Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 48 nº 2 - Mar. / Apr. of 2015
Vol. 48 nº 2 - Mar. / Apr. of 2015
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Ricardo Schwingel1; Stenio Bruno Leal Duarte1; Mariana Mari Oshima1; João Vitor do Amaral Mesquita1; Fabiano Reis2 |
|
|
A female, 23-year-old patient presenting with headache and uncontrollable vomiting for four months. Magnetic resonance imaging of the brain and spinal cord was performed (Figure 1).
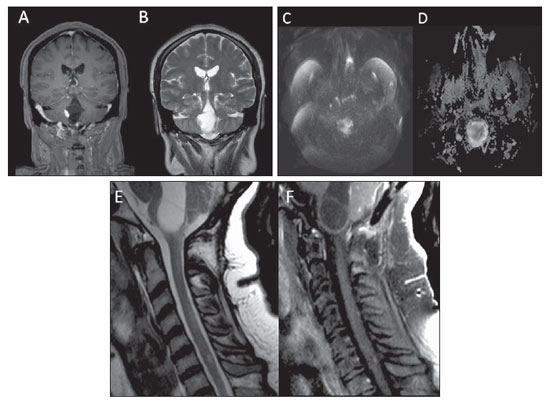 Figure 1. (A-D): Brain magnetic resonance imaging, coronal, T1-weigthed image with fat saturation, after intravenous paramagnetic (gadolinium) contrast injection (A), coronal, T2-weighted image (B), axial, diffusion-weighted image (DWI) (C), axial ADC map (D). E,F: Spinal cord magnetic resonance imaging, sagittal, T2-weighted image (E) and contrast-enhanced sagittal, T1-weighted image with fat saturation (F). Images description Figure 1. A-D: Brain magnetic resonance imaging. Contrast-enhanced, coronal, T1-weighted image (A) shows two cerebellar lesions (the largest one in the vermis, and the smallest one in the upper right hemisphere), with diffuse nodular contrast enhancement of the smallest lesion and of the eccentric solid component of the largest lesion, demonstrating isointensity at T2-weighted image (B). The cystic component of the largest lesion extends toward the lower portion of the fourth ventricle. There is a focus of diffusion facilitation characterized by hyposignal at diffusion-weighted image (C) and hypersignal at the ADC map (D). E,F: Spinal cord magnetic resonance imaging. Sagittal, T2-weighted (E) and contrast-enhanced T1-weighted (F) images show two ovoid lesions in the region of the cervical cord with hypersignal on T2-weighted image, demonstrating enhancement after contrast injection at C4 and C6 levels. Diagnosis: Multiple hemangioblastomas, association with von Hippel-Lindau syndrome. COMMENTS The imaging evaluation of the central nervous system (CNS), particularly with magnetic resonance imaging, has been approached in a series of recent publications in the Brazilian radiological literature(1-9). Main differential diagnoses of cerebellar lesions with radiological characteristics exhibited by such a condition include hemangioblastomas, metastases and pilocytic astrocytoma. The lesions multiplicity favors the two first hypotheses. The patient's age range is compatible with hemangioblastoma, considering that pilocytic astrocytoma affects pediatric patients and metastasis would be expected in older patients. Additionally, the absence of supratentorial lesions favors the hypothesis of hemangioblastomas in relation to metastases, particularly in cases of multiple lesions, considering that least probably hematogenic neoplastic dissemination would affect only the infratentorial region due to the greater blood flow toward the supratentorial region(10). The hypothesis of multiple hemangioblastomas should lead one to consider an association with von Hippel-Lindau syndrome, that is a rare dominant autosomal familial cancer syndrome related to inactivation of a tumor suppressor gene located in the 3p chromosome(11,12). The estimated incidence is 1:36,000 individuals, with penetrance > 90% after the age of 65. Characteristic tumors of this syndrome include central nervous system and retinal hemangioblastomas, clear cell renal carcinoma, pheochromocytoma, endolymphatic sac tumor, pancreatic cysts, epididymal and broad ligament papillary cystadenomas.(11). Diagnostic criteria include: 1) more than one central nervous system hemangioblastoma; 2) one central nervous system hemangioblastoma and vascular manifestation of von Hippel-Lindau syndrome. Hemangioblastoma is the most frequent tumor in this syndrome, affecting 60% to 80% of patients. Mean age at disease onset is 33 years. Varied symptoms are reported, depending on the lesion location, including headache, emesis, hyperreflexia, ataxia, dizziness, muscle strength loss and dysmetria(11,12). Association with polycythemia may be observed, as some hemangioblastomas produce erythropoietin(10,11). Mean life expectancy in these cases is 49 years(12) and the most frequent causes of death include clear cell renal carcinoma and neurological complications of cerebellar hemangioblastomas; for this reason several institutions recommend periodic screening with a range of protocols including imaging studies for asymptomatic von Hippel-Lindau syndrome patients(11,12). Hemangioblastomas are highly vascularized and frequently cystic lesions with a mural nodule. Commonly, such lesions are benign and multifocal and present association with edema or cysts developed along the neuroaxis as a result of transudation of solid components of the lesion, with a high protein content, and for this reason appearing slightly more hyperintense than the normal cerebrospinal fluid and quite hyperintense at T2-weighted images(10). Generally, they show hypo/isosignal at T1-weighted images and hypersignal at T2-weighted images, with enhancement of the solid portion of the lesion at contrast-enhanced T1-weighted images, sometimes with tubular flow-void in cases where the tumor is supplied or drained by large-caliber vessels. Hemangioblastomas are typically infratentorial. Only 5% to 30% of cerebellar hemangioblastomas are attributed to von Hippel-Lindau syndrome, while 80% of medullary hemangioblastomas are associated with this syndrome, in these cases, occurring at earlier ages and with poorer prognosis(12). At diffusion-weighted imaging, diffusion facilitation may be observed (hyposignal on DWI and hypersignal at ADC mapping), which, in the case of an infratentorial lesion, is highly suggestive of a diagnosis of hemangioblastoma(13). The patient was recalled for further investigation and abdominal computed tomography revealed multiple pancreatic cysts. REFERENCES 1. Ono SE, Carvalho Neto A, Gasparetto EL, et al. Adrenoleucodistrofia ligada ao X: correlação entre o escore de Loes e parâmetros do tensor de difusão. Radiol Bras. 2014;47:342-9. 2. Santana PC, Mourão AP, Oliveira PMC, et al. Dosimetria de pacientes submetidos a exames de PET/CT cerebral para diagnóstico de comprometimento cognitivo leve. Radiol Bras. 2014;47:350-4. 3. Castro FD, Reis F, Guerra JGG. Lesões expansivas intraventriculares à ressonância magnética: ensaio iconográfico - parte 1. Radiol Bras. 2014;47:176-81. 4. Castro FD, Reis F, Guerra JGG. Lesões expansivas intraventriculares à ressonância magnética: ensaio iconográfico - parte 2. Radiol Bras. 2014;47:245-50. 5. Carneiro Filho O, Vilela Filho O, Ragazzo PC, et al. Um novo método para a localização intraoperatória de foco de epilepsia mediante utilização de gamaprobe. Radiol Bras. 2014;47:23-7. 6. Carvalho GBS, Sandim GB, Tibana LAT, et al. Diagnóstico diferencial das lesões inflamatórias e infecciosas do cone medular utilizando a ressonância magnética. Radiol Bras. 2013;46:51-5. 7. Fiore L, Silva Junior NA, Bertanha R, et al. Fístula arteriovenosa dural intracraniana. Radiol Bras. 2013;46(4):xi-xii. 8. Reis F, Schwingel R, Nascimento FBP. Linfoma do sistema nervoso central: ensaio iconográfico. Radiol Bras. 2013;46:110-6. 9. Brandão LA. Linfoma primário e secundário do sistema nervoso central. Aspectos de imagem na ressonância magnética convencional e funcional. Radiol Bras. 2013;46(2):ix-x. 10. Ho VB, Smirniotopoulos JG, Murphy FM, et al. Radiologic-pathologic correlation: hemangioblastoma. AJNR Am J Neuroradiol. 1992;13:1343-52. 11. Kim JJ, Rini BI, Hansel DE. Von Hippel Lindau syndrome. Adv Exp Med Biol. 2010;685:228-49. 12. Leung RS, Biswas SV, Duncan M, et al. Imaging features of von Hippel-Lindau disease. Radiographics. 2008;28:65-79. 13. Quadery FA, Okamoto K. Diffusion-weighted MRI of haemangioblastomas and other cerebellar tumours. Neuroradiology. 2003;45:212-9. 1. MDs, Residents, Department of Radiology and Imaging Diagnosis, Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil 2. PhD, Teacher Responsible for the Division of Neuroradiology, Professor at Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil Mailing Address: Dr. Fabiano Reis Hospital de Clínicas da Universidade Estadual de Campinas (HC-Unicamp) Rua Vital Brasil, 251, Cidade Universitária Zeferino Vaz Campinas, SP, Brazil, 13083-888, Brazil E-mail: fabianoreis2@gmail.com |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554