Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 4 - July / Aug. of 2014
Vol. 47 nº 4 - July / Aug. of 2014
|
ORIGINAL ARTICLE
|
|
Evaluation of non-radiologist physicians' knowledge on aspects related to ionizing radiation in imaging |
|
|
Autho(rs): Renata Rodrigues Madrigano1; Karen Cristine Abrão2; Andrea Puchnick3; Rodrigo Regacini4 |
|
|
Keywords: Ionizing radiation; Knowledge; Physicians; Imaging diagnosis; Radiation protection; Questionnaire. |
|
|
Abstract: INTRODUCTION
Medical applications comprise most of the artificial radiation sources which humans are exposed to, and radiological examinations lead the list of such sources(1). Ionizing radiations are utilized in radiography, fluoroscopy, angiography and computed tomography (CT) besides nuclear medicine examinations, and the dose depends on factors related to the patients (age and size), technical factors (equipment parameters and procedure duration) as well as equipment model(2). Ionizing radiation may lead to several undesirable effects on the exposed individuals, particularly increased lifetime risk for cancer(3). Thus, methods relying on ionizing radiations should be rationally utilized, taking their risks and benefits into consideration, and whenever possible, preference should be given to methods that do not rely on ionizing radiation, and to the utilization of the minimum dose required to solve the clinical doubt. The knowledge on ionizing radiation doses in radiology, their potential carcinogenic effects, as well as their rational utilization, is very heterogeneous among physicians(4,5). Some specialties have a more intense participation in scientific discussions on ionizing radiation, either during residency, in radiology, or in daily practice, for frequently requesting radiological studies(5). Multidisciplinary clinical meetings, congresses, or any other form of continued education can also increase the exposure of physicians to information on ionizing radiation. The preoccupation with the medical community inappropriate knowledge on radiation doses in imaging examinations keeps increasing in the literature(5–11). Requesting physicians have great responsibility on the effective, rational utilization of such methods. In this scenario, a questionnaire was applied to non-radiologist physicians in order to evaluate their knowledge on the rational utilization of imaging methods, and to raise a brief discussion on the most relevant points of the theme. MATERIALS AND METHODS Cross-sectional study, duly approved by the Committee for Ethics in Research, undertaken on the second semester of 2012, including an anonymous questionnaire applied to non-radiologist physicians in clinical and surgical specialties involved in ambulatory and hospital practice. All participants signed a term of free and informed consent. The questionnaire was divided into two parts: the first part comprising questions on the characteristics of the groups of participating physicians (age, gender, specialty, academic degree, and time in the profession), frequency of imaging studies requests and frequency of participation in professional update events; and the second part comprising multiple choice questions approaching three large knowledge fields: general knowledge, radioprotection principles and optimization principles – specially the ALARA (as low as reasonably achievable) principle. The frequency of imaging studies requests and participation in professional update events was graded in a scale of 0 to 4 points, where: 0 = never; 1 = rarely; 2 = not frequent; 3 = frequent; 4 = very frequent. Professional update events were divided into clinical meetings, participation in congresses, specialty courses, teaching activities, and research activities. The imaging studies whose request frequency was evaluated, were the following: conventional radiography, contrast-enhanced radiography and CT. Among the questions on general knowledge, the first one included a list of multiple imaging methods, including those which utilize non-ionizing radiation. The next two questions involved the knowledge on relative dose of ionizing radiation. The questions on the ALARA principle involved the application of the concept with practical examples, without questioning the definition itself. On the questions about radioprotection, the knowledge on how to protect from ionizing radiation, as well as the risks for development of cancer related to radiation was approached. The utilization of radiological methods in pediatrics and in pregnant women was also approached. For the statistical analysis, the Statistic Package for Social Sciences for Windows, release 16.0 was utilized. The questions which were not responded, or for which more than one alternative was selected when more than one selection was not permitted, were invalidated and, therefore, excluded from the statistical analysis. The results were expressed in mean and standard deviation for the quantitative variables and in number and percentage for the categorical variables. The Student's t test was utilized for comparison of the quantitative variables and the exact Fisher's test was utilized for comparing the categorical variables. The value of p < 0.05 was considered as being statistically significant. RESULTS A total of 120 (38.8%) out of 309 distributed questionnaires were responded. From the total of participating physicians, 62 (51.7%) had completed medical residency, 40 (33.3%) were specialists, 11 (9.2%) had a master's degree, 1 (0.8%) post-doctorate degree, 1 (0.8%) was a private docent, 5 (4.2%) were only graduates and no doctorates, distributed in different clinical and surgical specialties (Tables 1 and 2). 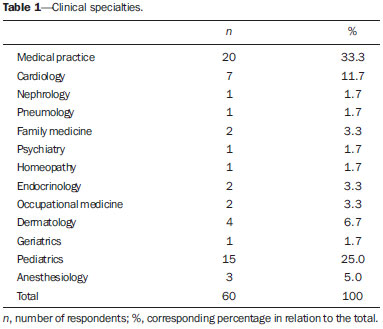 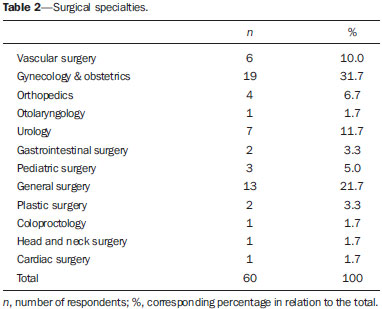 Mean time of professional practice was 12.69 ± 12.15 years, ranging from 1 to 47 years. Mean frequency of participation in professional update events was 2.81 ± 0.93 for clinical meetings, 2.43 ± 0.96 for participation in congresses, 2.43 ± 0.98 for specialty courses, 2.02 ± 1.39 for teaching activities, and 1.60 ± 1.16 for research activities. Mean frequency of imaging studies requests was 3.03 ± 1.08 for conventional radiography, 1.73 ± 1.22 for contrast-enhanced radiography, and 2.48 ± 1.14 for CT. The mean score was 6.77 ± 1.04, ranging from 3.81 to 9.52. The participating physicians were asked questions on their general knowledge (Tables 3 and 4), on radiation and, as shown on Table 3, 45% (n = 54) of the physicians indicated magnetic resonance imaging (MRI) and 2.5% (n = 3) ultrasonography (US) as imaging methods that utilize ionizing radiation. The participants were also questioned about optimization principles (Table 5) and on several topics related to radioprotection (Tables 6, 7 and 8). 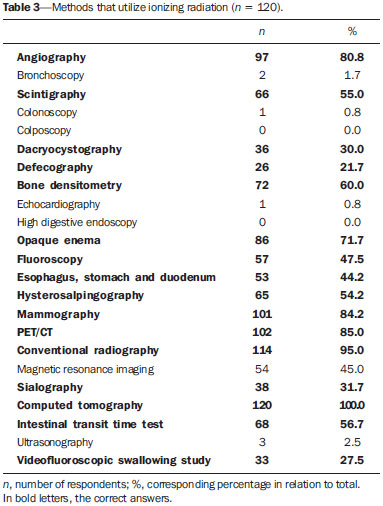 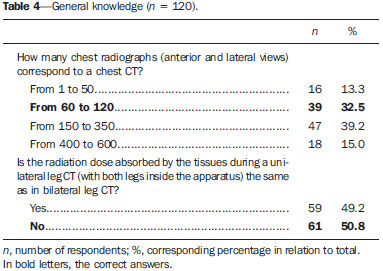 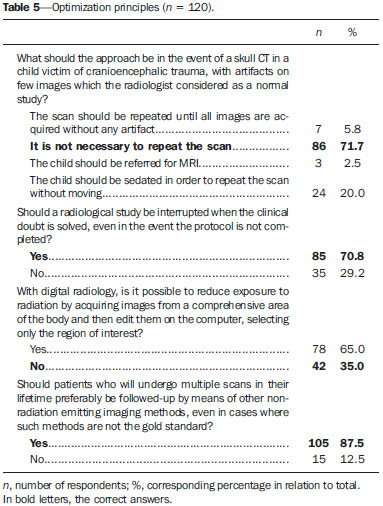 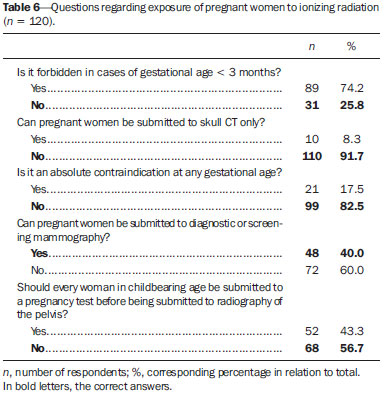 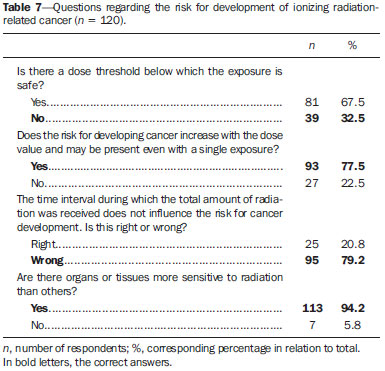 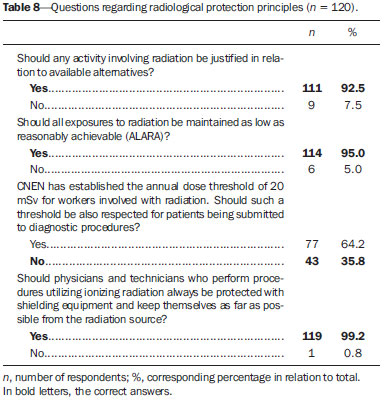 As the medical specialties were compared, the authors observed that the knowledge about ionizing radiation is greater in the surgical specialties, but without any significant differences, with the exception for the question on radiation exposure in pregnant women. The average score (6.33 ± 2.15) for the surgical specialties regarding that question was statistically superior to the average score for the clinical specialties (5.53 ± 2.22) (p = 0.047). Thirty one physicians (25.8%) in surgical specialties correctly responded that pregnant women can undergo diagnostic or screening mammography, as compared with the 17 (14.2%) clinicians (p = 0.015), and 41 (35.2%) of the physicians in surgical specialties who correctly responded that there is no need for every woman in childbearing age for undergoing pregnancy tests before being submitted to radiography of the pelvis, as compared with 27 (22.5%) clinicians (p = 0.016). The physicians with a higher mean frequency of participation in professional update events demonstrated statistically superior knowledge on ionizing radiation, in comparison with the other physicians, particularly in relation to correct answers on the methods which utilize ionizing radiation, such as dacryocystography (p = 0.046), defecography (p = 0.037), opaque enema (p = 0.047), esophagus, stomach and duodenum (p = 0.021), mammography (p = 0.049), sialography (p = 0.002), intestinal transit time test (p = 0.003), and videofluoroscopic swallowing study (p = 0.009). Among the 120 participating physicians, 91.7% regularly participate in clinical meetings, 83.3% participate in congresses, 85% attend specialty courses, 60.8% participate in teaching activities, and 49.2 participate in research activities. The mean score of the physicians who attend clinical meetings was statistically superior to those who don't (6.82 ± 1.03 versus 6.17 ± 0.98; p = 0.050), as well as the mean score of those who participate in teaching activities as compared with those who don't (6.92 ± 1.03 versus 6.54 ± 1.01; p = 0.047). The same was observed in relation to the mean scores for questions regarding general knowledge, both for physicians who attend clinical meetings (6.81 ± 1.40 versus 5.64 ± 1.47; p = 0.013) and those who participate in teaching activities (6.96 ± 1.32 versus 6.31 ± 1.53; p = 0.015). Among the 66 respondents (55%) who knew that MRI does not utilize ionizing radiation, 60 (50%) participated in congresses (p = 0.025). DISCUSSION The preoccupation with the knowledge that non-radiologist physicians have on radiation doses involved in radiological procedures is increasing in the literature, and previous studies have demonstrated that such knowledge is inappropriate(5–11). The applied questionnaire was not based on formal concepts or on absolute values of ionizing radiation dose, like in the case of most studies in the literature, but rather on clinical situations of the daily practice. From the obtained data, it is possible to realize that the very concept of ionizing radiation is insufficient among non-radiologist physicians, as 45% and 2.5% of the physicians responded, respectively, that MRI and US are imaging methods that utilize ionizing radiation. One should highlight the fact that a relatively high number of physicians who selected MRI, as such method is an excellent alternative to reduce exposure to ionizing radiation in certain cases, and, without such knowledge, the utilization of the method as an alternative may be impaired. On account of the fact that the questionnaire did not approach formal definitions or absolute values of radiation doses, one considered that the mean value of the scores was relatively high (6.77 ± 1.04 [3.81–9.52]), without statistically significant differences among clinical and surgical specialties. Among the surgical specialties, 31.7% were from gynecology and obstetrics, a fact that may have contributed for the higher number of correct answers related to the exposure of pregnant women, which was statistically significant (p = 0.047). There was a statistical significant correlation between professional updating and correct answers in parts of the questionnaire, as well as of the higher mean score value of the physicians who attend clinical meetings (p = 0.050) and participate in teaching activities (p = 0.047). The knowledge on medical physics and ionizing radiations is part of the academic formation of radiologists. For the other specialties evaluated in the present study, it was possible to observe that great part of such knowledge is acquired in multidisciplinary clinical meetings, congresses, teaching and research activities. The time spent in professional practice and frequency of exam requests did not demonstrate any significant correlation. Although most of the respondents have returned the questionnaires promptly, others did it after a few days, which may have allowed such respondents to seek correct answers in other sources. This may be considered a bias factor in the method. Additionally, there was difficulty in retrieving the handed out questionnaires and in applying them to a greater number of physicians, probably due to the fact that the questionnaire approached knowledge on a theme that is still poorly explored formally. Ionizing radiation comprises electromagnetic waves which upon interaction with matter unleashes a series of ionizations, transferring energy to atoms and molecules present in the irradiated field and promoting intracellular physical and chemical changes(3). The amount of energy (in Joules) deposited by radiation on matter per mass unit (in kilograms) refers to the concept of "absorbed dose", whose unit in the International System of Measurements is the gray (Gy). The concept of absorbed dose is adopted for any type of ionizing radiation, and not only for x-rays. Different types of ionizing radiations produce different biological effects. For utilization in radiological exams, the most appropriate concept is that of "equivalent dose", which takes into consideration the type of radiation involved in the exposure, by means of a correction factor applied to the value of the absorbed dose. The quantity utilized for equivalent dose is the unit sievert (Sv). For x-rays, the correction factor is equal to 1 and, therefore, 1 Gy is numerically equal to 1 Sv(3,12). The biological effects caused by high energy ionizing radiation can be divided into deterministic and stochastic effects. Deterministic effects, or tissue reactions, are characteristic of the high doses and depend directly on such an exposure, as cellular death (for example, of malignant cells submitted to radiotherapy), skin burns, sterility or occurrence of cataracts(13,14). For low doses, the risks are primarily for stochastic (or random) effects which are those that are not apparent and manifest after months or years from the exposure to radiation, thus not allowing for the clear establishment of a cause-and-effect relationship, but rather only the probability of occurrence, which is proportional to the dose. The most relevant stochastic effects are mutations and carcinogenesis(3,14,15). For stochastic effects, one considers that there is a dose-response linear component, without a limit below which the exposure is safe, i.e., any radiation dose has the probability of causing mutation or cancer(15). On the basis of such a concept, several mathematical models are utilized to extrapolate the experience of Japanese survivors of atom bombs explosion (exposed to moderate and high radiation doses) and to estimate the risks caused by low ionizing radiation doses. Most studies estimating the population risk are based on the life span study of such survivors(16-18). However, evidence of excess risk of fatal cancer in people exposed to high energy radiation also come from other types of studies, such as those involving populations exposed to radiation of medical origin (for example: studies with radiotherapy treatments), occupational exposure and environmental exposure(15). In 2001, Brenner et al.(19) concluded that there may be up to 500 additional fatal cancer cases related to CT scans annually performed in the pediatric population in the United States of America, based on estimates of the number of scans performed and a single CT protocol, leading to practically one case of fatal cancer for each 1,000 CT scans performed in children. Later in 2005, The "Committee on the Biological Effects of Ionizing Radiations" conducted an extensive literature review and developed risk projection models for the American population(15). Various criticisms to such approaches are possible, such as assuming that the linear (or quadratic) model of radiation exposure is the most appropriate to estimate related risks; generalize the exposure from a regional CT scan as being equivalent to that from a whole body scan; not considering differences between fractioned exposure and a single exposure, besides varied interpretations of epidemiological data utilized to draw conclusions about on cancer risk(20). In spite of technical difficulties inherent to the attempts to quantify such risk, the implications for public health should be considered. Even small increments in cancer risks, when applied to a high number of individuals, may result in a public health problem(11). An Australian study with 680,211 people exposed to low-dose ionizing radiation during CT scans in their childhood and adolescence, evaluated the risk for developing cancer in people exposed at CT scans compared with the risk of unexposed individuals. Such a study utilized the comparison between groups to estimate the risk, and the authors observed that the general cancer incidence in the group of exposed people was 24% higher than in the unexposed group. An increase of 1.6% in risk for cancer for each additional CT scan was observed, and such a risk was higher in individuals of lower ages. The absolute incidence for all combined cancers was 9.38 per 100,000 people/year. The effective dose per scan was estimated to be 4.5 mSv(21). For radiation doses above 100 mSv related to acute or long-term exposures, there is little questioning on the damaging consequences in human beings. According to epidemiological studies(22), radiation doses between 50 and 100 mSv (long-term exposure) or between 10 and 50 mSv (acute exposure) are associated with increased risk for some types of cancer. The mean annual natural radiation (radioactive elements present in nature) exposure of human beings is 3 mSv(14). The majority of the radiological exams produce radiation doses ranging between 0.01 mSv and 30 mSv. In spite of the wide variation, the mean dose reported in the literature, for chest radiography (anterior e lateral), for example, is 0.1 mSv, and for chest CT is 7 mSv, i.e., one chest CT scan is equivalent to 70 chest (anterior and lateral) radiographs(23). In Brazil, the Comissão Nacional de Energia Nuclear (CNEN) (National Commission of Nuclear Energy) establishes three basic radioprotection principles: justification, optimization and limitation of individual doses. The principle of justification means that any activity involving radiation must be justifiable in relation to other alternatives and produce a net benefit to society. The optimization principle establishes that all exposures should be maintained as low as reasonably achievable (ALARA). The last principle imposes that the individual doses on workers and general public individuals should not exceed the annual dose limits established by CNEN(24). The ALARA principle is strongly supported by the Society for Pediatric Radiology in the United States, particularly for CT. The current imaging methods must be optimized in order to reduce the radiation exposure in pediatric patients(25), who may be up to ten times more radiosensitive than adults. According to this principle two approaches are necessary to limit the doses: the first approach, related to the equipment itself whose design should be optimized for dose reduction, and the second approach, related to the correct operation of such an equipment by properly trained people(26). It is also possible to discuss the attitude towards a study whose image quality is not perfect, although good enough to clarify the clinical doubt with the obtained images. In such a situation, it is not advisable to repeat the scan in order to obtain better images if such images will not provide further relevant data. In exposed pregnant women, several biological effects of ionizing radiation may be observed on the fetus, namely, intrauterine death, malformations, defects of growth and development, mutagenic and carcinogenic effects(27). The occurrence of such effects depends on the absorbed radiation dose and gestational age(28). According to the American College of Obstetricians and Gynecologists(29), the risk to the fetus in exposures with doses < 50 mGy is minimum. For doses of 100 mGy, the increase of combined risk for malformations or childhood cancer above the population incidence is of approximately 1%. Radiography (including mammography), fluoroscopy and CT in areas other than the abdomen and pelvis, expose the fetus to minimal radiation doses, and in cases where such studies include the abdominal and pelvic regions, they rarely exceed 25 mGy. The absolute risk for effects to the fetus is small for doses up to 100 mGy and minimum for doses < 50 mGy. The mentioned more severe effects have a greater possibility of occurring with doses above 100 mGy(14). CT is not forbidden for pregnant patients, particularly in some clinical situations such as polytrauma or pulmonary thromboembolism. Whenever possible, diagnostic methods which are known to be innocuous to the fetus, such as US and MRI, should be prioritized(14). CONCLUSION In order to assist physicians to request radiological studies weighting the risk in relation to the benefits, it is necessary for them to have the knowledge on ionizing radiation and its risks. If that knowledge is inappropriate, patients may be investigated more times and by methods that rely on higher than necessary radiation doses. Multidisciplinary clinical meetings and teaching activities are important forms of disseminating information on ionizing radiation, and radiology, the specialty which receives formal training on the subject, plays a fundamental role in this endeavor. REFERENCES 1. Mettler FA Jr, Bhargavan M, Faulkner K, et al. Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources – 1950-2007. Radiology. 2009;253:520–31. 2. Divrik Gökçe S, Gökçe E, Coskun M. Radiology residents' awareness about ionizing radiation doses in imaging studies and their cancer risk during radiological examinations. Korean J Radiol. 2012;13:202–9. 3. Biral AR. Radiações ionizantes para médicos, físicos e leigos. Florianópolis, SC: Insular; 2002. 4. Borgen L, Stranden E, Espeland A. Clinicians' justification of imaging: do radiation issues play a role? Insights Imaging. 2010;1:193–200. 5. Thomas KE, Parnell-Parmley JE, Haidar S, et al. Assessment of radiation dose awareness among pediatricians. Pediatr Radiol. 2006;36:823–32. 6. Soye JA, Paterson A. A survey of awareness of radiation dose among health professionals in Northern Ireland. Br J Radiol. 2008;81:725–9. 7. Arslanoglu A, Bilgin S, Kubal Z, et al. Doctors' and intern doctors' knowledge about patients' ionizing radiation exposure doses during common radiological examinations. Diagn Interv Radiol. 2007;13:53–5. 8. Jacob K, Vivian G, Steel JR. X-ray dose training: are we exposed to enough? Clin Radiol. 2004;59:928–34. 9. Lee CI, Haims AH, Monico EP, et al. Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology. 2004;231:393–8. 10. Quinn AD, Taylor CG, Sabharwal T, et al. Radiation protection awareness in non-radiologists. Br J Radiol. 1997;70:102–6. 11. Rice HE, Frush DP, Harker MJ, et al. Peer assessment of pediatric surgeons for potential risks of radiation exposure from computed tomography scans. J Pediatr Surg. 2007;42:1157–64. 12. Amis ES Jr, Butler PF, Applegate KE, et al. American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol. 2007;4:272–84. 13. Prasad KN, Cole WC, Hasse GM. Health risks of low dose ionizing radiation in humans: a review. Exp Biol Med (Maywood). 2004;229:378–82. 14. D'Ippolito G, Medeiros RB. Exames radiológicos na gestação. Radiol Bras. 2005;38:447–50. 15. Little MP, Wakeford R, Tawn EJ, et al. Risks associated with low doses and low dose rates of ionizing radiation: why linearity may be (almost) the best we can do. Radiology. 2009;251:6–12. 16. Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation. Health risks from exposure to low levels of ionizing radiation: BEIR VII Phase 2 (2006). Washington, DC: The National Academies Press; 2006. 17. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP. 2007;37:1–332. 18. United Nations Scientific Committee on the Effects of Atomic Radiation. Effects of ionizing radiation. UNSCEAR 2006 Report, Volume 1 – Report to the General Assembly, with Scientific Annexes A and B. New York, NY: United Nations; 2008. 19. Brenner DJ, Elliston CD, Hall EJ, et al. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:289–96. 20. Cohen BL. Cancer risk from low-level radiation. AJR Am J Roentgenol. 2002;179:1137–43. 21. Mathews JD, Forsythe AV, Brady Z, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013;346:f2360. 22. Brenner DJ, Doll R, Goodhead DT, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci U S A. 2003;100:13761–6. 23. Mettler FA Jr, Huda W, Yoshizumi TT, et al. Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology. 2008;248:254–63. 24. Tauhata L, Salati IPA, Di Prinzio R, et al. Radioproteção e dosimetria: fundamentos. Rio de Janeiro, RJ: IRD/CNEN; 2003. 25. Kleinerman RA. Cancer risks following diagnostic and therapeutic radiation exposure in children. Pediatr Radiol. 2006;36 Suppl 2:121–5. 26. Strauss KJ, Kaste SC. The ALARA (as low as reasonably achievable) concept in pediatric interventional and fluoroscopic imaging: striving to keep radiation doses as low as possible during fluoroscopy of pediatric patients – a white paper executive summary. Pediatr Radiol. 2006;36 Suppl 2:110–2. 27. Brent RL. The effect of embryonic and fetal exposure to x-ray, microwaves, and ultrasound: counseling the pregnant and nonpregnant patient about these risks. Semin Oncol. 1989;16:347–68. 28. McCollough CH, Schueler BA, Atwell TD, et al. Radiation exposure and pregnancy: when should we be concerned? Radiographics. 2007;27:909–17. 29. ACOG Committee on Obstetric Practice. ACOG Committee Opinion. Number 299, September 2004 (replaces No. 158, September 1995). Guidelines for diagnostic imaging during pregnancy. Obstet Gynecol. 2004;104:647–51. 1. MD, Hospital Santa Helena, Santo André, SP, Brazil 2. Teacher and Assistant Academic Director, Escola de Medicina da Universidade Anhembi Morumbi, PhD, Department of Gynecology and Obstetrics, Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil 3. Professor, Coordinator for Support to Teaching and Research, Department of Imaging Diagnosis, Escola Paulista de Medicina da Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil 4. Teacher of Morphology and Radiology and Imaging Diagnosis, School of Medicine - Universidade Anhembi Morumbi, MD, Pediatric Radiologist and Fellow Master degree, Department of Imaging Diagnosis, Escola Paulista de Medicina da Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil Mailing Address: Dr. Rodrigo Regacini Universidade Anhembi Morumbi – Coordenação de Medicina Rua Doutor Almeida Lima, 1134, Brás São Paulo, SP, Brazil, 03164-000 E-mail: regacini@gmail.com Received June 25, 2013. Accepted after revision February 6, 2014. Study developed at Escola de Medicina da Universidade Anhembi Morumbi, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554