Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 5 - Sep. / Oct. of 2014
Vol. 47 nº 5 - Sep. / Oct. of 2014
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Bruno Hochhegger1; Klaus Loureiro Irion2; Arthur Soares Souza Junior3; Adalberto Sperb Rubin1; Gláucia Zanetti4 |
|
|
A 23-year-old, male drugs user presenting with dry cough and progressive dyspnea to medium/great stress. Posteroanterior chest radiography and chest computed tomography were performed (Figure 1).
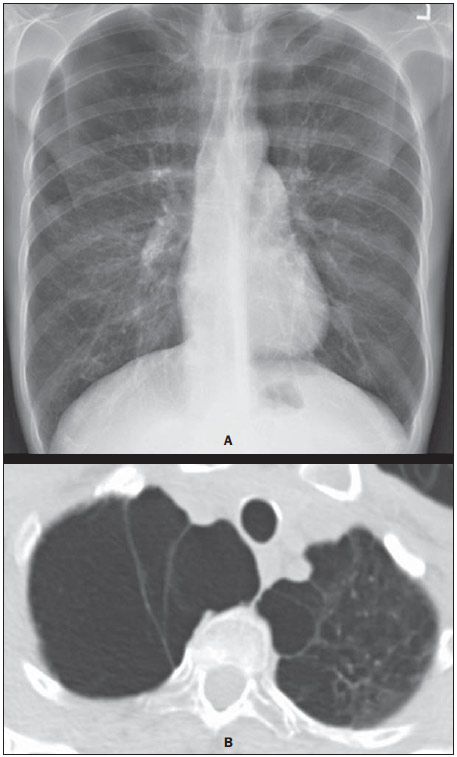 Figure 1. A: Posteroanterior chest radiographic image. B: Computed tomography – pulmonary parenchyma window. Section at the level of the upper lung lobes. Image description Figure 1. Posteroanterior chest radiography and chest computed tomography showing bullous emphysema in the upper portions of the lungs, predominantly at right. Diagnosis: Bullous emphysema in a smoking cocaine (crack) user. COMMENTS The imaging evaluation of the respiratory system has been the object of a series of recent publications in the Brazilian radiological literature(1-16). Chest computed tomography (CT) has revolutionized the application of imaging methods in many aspects of pneumology and thoracic surgery. The use of CT in the investigation lung cancer, interstitial diseases and emphysema is already part of the routine in pneumological investigation. However, the potential of the method has been sub-utilized in cases of emphysema. As a routine, the use of CT remains restricted to the purpose of diagnostic confirmation and subjective analysis of the extent and type of emphysematous lesions(17-26). Currently, multidetector CT is available in most diagnostic imaging centers. Such CT apparatuses have allowed chest CT scans with acquisition of all the images during a single breathhold. Such a technical feature has opened new avenues for the investigation of lung diseases. Objective measurements of the total pulmonary volume and of the volume of the lung affected by emphysema can be performed with high accuracy(27-36). The quantification of emphysema by CT densitovolumetry(27,37) is a process where areas of the lung with predetermined density values or with attenuation below a determined threshold are depicted in a solid color, so as the observer can immediately identify those areas with altered pulmonary density or emphysema. In 1995, It was suggested that a threshold corresponding to -950 UH was fixed to differentiate a healthy lung from an emphysematous lung (emphysema quantification)(38), so this value is most frequently utilized. With the introduction of helical CT, it became possible to calculate the actual volume (cm3) instead of the area (cm2), so the volumetric quantification of emphysema by CT was introduced. Such technique has allowed the early diagnosis as well as the monitoring of these patients(21,28,31). Such pioneering studies have inspired many other authors who expanded the clinical application of CT beyond the subjective analysis of anatomical aspects on images. Nowadays, it is recognized that CT densitovolumetry is more accurate and sensitive than the traditional pulmonary function tests and is considered the method of choice for noninvasive and accurate evaluation of pathological alterations in emphysema, demonstrating good correlation with histopathological results(39). The use of illicit drugs may cause lungs injury by different mechanisms. One of such mechanisms is the intravenous injection of medicines originally intended for oral administration, causing pulmonary talcosis or emphysema. In general, some drug users grind medicine tablets down, dissolve them with water and inject such a solution intravenously(40-42). Such oral medications have in common the addition of an insoluble mean (talc, cellulose or starch) to bind medicinal particles together and act as a lubricant preventing tablets from sticking either to machinery or to each other during production(40,41). Thus, the substance injection results in microscopic pulmonary emboli(40,42). The particles may migrate to the interstitium, causing a foreign-body-type granulomatous reaction(40,42). It seems that the talc directly injected in the vascular system is the most relevant mechanism in the development of emphysema. The physiopathological explanation is still unclear, but whatever the involved mechanism is, emphysema is an extremely relevant element in the physiopathology of some forms of pulmonary talcosis(40,42). At CT, the main difference between the inhalatory and intravenous (related to the use of intravenously injected oral drugs) forms of talcosis is the development of emphysema in the latter, predominantly affecting the lower lobes. The significantly increased prevalence of panacinar emphysema in the lower lung lobes is observed in intravenous drugs-addicted patients who inject metylphenidate (Ritalin)(41,43,44). Such a disease pattern is similar to the emphysema described in patients with alpha-1 antitrypsin deficiency(42,44). Emphysema is the only finding in some Ritalin users. Barotrauma is another complication resulting from the habit of smoking crack or inhaling cocaine(45,46). Such a condition may manifest as pneumothorax, pneumomediastinum, pneumopericardium or subcutaneous emphysema(45,47). In cocaine users, increased intrathoracic pressure may be observed during the smoking act due to vigorous coughing or intentional production of a Valsalva maneuver to increase the drug absorption and maximize its effects(46). Overdistention of the alveoli may cause their rupture and escape of air into the interstitium and, eventually, to the mediastinum, producing pneumomediastinum(45,48). Vigorous aspiration following cocaine inhalation may cause pneumomediastinum by a similar mechanism(46,49). Barotrauma is generally diagnosed by chest radiography, but CT may be useful in the diagnosis in cases where radiography is not conclusive. In young individuals, the presence of air in the mediastinum should raise the suspicion of cocaine use in the absence of other etiological factors(45). Emphysema has also been reported in smoked or inhaled drug users, generally affecting young men. Some studies have described the presence of severe bullous alterations associated with cocaine smoking. CT can identify bullae and centrilobular emphysema in the upper lung lobes, particularly in the periphery, sparing the central regions of the lungs(45,47), as observed in the present case. REFERENCES 1. Yamanari MGI, Mansur MCD, Kay FU, et al. Bullet embolism of pulmonary artery: a case report. Radiol Bras. 2014;47:128-30. 2. Zanetti G, Nobre LF, Mançano AD, et al. Pulmonary paracoccidioidomycosis. Radiol Bras. 2014;47(1):xi-xiii. 3. Fernandes MC, Zanetti G, Hochhegger B, et al. Rhodococcus equi pneumonia in an AIDS patient. Radiol Bras. 2014;47(3):xi-xiii. 4. Mançano AD, Santos Neto RC, Silva KCC. Williams-Campbell syndrome. Radiol Bras. 2014;47(2):xi-xii. 5. Ceratti S, Pereira TR, Velludo SF, et al. Pulmonary tuberculosis in a patient with rheumatoid arthritis undergoing immunosuppressive treatment: case report. Radiol Bras. 2014;47:60-2. 6. Bispo IGA, Nascimento DT, Ferreira KO, et al. Brain metastasis as initial presentation of papillary adenocarcinoma of the lung: case report. Radiol Bras. 2013;46:313-6. 7. Eifer DA, Arsego FV, Torres FS. Unilateral pulmonary veins atresia: evaluation by computed tomography. Radiol Bras. 2013;46:376-8. 8. Amorim VB, Rodrigues RS, Barreto MM, et al. Computed tomography findings in patients with H1N1 influenza A infection. Radiol Bras. 2013;46:299-306. 9. Carneiro DS, Arantes JH, Souza GV, et al. Heterotaxy syndrome: a case report. Radiol Bras. 2013;46:181-3. 10. Zanetti G, Nobre LF, Mançano AD, et al. Nodular reversed halo sign caused by pulmonary tuberculosis, confirmed by sputum culture. Radiol Bras. 2013;46(6):ix-x. 11. Costa AN, Giassi KS, Bachion GH, et al. Post-traumatic pulmonary pseudocyst in a soccer player: a case report. Radiol Bras. 2013;46:122-4. 12. Amoedo MK, Souza LVS, Souza AS, et al. Pulmonary interstitial emphysema: a case report and review of the literature. Radiol Bras. 2013;46:317-9. 13. Souza VF, Chaves RT, Balieiro VS, et al. Qualitative and quantitative pulmonary density analysis in a patient with polymyositis and pulmonary fibrosis. Radiol Bras. 2013;46(3):ix-x. 14. Pereira e Silva JL. The virus-drug-host dynamics in the tomographic characterization of pulmonary influenza A (H1N1) infection - a clinical-radiological-pathological view. Radiol Bras. 2013;46(5):vii-ix. 15. Canellas R, Kanaan D, Martins PHR, et al. Spontaneous regression of pulmonary alveolar proteinosis: a case report. Radiol Bras. 2012;45:294-6. 16. Bozi LCF, Melo ASA, Marchiori E. Pulmonary metastatic calcification: a case report. Radiol Bras. 2012;45:297-9. 17. Irion KL, Hochhegger B, Marchiori E, et al. Radiograma de tórax e tomografia computadorizada na avaliação do enfisema pulmonar. J Bras Pneumol. 2007;33:720-32. 18. Hochhegger B, Dixon S, Screaton N, et al. Emphysema and smoking-related lung diseases. Imaging. 2008;20:219-35. 19. Irion KL, Marchiori E, Hochhegger B. Tomographic diagnosis of pulmonary emphysema. J Bras Pneumol. 2009;35:821-3. 20. Hochhegger B, Irion KL, Andrade CF, et al. Congenital lobar emphysema: the role of multislice computed tomography with virtual bronchoscopy in the differential diagnosis with bronchial foreign bodies. Eur Arch Otorhinolaryngol. 2012;269:2015-6. 21. Hochhegger B, Alves GR, Irion KL, et al. Emphysema index in a cohort of patients with no recognizable lung disease: influence of age. J Bras Pneumol. 2012;38:494-502. 22. Hochhegger B, Souza G, Meireles GP, et al. The chest and aging: radiological findings. J Bras Pneumol. 2012;38:656-65. 23. Hochhegger B, Irion KL. Chest radiography and COPD. Radiol Bras. 2013;46(6):v-vi. 24. Marcos L, Bichinho GL, Panizzi EA, et al. Classification of chronic obstructive pulmonary disease based on chest radiography. Radiol Bras. 2013;46:327-32. 25. Irion KL, Hochhegger B. Emphysema: diagnosis, classification, quantification and treatment planning. Radiol Bras. 2013;46(1):ix. 26. Koenigkam-Santos M, Paula WD, Gompelmann D, et al. Endobronchial valves in severe emphysematous patients: CT evaluation of lung fissures completeness, treatment radiological response and quantitative emphysema analysis. Radiol Bras. 2013;46:15-22. 27. Hochhegger B, Marchiori E, Irion K, et al. Accuracy of measurement of pulmonary emphysema with computed tomography: relevant points. Radiol Bras. 2010;43:260-5. 28. Irion KL, Marchiori E, Hochhegger B, et al. CT Quantification of emphysema in young subjects with no recognizable chest disease. AJR Am J Roentgenol. 2009;192:W906. 29. Hochhegger B, Irion KL, Marchiori E, et al. Reconstruction algorithms and their influence in emphysema CT measurements. Acad Radiol. 2010;17:674. 30. Hochhegger B, Marchiori E, Irion KL, et al. Are we measuring pulmonary emphysema? Respir Med. 2010;104:1073. 31. Hochhegger B, Irion KL, Marchiori E, et al. Reconstruction algorithms influence the follow-up variability in the longitudinal CT emphysema index measurements. Korean J Radiol. 2011;12:169-75. 32. Hochhegger B, Marchiori E, Irion K, et al. Visual vs automated assessment of emphysema. Chest. 2011;140:1384. 33. Hochhegger B, Marchiori E, Irion KL, et al. Iodinated contrast media and its influence in emphysema CT measurements. Clin Imaging. 2012;36:160. 34. Hochhegger B, Irion KL, Marchiori E. Reconstruction algorithms and CT emphysema measurements. Radiology. 2012;263:935-6. 35. Hochhegger B, Irion KL, Alves GRT, et al. Normal variance in emphysema index measurements in 64 multidetector-row computed tomography. J Appl Clin Med Phys. 2013;14:4215. 36. de Castro MC, Ferreira AS, Irion KL, et al. CT quantification of large opacities and emphysema in silicosis: correlations among clinical, functional, and radiological parameters. Lung. 2014;192:543-51. 37. Müller NL, Staples CA, Miller RR, et al. "Density mask". An objective method to quantitate emphysema using computed tomography. Chest. 1988;94:782-7. 38. Gevenois PA, de Maertelaer V, De Vuyst P, et al. Comparison of computed density and macroscopic morphometry in pulmonary emphysema. Am J Respir Crit Care Med. 1995;152:653-7. 39. Newell JD Jr, Hogg JC, Snider GL. Report of a workshop: quantitative computed tomography scanning in longitudinal studies of emphysema. Eur Respir J. 2004;23:769-75. 40. Souza Jr AS, Marchiori E, Irion KL, et al. Talcose pulmonar associada ao uso endovenoso de medicamentos orais. Radiol Bras. 2003;36:187-90. 41. Paré JP, Cote G, Fraser RS. Long-term follow-up of drug abusers with intravenous talcosis. Am Rev Respir Dis. 1989;139:233-41. 42. Ward S, Heyneman LE, Reittner P, et al. Talcosis associated with IV abuse of oral medications: CT findings. AJR Am J Roentgenol. 2000;174:789-93. 43. Marchiori E, Franquet T, Gasparetto TD, et al. Consolidation with diffuse or focal high attenuation: computed tomography findings. J Thorac Imaging. 2008;23:298-304. 44. Marchiori E, Lourenço S, Gasparetto TD, et al. Pulmonary talcosis: imaging findings. Lung. 2010;188:165-71. 45. de Almeida RR, de Souza LS, Mançano AD, et al. High-resolution computed tomographic findings of cocaine-induced pulmonary disease: a state of the art review. Lung. 2014;192:225-33. 46. Kloss BT, Broton CE, Rodriguez E. Pneumomediastinum from nasal insufflation of cocaine. Int J Emerg Med. 2010;3:435-7. 47. Restrepo CS, Carrillo JA, Martínez S, et al. Pulmonary complications from cocaine and cocaine-based substances: imaging manifestations. Radiographics. 2007;27:941-56. 48. Gotway MB, Marder SR, Hanks DK, et al. Thoracic complications of illicit drug use: an organ system approach. Radiographics 2002;22 Spec No:S119-35. 49. Mançano A, Marchiori E, Zanetti G, et al. Pulmonary complications of crack cocaine use: high-resolution computed tomography of the chest. J Bras Pneumol. 2008;34:323-7. 1. Medical Imaging Research Laboratory of Universidade Federal de Ciências da Saúde de Porto Alegre and Santa Casa de Porto Alegre, Porto Alegre, RS, Brazil 2. Royal Liverpool University Hospital, Liverpool, England 3. Faculdade de Medicina de São José do Rio Preto (Famerp) and Ultra-X, São José do Rio Preto, SP, Brazil 4. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil Mailing Address: Dr. Bruno Hochhegger Rua General Neto, 315/404, Floresta Porto Alegre, RS, Brazil, 90560-020 E-mail: brunohochhegger@gmail.com Study developed at the Medical Imaging Research Laboratory of Universidade Federal de Ciências da Saúde de Porto Alegre and Santa Casa de Porto Alegre, Porto Alegre, RS, Brazil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554