Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 6 - Nov. / Dec. of 2014
Vol. 47 nº 6 - Nov. / Dec. of 2014
|
REVIEW ARTICLE
|
|
Bosniak classification for complex renal cysts: history and critical analysis |
|
|
Autho(rs): Valdair F. Muglia1; Antonio Carlos Westphalen2 |
|
|
Keywords: Renal cysts; Bosniak; Computed tomography; Magnetic resonance imaging. |
|
|
Abstract: INTRODUCTION
With the disseminated use of imaging methods for the investigation of abdominal diseases, the identification of incidental findings whose management is not always easy or consensual has become increasingly common. Complex renal cysts are fully representative of such a situation. In 1986 Morton Bosniak published a review article in which he suggested a classification and further management of cystic lesions of the kidneys based on findings on contrast-enhanced computed tomography (CT)(1). The classification was gradually adopted by imaging specialists and urologists, and is currently a reference in the field (Figure 1). 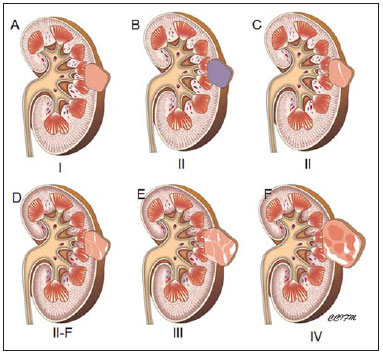 Figure 1. Illustration demonstrates the main findings in the Bosniak classification for renal cystic lesions. A: Category I. B and C: Category II, hyperdense on B. D: Category IIF. E: Category III. F: Category IV. However, in spite of the standardized description that was suggested by Bosniak, there remained a subjective component to the assessment of these lesions, in particular for distinguishing between minimally complex and benign lesions (Bosniak II) whose surgical approach is not mandatory, or complex and possibly malignant cysts (Bosniak III), for which surgical approach is recommended(2-5). In order to address this problem, a few years later Bosniak and his collaborators suggested the introduction of a fifth category, called II-F ("F" as follow-up), in his classification(6-8). The classification would undergo another small change in 2005(9), reaching its current format(10), which is shown in Table 1. According to the current classification, lesions in category I correspond to simple cysts without septa or vegetations, with thin and smooth walls, and no contrast enhancement after the administration of intravenous contrast agents (Figure 2A). Category II includes cysts with thin septations, minimally thick walls and fine parietal calcifications, and no contrast enhancement after intravenous contrast agent injection (Figure 2A). Homogeneous hyperdense cysts < 3.0 cm are included in this category. Lesions with irregular and/or thick septa, with course calcifications, and clear enhancement after intravenous contrast injection are described as category III (Figure 2B). Category IV is reserved for lesions with septa or walls with well-defined solid components that demonstrate contrast-enhancement after intravenous contrast injection (Figure 2C). Category II-F corresponds to indeterminate lesions with findings described on Table 1, which, although not sufficient to indicate surgical exploration, suggest a slight risk of malignancy (Figure 3). 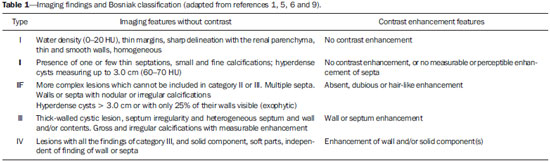 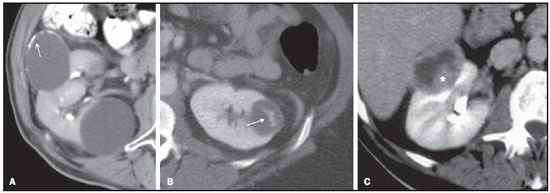 Figure 2. A: Categories I and II. Contrast-enhanced, axial CT section demonstrates a cyst with smooth and imperceptible walls, category I, and another with fine calcifications on its walls (arrow), category II, both without perceptible contrast-enhancement. B: Category III. Contrast-enhanced axial CT section demonstrates a cyst with smooth walls and a thin septum with perceptible and measurable enhancement after intravenous contrast injection (arrow). C: Category IV. Contrast-enhanced axial CT section demonstrates a mixed, thick-walled cystic-solid lesion with a solid component in the posterior wall (asterisk) that shows homogeneous enhancement after intravenous contrast injection.  Figure 3. Bosniak II-F cyst. Contrast-enhanced CT image shows a partially exophytic cyst with a fine septation inside. Subtle nodularity is observed in the septum, which has perceptible but not measurable contrast-enhancement (arrow). VALIDATION AND CONTROVERSIES Several studies, most retrospective, have evaluated the effectiveness of the Bosniak classification(11-15). A recent metaanalysis that included nine studies with at least 30 cases each(16) showed that the inclusion of the category II-F led to a reduction of the number of cases included in category III and, consequently, to a decrease in the number of surgical exploration of benign lesions. The negative predictive value of categories I and II remained the same(16). The percentage of malignant lesions in category I was 0%, 15.6% for category II, 0% for category II-F, 65.3% for category III, and 91.7% for category IV. The high frequency of malignant lesions in category II was driven by a single study in which two lesions were classified as Bosniak II and one was malignant(11). In another recent study, patients with cysts classified as II-F and III were followed either until proved stable or submitted to surgical resection(17). The frequency of malignant lesions was 25% and 54% for categories II-F and III, respectively. The authors have also observed that previous history of malignant renal neoplasia, and coexistence of malignant solid lesion, Bosniak category IV, or multiple Bosniak III cysts represent risk factors and increase the proportion of malignant lesions in cysts category III. Except for one study, the review of the most relevant articles (n > 30 patients) published until 2012 (Table 2) shows that one should expect a very low frequency of malignancy in category II-F. 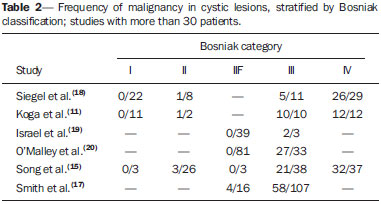 The introduction of category II-F has allowed for a more systematic approach to distinguish between categories II and III; however, there remains room for improvements, as findings that define a cyst as II-F are not always clearly noticeable. For example, in addition to being tenuous, the identification of enhancement in hair-like septa is subjective (Figure 3). It is widely known that experience and, mainly, the correlation with surgical exploration and histopathological findings improve the individual performance in the utilization of the Bosniak classification. The Bosniak classification suggests the necessity of follow-up of lesions classified as II-F, but it does neither establish an interval for imaging repetition nor the total follow-up duration period. This has led to distinctive approaches reported in recent publications(14,15,17). Bosniak himself recognizes the presence of heterogeneity among lesions in category II-F(9), some of which have lower risk of malignancy and require short-term imaging follow-up every six months for a two-year period; and others with more suspicious findings that are likely to benefit from longer follow-up period (up to four years) before being reclassified as category II, if stable(20-22). In the authors' experience, more suspicious lesions might be followed-up during the first year at shorter intervals (three to four months), alternating ultrasonography (US) and contrast-enhanced enhanced cross-sectional imaging (CT and magnetic resonance imaging - MRI), and every six months thereafter (Figure 4). In these instances, the observation of changes in the internal architecture of the complex cyst is equally or more important than the evaluation of its growth. 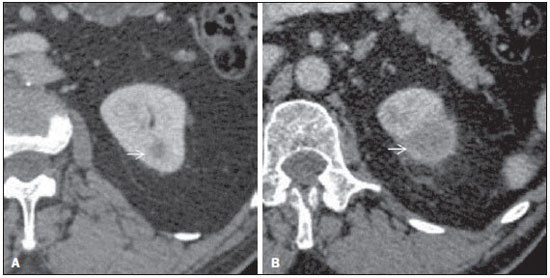 Figure 4. Progression of a complex cystic lesion. A: Contrast-enhanced CT. Initial study shows a small hypodense cortical lesion in the upper pole of the left kidney (arrow). B: Contrast-enhanced CT image acquired four months later. Despite the significant enlargement of the lesion (arrow), it was classified as Bosniak II-F. After another follow-up scan that demonstrated further increase in dimensions, the lesion was resected and a clear cell renal cell carcinoma was diagnosed. UTILIZATION OF OTHER DIAGNOSTIC METHODS: MRI AND US MRI has been widely used in the evaluation of cystic lesions in kidneys and other organs, usually with better performance than CT. In a study published in 2004, Bosniak recognized that the method is appropriate for his classification(23). MRI better demonstrates the presence of thin septa in cystic lesions, in particular within cysts < 2.0 cm). Yet, because of artifacts inherent to MR imaging, septa in renal cystic lesions may appear thicker than on CT (Figure 5). This may lead to disagreements, and lesions classified as II or II-F on CT might be classified as II-F or III on MRI(24). Additionally, less experienced observers tend to classify a higher number of lesions as II-F and III probably because of to the higher tissue and contrast resolution provided by MRI, possibly leading to a higher number of surgical explorations of benign lesions(22). 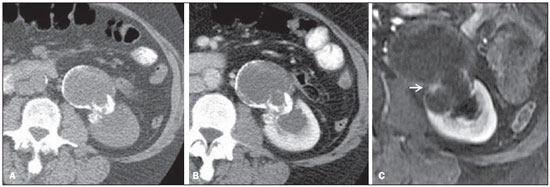 Figure 5. Evaluation of contrast enhancement at CT and MRI. A: Pre- and post-contrast, axial CT sections shows complex cyst with irregular walls and gross, parietal calcifications in the central region of the lesion. No defined enhancement is observed within the lesion. B: Post-gadolinium axial T1-weighted image with subtraction technique. Observe the nodular, irregular enhancement (arrow) adjacent to the calcifications. The lesion was reclassified as Bosniak IV and confirmed to be malignant. The enhancement of thin septa, described as capillary or hair-like enhancement, is much more conspicuous at MRI than at CT, providing greater confidence in their detection and for denying the absence of contrast-enhancement. This fact, however, is unlikely to change management the vast majority of lesions will be classified within category II, rather than I. Other advantage of MRI is the identification of contrast-enhancement of internal septa within hemorrhagic cysts(25). The high density of blood hinders the perception of contrast enhancement on CT, but subtraction techniques on MR imaging can bypass this situation (Figure 5). The use of ultrasound (US) in the Bosniak classification has never been unquestionably accepted, as the detection of neovascularization in malignant lesions, indicated by contrast enhancement of solid components, septa or walls, is a fundamental part of the classification(26,27). However, it is known that US may demonstrate internal septa better than CT and even MRI. Accordingly, it has been suggested that simple (Bosniak I) and minimally complex (Bosniak II) cysts may be followed with US only(28). Another potential advantage of US is its capacity of defining the cystic or solid nature of the lesion. In some situations, the characterization of remarkably hypovascular lesions may be difficult on CT (Figure 6). The papillary renal cell carcinoma is an example of such tumors(29) and its diagnosis may be difficult if the change in density between pre- and post-contrast phases approaches pseudoenhancement values (around 20 HU at 64-channel MDCT, and 10 HU at 16-channel MDCT)(30). In addition to their hypovascular nature, papillary tumors present cystic degeneration with a frequency similar to the clear cell variant. 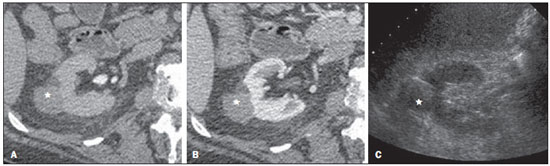 Figure 6. Value of ultrasonography. A,B: Axial CT sections shows homogeneously hypodense, exophytic, circumscribed lesion (asterisks) in the middle third of the left kidney, with questionable contrast enhancement (18 HU difference). C: Cross sectional US clearly demonstrates a solid lesion (asterisk) with some areas of sound beam attenuation. Papillary carcinoma was confirmed after surgical resection. Although not used to classify renal cystic lesions according to the Bosniak criteria, US can accurately indicate their degree of complexity and is an excellent method for the initial evaluation of patients with renal cystic lesions (Figure 7). 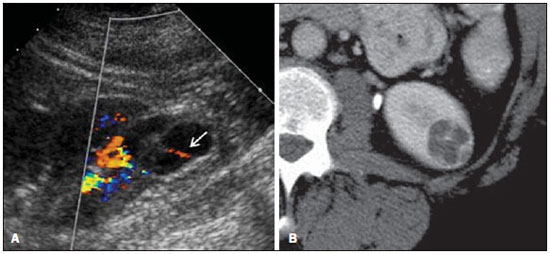 Figure 7. Ultrasonography. A: Sonographic section of the left kidney shows a cystic lesion with multiple septa inside, one of them with signal on color Doppler study (arrow). B: Contrast-enhanced axial MDCT section shows irregular septal enhancement. While not used to categorize lesions according to the Bosniak classification, the findings on US triggered further investigating and the lesion was confirmed to be a clear cell carcinoma. NEW PROSPECTS Recent studies have demonstrated that the use of intravenous sonographic contrast agent may allow for the detection of enhancement in complex cystic lesions, even in cases of very thin septa (hair-like enhancement), with an accuracy superior to CT(31). Limitations of such a technique include low reproducibility of the method, US operator dependence, and the cost of the contrast agent four times higher than the value of the iodinated contrast agent, a difference that might increase in cases of multiple cysts requiring repeated contrast injections. Other techniques have been employed in an attempt to improve the characterization of complex renal cystic lesions. Among them, diffusion-weighted MRI has attracted more attention. The method allows for indirect evaluation of the cellularity of neoplasms, and in complex cystic lesions, restricted diffusion in solid components was shown to have a high positive predictive value for cancer(32,33) (Figure 8). 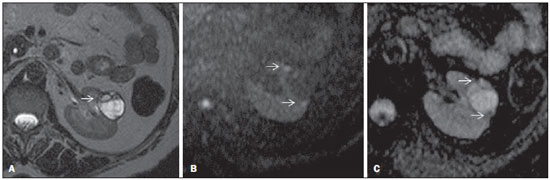 Figure 8. MRI and diffusion-weighted imaging (DWI). A: Axial T2-weighted image shows the presence of septa and solid contents on the anterior wall of the lesion (arrow). B,C: DWI and ADC mapping of the same lesion shows areas of water motion restriction identified as foci of high signal intensity at DWI and low signal on the ADC map (arrows). Note the significant difference favoring MRI in the characterization of complex cysts content. Clear cell renal cystic carcinoma was confirmed after resection In summary, the Bosniak classification has allowed for the standardization of the description and management of renal cystic lesions. Initially described for CT, the classification is now used with some advantages with MRI. The introduction of the intermediate category II-F has created conditions to reduce the number benign lesions treated with surgery. Although not utilized to determine the Bosniak classification, ultrasound remains as an excellent method for detecting and defining the complexity of cystic lesions. REFERENCES 1. Bosniak MA. The current radiological approach to renal cysts. Radiology. 1986;158:1-10. 2. Cloix P, Martin X, Pangaud C, et al. Surgical management of complex renal cysts: a series of 32 cases. J Urol. 1996;156:28-30. 3. Wilson TE, Doelle EA, Cohan RH, et al. Cystic renal masses: a reevaluation of the usefulness of the Bosniak classification system. Acad Radiol. 1996;3:564-70. 4. Aronson S, Frazier HA, Baluch JD, et al. Cystic renal masses: usefulness of the Bosniak classification. Urol Radiol. 1991;13:83-90. 5. Bosniak MA. Difficulties in classifying cystic lesions of the kidney. Urol Radiol. 1991;13:91-3. 6. Bosniak MA. Problems in the radiologic diagnosis of renal parenchymal tumors. Urol Clin North Am. 1993;20:217-30. 7. Bosniak MA. Diagnosis and management of patients with complicated cystic lesions of the kidney. AJR Am J Roentgenol. 1997;169: 819-21. 8. Bosniak MA. The use of the Bosniak classification system for renal cysts and cystic tumors. J Urol. 1997;157:1852-3. 9. Israel GM, Bosniak MA. An update of the Bosniak renal cyst classification system. Urology. 2005;66:484-8. 10. Israel GM, Bosniak MA. How I do it: evaluating renal masses. Radiology. 2005;236:441-50. 11. Koga S, Nishikido M, Inuzuka S, et al. An evaluation of Bosniak's radiological classification of cystic renal masses. BJU Int. 2000;86: 607-9. 12. Harisinghani MG, Maher MM, Gervais DA, et al. Incidence of malignancy in complex cystic renal masses (Bosniak category III): should imaging-guided biopsy precede surgery? AJR Am J Roentgenol. 2003;180:755-8. 13. Warren KS, McFarlane J. The Bosniak classification of renal cystic masses. BJU Int. 2005;95:939-42. 14. O'Malley RL, Godoy G, Hecht EM, et al. Bosniak category IIF designation and surgery for complex renal cysts. J Urol. 2009;182:1091-5. 15. Song C, Min GE, Song K, et al. Differential diagnosis of complex cystic renal mass using multiphase computerized tomography. J Urol. 2009;181:2446-50. 16. Graumann O, Osther SS, Oster PJ. Characterization of complex renal cysts: a critical evaluation of the Bosniak classification. Scand J Urol Nephrol. 2011;45:84-90. 17. Smith AD, Remmer EM, Cox KL, et al. Bosniak category IIF and III cystic renal lesions: outcomes and associations. Radiology. 2012;262:152-60. 18. Siegel CL, McFarland EG, Brink JA, et al. CT of cystic renal masses: analysis of diagnostic performance and interobserver variation. AJR Am J Roentgenol. 1997;169:813-8. 19. Israel GM, Bosniak MA. Follow-up CT of moderately complex cystic lesions of the kidney (Bosniak category IIF). AJR Am J Roentgenol. 2003;181:627-33. 20. O'Malley RL, Godoy G, Hecht EM, et al. Bosniak category IIF designation and surgery for complex renal cysts. J Urol. 2009;182: 1091-5. 21. Hwang JH, Lee CK, Yu HS, et al. Clinical outcomes of Bosniak category IIF complex renal cysts in Korean patients. Korean J Urol. 2012;53:386-90. 22. Lang EK, Macchia RJ, Gayle B, et al. CT-guided biopsy of indeterminate renal cystic masses (Bosniak 3 and 2F): accuracy and impact on clinical management. Eur Radiol. 2002;12:2518-24. 23. Israel GM, Hindman N, Bosniak MA. Evaluation of cystic renal masses: comparison of CT and MR imaging by using the Bosniak classification system. Radiology. 2004;231:365-71. 24. Weibl P, Klatte T, Kollarik B, et al. Interpersonal variability and present diagnostic dilemmas in Bosniak classification system. Scand J Urol Nephrol. 2011;45:239-44. 25. Kim WB, Lee SW, Doo SW, et al. Category migration of renal cystic masses with use of gadolinium-enhanced magnetic resonance imaging. Korean J Urol. 2012;53:573-6. 26. Ascenti G, Mazziotti S, Zimbaro G, et al. Complex cystic renal masses: characterization with contrast-enhanced US. Radiology. 2007;243: 158-65. 27. Park BK, Kim B, Kim SH, et al. Assessment of cystic renal masses based on Bosniak classification: comparison of CT and contrast-enhanced US. Eur J Radiol. 2007;61:310-4. 28. McGuire BB, Fitzpatrick JM. The diagnosis and management of complex renal cysts. Curr Opin Urol. 2010;20:349-54. 29. Vikram R, Ng CS, Tamboli P, et al. Papillary renal cell carcinoma: radiologic-pathologic correlation and spectrum of disease. Radio-graphics. 2009;29:741-54. 30. Sai V, Rakow-Penner R, Yeh BM, et al. Renal cyst pseudoenhancement at 16- and 64-dector row MDCT. Clin Imaging. 2013;37:520-5. 31. Quaia E, Bertolotto M, Cioffi V, et al. Comparison of contrast-enhanced sonography with unenhanced sonography and contrast-enhanced CT in the diagnosis of malignancy in complex cystic renal masses. AJR Am J Roentgenol. 2008;191:1239-49. 32. Inci E, Hocaoglu E, Aydin S, et al. Diffusion-weighted magnetic resonance imaging in evaluation of primary solid and cystic renal masses using the Bosniak classification. Eur J Radiol. 2012;81:815-20. 33. Sandrasegaran K, Sundaram CP, Ramaswamy R, et al. Usefulness of diffusion-weighted imaging in the evaluation of renal masses. AJR Am J Roentgenol. 2010;194:438-45. 1. Fellow PhD degree, Associate Professor, Department of Medical Practice, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP) – Centro de Ciências da Imagem e Física Médica (CCIFM), Ribeirão Preto, SP, Brazil 2. PhD, Associate Professor of Radiology, Department of Radiology and Biomedical Imaging – University of California, San Francisco (UCSF), San Francisco, CA, USA Mailing Address: Dr. Valdair F. Muglia FMRP-USP – CCIFM Avenida Bandeirantes, 3900, Campus Universitário, Monte Alegre Ribeirão Preto, SP, Brazil, 14048-900 Email: fmuglia@fmrp.usp.br Received May 10, 2013. Accepted after revision January 8, 2014. Study developed at Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil, and at University of California at San Francisco (UCSF) – School of Medicine, San Francisco, CA, USA. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554