Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 4 - July / Aug. of 2014
Vol. 47 nº 4 - July / Aug. of 2014
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Pedro José de Santana Júnior1; Ana Caroline Vieira Aurione2; Rafael Dangoni2; Roberta Rodrigues Monteiro da Gama3; Tiago Marinho Almeida Noleto3; Kim-Ir-Sen Santos Teixeira4 |
|
|
A 62-year-old male patient complaining of asthenia, anorexia, nauseas and vomiting for two months, with weight loss of 20 kg in this period. He brought the results from high digestive endoscopy performed in another service, with report of ulcerated gastric lesion. Pallor and weight deficit were observed at physical examination. The patient denied previous history of diseases and surgeries. Computed tomography (CT) (Figures 1 and 2) was performed and subsequently the patient was submitted to laparotomy with gastroenteroanastomosis and jejunostomy with biopsy.
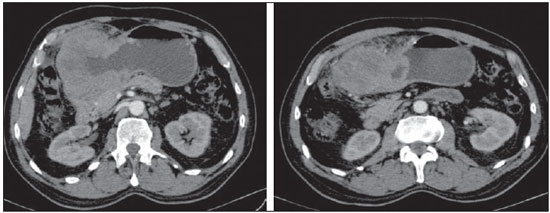 Figure 1. Contrast-enhanced whole abdomen CT, axial sections. 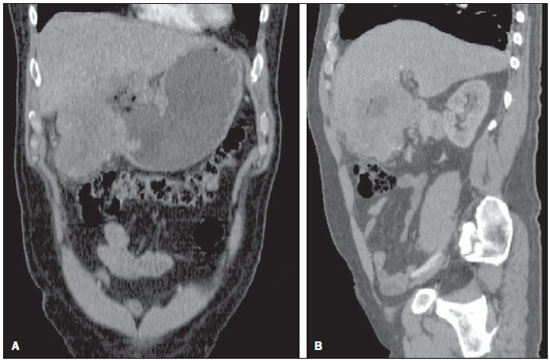 Figure 2. Contrast-enhanced whole abdomen CT, coronal (A) and sagittal reformation (B). Images description Figure 1. Contrast-enhanced whole abdomen CT, axial sections. A large lesion involving the gastric antropyloric region and the first duodenal portion, characterized by remarkable concentric irregular parietal thickening, with hypoattenuating central regions (liquefaction necrosis). Figure 2. Contrast-enhanced whole abdomen CT, coronal (A) and sagittal reformation (B). A large lesion involving the gastric antropyloric and the first duodenal portion, characterized by remarkable concentric irregular parietal thickening, with hypoattenuating central regions (liquefaction necrosis). There are signs of invasion of hepatic segments III and IV. Diagnosis: Type III gastric neuroendocrine tumor. COMMENTS The imaging evaluation of the digestive system has been approached by a series of recent publications in the Brazilian literature(1–8). Neuroendocrine tumors originate in different organs, most commonly in the gastrointestinal tract (GIT) and secondly in the bronchopulmonary tract(9,10). More rarely, such tumors affect the liver, gallbladder, ovaries, testicles and thymus, sites which also contain neuroendocrine system cells(9). Neuroendocrine gastric (carcinoid) tumor is a rare neoplasia originating from enterochromaffin cells, corresponding to 1.2–1.5% of all stomach tumors, with an incidence of 1.6-2.0 cases per 100,000 patients/year(11). Stomach is the least common site of GIT tumors, losing in frequency for small bowel, rectum, colon, cecum and appendix(12). The mean age of diagnosed patients is 60 years, with predominance in female individuals (2:1)(12). Gastric carcinoid tumors are usually classified into three types. Type I (70–85% of cases) develops with hypergastrinemia and is related to atrophic gastritis and pernicious anemia. It occurs in mid aged women, with multiple, small polypoid lesions and rarely produces metastases. Type II (5–10% of cases develops with hypergatrinemia related to Zollinger-Ellison syndrome, in most of cases in a context of type I multiple endocrine neoplasia (MEN I). Type III (15–25%), where the presently described lesion is included, presents a poor prognosis. There is no relation with hypergastrinemia and it is sporadic. Its highest incidence occurs mainly in men at the sixth decade of life, with metastases at diagnosis (frequently nodal and hepatic metastases). Such lesion is solitary, larger than 2 cm, presenting an aggressive behavior and dissemination by contiguity to the liver, many times with tendency to necrosis(11–13). The differential diagnosis for types I and II lesions includes adenomatous or hamartomatous polyps(13). Kaposi sarcoma and metastases may also manifest as small gastric parietal lesions. Adenocarcinoma, lymphoma and gastrointestinal stromal tumors are considered as differential for type III lesions(13), substantially more frequent, which highlights the relevance of the present report. The diagnosis of neuroendocrine gastric tumors involves high digestive endoscopy, endoscopic ultrasonography, computed tomography or magnetic resonance imaging, besides biopsy with immunohistochemical analysis. The surgical treatment depends on the lesion type and extent, and corresponds to local resection, antrectomy or total gastrectomy, either associated or not with lymphadenectomy. The clinical treatment involves the use of somatostatin for symptoms management, in addition to complementary chemotherapy and/or radiotherapy as necessary. REFERENCES 1. Fernandes DA, Chagas ACP, Jesus AR, et al. Aspectos ultrassonográficos associados à morbidade de formas clínicas crônicas de esquistossomose mansônica, utilizando-se protocolo proposto pela Organização Mundial da Saúde. Radiol Bras. 2013;46:1–6. 2. Monjardin RF, Costa DMC, Romano RFT, et al. Diagnóstico da esteatose hepática pela tomografia computadorizada de abdome com meio de contraste intravenoso. Radiol Bras. 2013;46:134–8. 3. Salvadori PS, Costa DMC, Romano RFT, et al. Quando a fase de equilíbrio pode ser suprimida nos exames de tomografia computadorizada de abdome? Radiol Bras. 2013;46:65–70. 4. Eifler RV. O papel da ultrassonografia na medida da gordura subcutânea e visceral e sua correlação com a esteatose hepática. Radiol Bras. 2013;46:273–8. 5. Teixeira ACV, Torres US, Westin CEG, et al. Tomografia computadorizada com multidetectores no diagnóstico pré-operatório das complicações intestinais causadas pela ingestão de corpos estranhos da dieta sem suspeita clínica: série de casos enfatizando o uso de técnicas de renderização volumétrica. Radiol Bras. 2013;46:346–50. 6. Costa DMC, Salvadori PS, Monjardim RF, et al. Quando a fase sem contraste intravenoso é desnecessária nos exames de tomografia computadorizada do abdome? Análise retrospectiva de 244 casos. Radiol Bras. 2013;46:197–202. 7. Hollanda ES, Torres US, Gual F, et al. Perfuração espontânea da vesícula biliar com formação de biloma intra-hepático: sinais ultrassonográficos e correlação com tomografia computadorizada. Radiol Bras. 2013;46:320–2. 8. Galvão BVT, Torres LR, Cardia PP, et al. Prevalência de cistos simples e hemangiomas hepáticos em pacientes cirróticos e não cirróticos submetidos a exames de ressonância magnética. Radiol Bras. 2013;46:203–8. 9. Levy AD, Sobin LH. From the archives of the AFIP: Gastrointestinal carcinoids: imaging features with clinicopathologic comparison. Radiographics. 2007;27:237–57. 10. Scarsbrook AF, Ganeshan A, Statham J, et al. Anatomic and functional imaging of metastatic carcinoid tumors. Radiographics. 2007;27:455–77. 11. Chang S, Choi D, Lee SJ, et al. Neuroendocrine neoplasms of the gastrointestinal tract: classification, pathologic basis, and imaging features. Radiographics. 2007;27:1667–79. 12. Dal Pizzol AC, Linhares E, Gonçalves R, et al. Tumores neuroendócrinos do estômago: série de casos. Rev Bras Cancerol. 2010;56:453–61. 13. Ganeshan D, Bhosale P, Yang T, et al. Imaging features of carcinoid tumors of the gastrointestinal tract. AJR Am J Roentgenol. 2013;201:773–86. 1. Titular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), Substitute Professor at School of Medicine – Universidade Federal de Goiás (UFG), Goiânia, GO. Brazil 2. MDs, Residents, Department of Radiology and Imaging Diagnosis, Hospital das Clínicas – Universidade Federal de Goiás (UFG), Goiânia, GO, Brazil 3. Trainee Physicians, Department of Radiology and Imaging Diagnosis, Hospital das Clínicas – Universidade Federal de Goiás (UFG), Goiânia, GO. Brazil 4. PhD, Associate Professor and Head of Department of Radiology and Imaging Diagnosis, Hospital das Clínicas – Universidade Federal de Goiás (UFG), Goiânia, GO. Brazil Mailing Address: Dr. Pedro José de Santana Júnior Avenida T4, nº 1616, ap. 402 B, Setor Serrinha Goiânia, GO, Brazil, 74835-090 E-mail: pedrojoseradiohcufg@gmail.com Study developed at Department of Radiology and Imaging Diagnosis of Hospital das Clínicas – Universidade Federal de Goiás (UFG), Goiânia, GO, Brazil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554