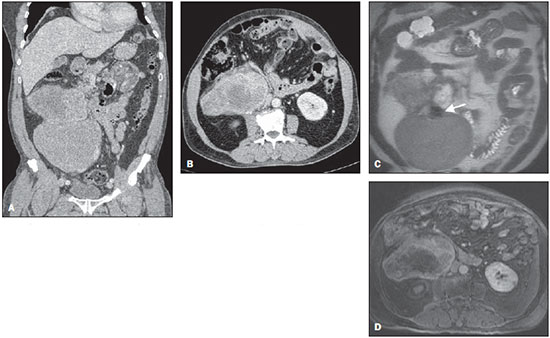 Figure 1. A: Iodinated contrast-enhanced CT (portal phase) – coronal reconstruction – identifies a large retroperitoneal, heterogeneous mass with two main portions. The upper portion of the mass is more heterogeneous and presents intense, peripheral enhancement, delimiting areas of necrosis or cystic/myxoid degeneration. The lower portion of the mass is less vascularized. B: Iodinated contrast enhanced CT (portal phase) – axial section – shows the region of the upper portion of the mass with heterogeneous density and enhancement. C: Coronal MRI T2-weighted HASTE image reveals a voluminous retroperitoneal, lobulated lesion with two distinctive portions, the upper portion more heterogeneous, with foci of high signal intensity on T2-weighted image and the lower portion with intermediate and less heterogeneous signal intensity. The white arrow indicates a nodular area with marked low signal intensity on T2-weighted image, which might correspond to a dense fibrotic stroma. D: Axial MRI T1-weighted image with fat saturation after intravenous contrast (gadolinium) injection in the region of the upper portion of the lesion shows findings similar to the ones observed at CT. At admission, hypoglycemic episodes were characterized. The lowest value for fasting glycemia was 29 mg/dL (normal: 70-99 mg/dL). The hypothesis of insulinoma was ruled out by the low insulin serum levels, and hypoinsulinemic hypoglycemia was characterized. Plasma IGF-I and IGF-II levels were measured, and the values were respectively 32.00 ng/mL (normal: 55-166 ng/mL) and 594 ng/mL (normal: 288-736 ng/mL). Because of the ratio IGF-II/IGF-I of 18.56 (normal, up to 3:1; > 10 is suggestive of hypoglycemia caused by non-islet cell tumors), Doege-Potter syndrome (DPS) was considered as the most probable hypothesis(1-4). The patient utilized prednisone for glycemic control and underwent percutaneous biopsy and later surgical intervention. Morpho-histopathological analysis in association with the immunohistochemical profile indicated a malignant solitary fibrotic tumor (SFT) with extensive areas of necrosis. Since his hospital discharge, the patient has not presented any hypoglycemic episode. SFT is a rare neoplasia and, in spite of its originally described pleural origin, it may occur in any site of the body(5-8). Clinically, many times, such tumor manifests as an asymptomatic slow-growing mass, frequently occurring in middle-aged individuals, with no predilection for sex(5-7). It may cause pain and symptoms resulting from adjacent structures compression(5). DPS refers to the paraneoplastic phenomenon characterized by hypoglycemia secondary to the SFT as it produces high-molecular-weight IGF-II prohormone in excess(1,4,5). Surgical resection is the treatment of choice for SFT and can cure hypoglycemia(1-5). Most SFTs are benign. Malignant SFTs are typically large, presenting areas of necrosis and hemorrhage in addition to cellular atypia and a high number of mitotic figures(5). At CT, SFT generally is seen as a circumscribed, lobulated, hypervascular mass, either displacing or compressing adjacent structures. The non-enhanced central areas of the mass represent necrosis, cystic/myxoid degeneration or hemorrhage. Calcifications are rarely found(5-7). At MRI, a SFT typically presents an intermediate signal intensity on T1-weighted images, and heterogeneous signal intensity on T2-weighted images, with areas of high signal intensity (necrosis or cystic/myxoid degeneration) and low signal intensity (fibrosis/collagen or flow void), with possible intense, predominantly peripheral enhancement in association with non-enhanced areas(5-7). Histopathological and immunohistochemical analyzes are necessary to confirm the diagnosis(6). REFERENCES 1. Bodnar TW, Acevedo MJ, Pietropaolo M. Management of non-islet-cell tumor hypoglycemia: a clinical review. J Clin Endocrinol Metab. 2014;99:713-22. 2. Khowaja A, Johnson-Rabebett B, Bantle J, et al. Hypoglycemia mediated by paraneoplastic production of insulin like growth factor-2 from a malignant renal solitary fibrous tumor - clinical case and literature review. BMC Endocr Disord. 2014;14:49. 3. Dutta P, Aggarwal A, Gogate Y, et al. Non-islet cell tumor-induced hypoglycemia: a report of five cases and brief review of the literature. Endocrinol Diabetes Metab Case Rep. 2013;2013:130046. 4. Schutt RC, Gordon TA, Bhabhra R, et al. Doege-Potter syndrome presenting with hypoinsulinemic hypoglycemia in a patient with a malignant extrapleural solitary fibrous tumor: a case report. J Med Case Rep. 2013;7:11. 5. Shanbhogue AK, Prasad SR, Takahashi N, et al. Somatic and visceral solitary fibrous tumors in the abdomen and pelvis: cross-sectional imaging spectrum. Radiographics. 2011;31:393-408. 6. Ginat DT, Bokhari A, Bhatt S, et al. Imaging features of solitary fibrous tumors. AJR Am J Roentgenol. 2011;196:487-95. 7. Wignall OJ, Moskovic EC, Thway K, et al. Solitary fibrous tumors of the soft tissues: review of the imaging and clinical features with histopathologic correlation. AJR Am J Roentgenol. 2010;195:W55-62. 8. Batista GR, D'Ippolito G, Szejnfeld J, et al. Tumor fibroso solitário do rim: descrição de caso. Radiol Bras. 2005;38:313-5. Escola Paulista de Medicina da Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil Mailing Address: Dr. Bruno Lima Moreira Departamento de Diagnóstico por Imagem - EPM-Unifesp Rua Napoleão de Barros, 800, Vila Clementino São Paulo, SP, Brazil, 04024-012 E-mail: limamoreiramed@gmail.com |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554