Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 48 nº 3 - May / June of 2015
Vol. 48 nº 3 - May / June of 2015
|
ORIGINAL ARTICLE
|
|
Transcatheter arterial embolization for unresectable symptomatic giant hepatic hemangiomas: single-center experience using a lipiodol-ethanol mixture |
|
|
Autho(rs): Denis Szejnfeld1; Thiago Franchi Nunes2; Vinicius Adami Vayego Fornazari1; Carla Adriana Loureiro de Matos3; Adriano Miziara Gonzalez4; Giuseppe D'Ippolito5; Ivonete Sandra de Souza e Silva3; Suzan Menasce Goldman5 |
|
|
Keywords: Hemangioma; Therapeutic embolization; Ethanol; Ethiodized oil. |
|
|
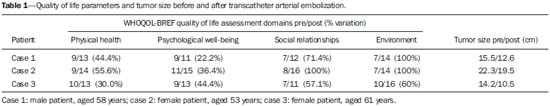
Abstract: INTRODUCTION
Hepatic hemangiomas are the most common benign liver tumors. They are usually asymptomatic and require no intervention(1,2). Hepatic hemangiomas are considered to be "giant" when greater than 5 cm, and the larger ones are more prone to spontaneous rupture(3,4). Spontaneous rupture is considered to be exceptionally rare in the absence of anticoagulant therapy or trauma and in such a situation the presence of underlying liver disease should be considered(4,5). Traditionally, patients with persistent pain are considered for resection when other causes for the pain have been excluded(3,6). In some cases, giant hemangiomas may present with extensive involvement of the hepatic hilum, veins and/or extension into the thorax and/or pelvis, and surgery becomes a high-risk procedure in these patients(6). Transcatheter arterial embolization (TAE) was first used in 1991 by Yamamoto et al.(7) as a preoperative procedure in a case of ruptured hemangioma. Since then, only a few reports on the use of TAE for the treatment of symptomatic (non-hemorrhagic) liver hemangiomas have been published(8,9). To the best of the authors' knowledge, no report using lipiodol-ethanol injection therapy has been published to date. The purpose of the present article is to report the authors' experience with TAE using a lipiodol-ethanol mixture in a small series of patients with symptomatic, unresectable giant hepatic hemangiomas. MATERIALS AND METHODS The study was approved by the local Committee for Ethics in Research (Institutional Review Board-equivalent) and was conducted in accordance with the provisions of the Declaration of Helsinki. A term of free and informed consent was obtained from all the patients prior to their inclusion in the study. Three cases of embolized hemangiomas between 2009 and 2010 were retrospectively reviewed. All the patients reported symptoms for at least three years, and none had undergone previous abdominal surgery. A quality of life questionnaire(10) was applied to each patient, 15 days before and 60 days after the procedure, to assess physical health, psychological well-being, and different aspects of their social relationships and social environment before and after TAE. The World Health Organization Quality of Life (WHOQOL) project was initiated in 1991 with the objective of developing an international cross-culturally comparable quality of life assessment instrument. It assesses the individuals' perception in the context of their culture and value systems, and their personal goals, standards and concerns. All the nodules showed the typical pattern of hemangiomas at contrast-enhanced computed tomography (CT) and/or magnetic resonance imaging (MRI). No biopsies were performed. All the patients were considered to be high-risk cases and were ineligible for major hepatic resection, because of involvement of multiple segments and/or extensive contact of the tumor with major vessels (Figure 1). 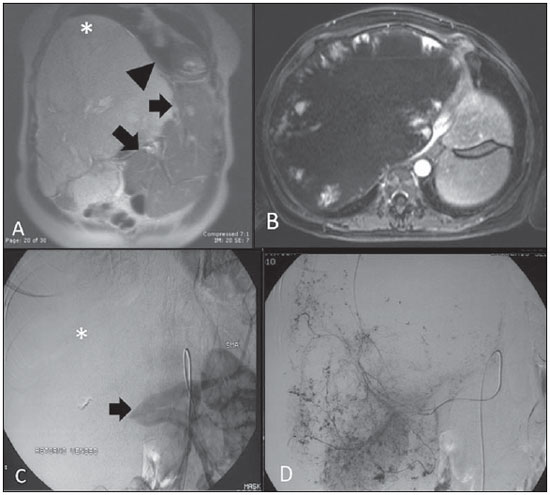 Figure 1. A: Coronal, T2-weighted MR image showing extension of the giant hemangioma into the thorax (asterisk) and displacement of the heart (arrowhead) as well as of normal liver parenchyma (arrows). B: Axial post-gadolinium-enhanced MR image showing the typical pattern of hemangioma. C: Late venous phase of digital subtraction arteriogram showing displacement of the portal vein (arrow) to the left and no portal venous enhancement characterizing hemangioma (asterisk). D: Digital subtraction arteriogram image of right hepatic artery showing a diffuse nodular pattern of hemangioma. Embolization procedures were performed under conscious sedation using a Philips Integris V3000 digital angiography unit (Philips Medical Systems; Best, The Netherlands). Initial diagnostic angiography was performed using a 5-F catheter to selectively examine the superior mesenteric artery, celiac trunk and hepatic artery in the late venous phase for patent tumor-feeding branches and to evaluate a possible blood flow into the tumor through the portal vein. Pre-embolization superselective angiography was performed to identify possible non-target flow or arteriovenous fistulas that might require prophylactic embolization. A superselective technique using a 0.028-inch microcatheter (Embocath, BioSphere Medical; Rockland, MA) was employed for embolization of the feeding branches. Before embolization, 2 mL of 0.5% lidocaine was slowly injected. A transarterial mixture of 8 mL of absolute ethanol and 2 mL of lipiodol (ethiodol) (Lipiodol® Ultra-Fluide, Guerbet Laboratories; Aulnay-Sous-Bois, France) was then injected into each feeding branch until stasis was achieved. No more than 10 mL of the lipiodol-ethanol mixture was needed to stop the flow of the embolized arteries. All three patients experienced moderate pain after TAE and received fentanyl (2 mL), ondansetron (8 mL), and a single dose of cefazolin (1 g). The same quality of life questionnaire was applied again and imaging tests (CT or MRI) were repeated for each patient after 60-90 days. RESULTS One patient was male, aged 58 years, and two were female, aged 53 and 61 years. The total dose of infused lipiodol-ethanol per patient was 9, 8, and 7 mL, respectively. Transcatheter arterial embolization was successful in all the cases, and the patients were discharged within 12 hours after the procedure. No immediate procedure-related complication was observed, nor any in the 60-90 day follow-up period. Quality of life parameters and tumor size assessed before and after TAE are summarized on Table 1. Two patients showed a moderate decrease and one patient showed a slight decrease (no more than 10% in the maximum diameter) in tumor size after TAE (Figure 2). Quality of life assessment revealed significant symptom regression and improvement in all four domains related to quality of life (physical health, psychological well-being, social relationships and environment) for all three patients (Table 1). 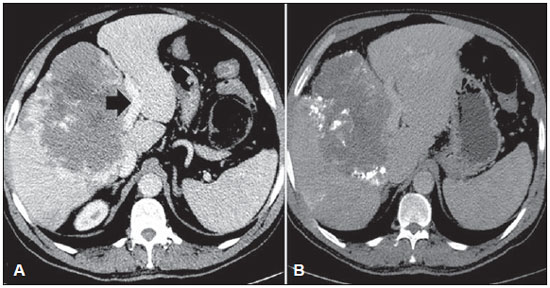 Figure 2. A: Pre-embolization axial, contrast-enhanced CT image showing extensive contact of the tumor with the left portal branch (arrow) and the typical pattern of hemangioma. B: Post-embolization CT image showing diffusion of lipiodol within the nodule and tumor size decrease. DISCUSSION Until the 1990s, there was no consensus in the literature as to an effective treatment for hepatic hemangiomas. In the last decade, several authors have reported that giant hemangiomas may cause symptoms such as incapacitating pain, abdominal discomfort, and dyspnea in about 40-50% of patients, with successful regression of symptoms after therapy(5,6,11). In the present study, complete symptoms regression and significant quality of life improvement were achieved in all cases after embolization with a transarterial mixture of ethanol and lipiodol. No other symptomatic medication was required (except for post-embolization pain relief), nor any other treatment during the follow-up period. The present results are consistent with earlier reports documenting that large liver hemangiomas are responsible for the symptoms, after exclusion of other possible causes of pain(6,8,9). Although liver hemangiomas resection can be performed with low morbidity in the presence of extensive parenchymal involvement (three or more segments), such procedure presents potential for significant complications and morbidity due to its surgical nature(6). Similar embolization procedures, such as transcatheter arterial chemoembolization (TACE) for hepatocellular carcinoma, are safe and usually performed on an outpatient basis. Immediate pain related to the injected ethanol dose in TAE was similar to that in TACE patients and was controlled with administration of oral opioid and anti-inflammatory drugs for seven days. Hemangiomas are composed of large blood-filled spaces lined by endothelium. The authors' hypothesis was that it would not be possible to fill and adequately embolize all these spaces with polyvinyl alcohol particles, and a liquid embolic agent such as absolute ethanol and lipiodol would be more appropriate to fill the vascular channels and destroy the endothelium, causing occlusion(12). This principle has already been adopted in the embolization of peripheral venous angiomas. The present study has some limitations such as the small sample size, with only three patients. However, symptomatic and unresectable giant hemangiomas are uncommon, and even in a large institution as ours, it would be difficult to have a large single-center pool of patients. In summary, based on these results, the authors conclude that TAE using ethanol mixed with lipiodol was a safe and effective treatment for symptomatic and unresectable giant hepatic hemangiomas in this small series of patients. REFERENCES 1. Paradis V. Benign liver tumors: an update. Clin Liver Dis. 2010;14:719-29. 2. Galvão BVT, Torres LR, Cardia PP, et al. Prevalence of simple liver cysts and hemangiomas in cirrhotic and non-cirrhotic patients submitted to magnetic resonance imaging. Radiol Bras. 2013;46:203-8. 3. Lise M, Feltrin G, Da Pian PP, et al. Giant cavernous hemangiomas: diagnosis and surgical strategies. World J Surg. 1992;16:516-20. 4. Paula Neto WT, Koifman ACB, Martins CAS. Ruptured hepatic cavernous hemangioma: a case report and literature review. Radiol Bras. 2009;42:271-3. 5. Donati M, Stavrou GA, Donati A, et al. The risk of spontaneous rupture of liver hemangiomas: a critical review of the literature. J Hepatobiliary Pancreat Sci. 2011 Jul 29. [Epub ahead of print]. 6. Yoon SS, Charny CK, Fong Y, et al. Diagnosis, management, and outcomes of 115 patients with hepatic hemangioma. J Am Coll Surg. 2003;197:392-402. 7. Yamamoto T, Kawarada Y, Yano T, et al. Spontaneous rupture of hemangioma of the liver: treatment with transcatheter hepatic arterial embolization. Am J Gastroenterol. 1991;86:1645-9. 8. Srivastava DN, Gandhi D, Seith A, et al. Transcatheter arterial embolization in the treatment of symptomatic cavernous hemangiomas of the liver: a prospective study. Abdom Imaging. 2001;26:510-4. 9. Zeng Q, Li Y, Chen Y, et al. Gigantic cavernous hemangioma of the liver treated by intra-arterial embolization with pingyangmycin-lipiodol emulsion: a multi-center study. Cardiovasc Intervent Radiol. 2004;27:481-5. 10. [No authors listed]. Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28:551-8. 11. Vassiou K, Rountas H, Liakou P, et al. Embolization of a giant hepatic hemangioma prior to urgent liver resection. Case report and review of the literature. Cardiovasc Intervent Radiol. 2007;30:800-2. 12. Yu SC, Hui JW, Hui EP, et al. Embolization efficacy and treatment effectiveness of transarterial therapy for unresectable hepatocellular carcinoma: a case-controlled comparison of transarterial ethanol ablation with lipiodol-ethanol mixture versus transcatheter arterial chemoembolization. J Vasc Interv Radiol. 2009;20:352-9. 1. MDs, Department of Imaging Diagnostic, Federal University of São Paulo (Unifesp), São Paulo, SP, Brazil 2. MSc, Department of Imaging Diagnostic, Federal University of São Paulo (Unifesp), São Paulo, SP, Brazil 3. MDs, Department of Gastrointestinal Surgery, Federal University of São Paulo (Unifesp), São Paulo, SP, Brazil 4. PhD, Department of Gastrointestinal Surgery, Federal University of São Paulo (Unifesp), São Paulo, SP, Brazil 5. PhDs, Department of Imaging Diagnostic, Federal University of São Paulo (Unifesp), São Paulo, SP, Brazil Mailing Address: Dr. Vinicius Adami Vayego Fornazari Rua Napoleão de Barros, 800, Vila Clementino São Paulo, SP, Brazil, 04024-002 E-mail: vfornazari@yahoo.com.br Received July 2, 2014. Accepted after revision November 13, 2014. Study developed at Federal University of São Paulo (Unifesp), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554