Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 3 - May / June of 2014
Vol. 47 nº 3 - May / June of 2014
|
ICONOGRAPHIC ESSAY
|
|
Intraventricular mass lesions at magnetic resonance imaging: iconographic essay - part 1 |
|
|
Autho(rs): Felipe Damásio de Castro1; Fabiano Reis2; José Guilherme Giocondo Guerra3 |
|
|
Keywords: Neoplasms; Cerebral ventricle neoplasms; Central nervous system; Magnetic resonance imaging. |
|
|
Abstract: INTRODUCTION
Intraventricular tumors represent a subgroup of intracranial lesions with typical and unique features, which may be considered apart from the classical subdivisions of tumors into intra- and extra-axial lesions(1). In spite of the fact that such lesions are easy to visualize, the differential diagnosis may be difficult without the knowledge on the types of tissues that give rise to such tumors(2). The ventricles are surrounded by a layer of ependymal cells and a subependymal plate formed by glial cells. Such layers give origin to ependymomas, subependymomas and subependymal giant cell astrocytomas. Such a lining and the septum pellucidum that is located between the corpus callosum and the fornix, separating the lateral ventricles, also give origin to central neurocytoma, a unique glial neuronal tumor of the ventricular systems(2). The choroid plexus is the most vascularized portion of the ventricular system and produces the cerebrospinal fluid. Primary neoplasias of this tissue are highly vascularized and are commonly associated with hydrocephalus due increased production of cerebrospinal fluid. Such lesions have a benign presentation (choroid plexus papillomas) and, less frequently, a malignant presentation (choroid plexus carcinomas). Tumors such as meningiomas and metastases may also occur in this location. Masses are more frequently found in the posterior portion of the lateral ventricles(2), but their location may vary according to the type of tumor. Choroid plexus papillomas occur mainly in children, with predilection for the lateral ventricles in this age range, while in adults it usually is more frequently found in the fourth ventricle. Ependymomas are most frequent in the posterior fossa in children, and in adults they are generally supratentorial. Many times, inflammatory/infectious lesions are observed within the ventricular system, and among them neurocysticercosis is very common in Brazil. Other less frequent conditions, such as histoplasmosis, may also be observed. In the present essay, the authors have gathered images obtained along the last 15 years at the Radiology Service of Hospital de Clínicas - Universidade Estadual de Campinas. The study was approved by the Committee for Ethics in Research of the Institution. RADIOLOGICAL FINDINGS Ependymoma Between 50% and 75% of ependymomas occur in the posterior fossa(1). Among those occurring in the intraventricular region, 58% originate in the fourth ventricle, while the other 42% are located in the lateral and third ventricles(2). Such tumors develop as a relatively soft mass, filling the ventricular lumen and molding into the ventricular cavity(1). At non-contrast-enhanced computed tomography (CT), intraventricular ependymomas are usually isodense, with areas of calcifications (40-80% of cases). Occasionally, intratumoral hemorrhages may produce a blood-fluid level. At contrast-enhanced CT, there is heterogeneous contrast enhancement(2-4). At magnetic resonance imaging (MRI) (Figure 1), ependymoma may appear as either a solid tumor or as a mixed solid cystic tumor. The solid portion of the lesion presents hypo or isosignal at T1-weighted sequences, and hypersignal at T2-weighted sequences, while the cystic portion presents a signal similar to the signal of the cerebrospinal fluid at T1- and T2-weighted sequences. The main feature of such tumors is signal heterogeneity. Areas of spontaneous hypersignal corresponding to hemorrhage may be observed at T1-weighted sequences. At susceptibility-weighted imaging, foci of hyposignal are commonly observed, corresponding to calcifications or hematic products. After paramagnetic contrast agent injection, a generally heterogeneous enhancement of this tumor is observed(1,3). MRI is considered the modality of choice to evaluate such lesions(2). 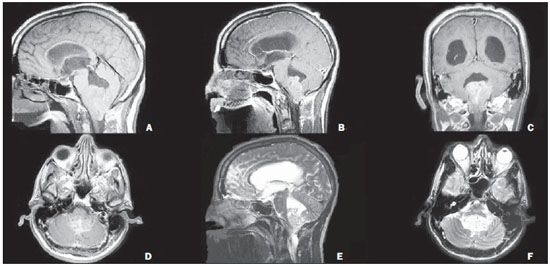 Figure 1. Male, 53-year-old patient. Sagittal MRI T1-weighted sequence (A) shows a plastic lesion located in the fourth ventricle, extending down to the Luschka's, Magendie's and magnum foramens, with areas of hypersignal (hemorrhage) and contrast uptake (B,C,D). At T2-weighted sequence (E,F), the lesion is hyperintense, with foci of hyposignal (hemorrhage/small calcifications). Anatomopathological analysis revealed the presence of an ependymoma. Low-grade astrocytoma The most common location of such tumors is in the temporal and frontal lobes. Intraventricular low-grade astrocytomas are located in the frontal horn, third ventricle, atrium and fourth ventricle. They may form focal masses with regular margins(1). At CT, astrocytomas are visualized as a hypodense, solidcystic mass(5). Such lesions are hypovascular tumors and usually present less intense enhancement than other intraventricular masses(6). At MRI (Figure 2), astrocytomas are homogeneous, presenting iso- or hyposignal at T1-weighted sequences and hypersignal at T2-weighted sequences. Cysts may be observed within the lesion. Contrast-enhancement is variable(1). 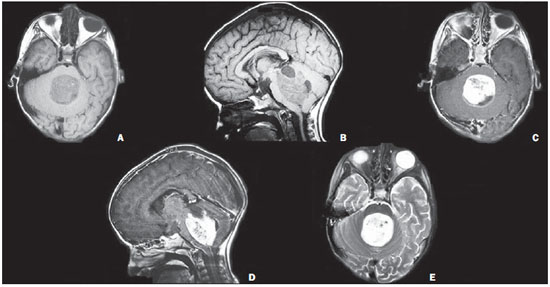 Figure 2. Male, 3-year-old patient. Axial (A) and sagittal (B) MRI T1-weighted sequences show the presence of a heterogeneous, solid-cystic lesion located in the fourth ventricle, with isosignal and some foci of hypersignal at T1-weighted sequence (hemorrhage). Axial (C) and sagittal (D) sections at contrast-enhanced T1-weighted sequences show intense contrast uptake in the solid component of the lesion. At T2-weighted sequence (E), the solid component shows predominant hypersignal, with some foci of hyposignal (hemorrhage). Biopsy revealed pilocytic astrocytoma. Central neurocytoma This tumor is frequently located in the ventricular system, filling the lateral ventricle from the foramen of Monro. At CT, the tumor presents in the form of either a polylobulated or round-shaped lesion that may be spontaneously hyperdense, isodense or mixed(3,7). They are seen attached to the septum pellucidum, and may extend to both lateral ventricles(1,8). Subtle or moderate enhancement is observed after contrast agent injection. Calcifications and cysts may be present(8). At MRI (Figure 3), the typical finding is that of an intraventricular mass, frequently located in the foramen of Monro, in contact with the septum pellucidum. The tumor is frequently isointense in relation to the parenchyma at T1-weighted sequence, and subtly hypointense at T2-weighted sequence. Cystic zones may be observed(8). The lesion appearance is spongy(3). After contrast agent injection, subtle or moderate enhancement of the lesion is observed(7). 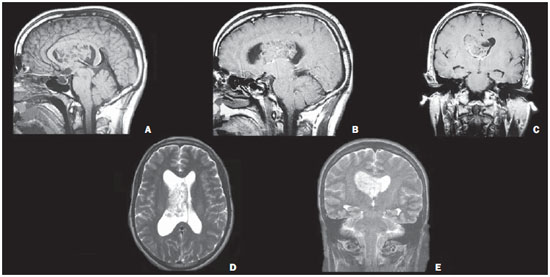 Figure 3. Male, 33-year-old patient. Sagittal MRI T1-weighted sequence (A) presents a heterogeneous, solid lesion with isosignal/areas of hyposignal (cystic areas) located in the right lateral ventricle, adjacent to the septum pellucidum, extending toward the foramen of Monro and left lateral ventricle, determining hydrocephalus. At contrast-enhanced T1-weighted sequence (B,C) a subtle enhancement is observed. On the axial and coronal sections of T2-weighted sequences (D,E), the lesion presents isosignal/hypersignal. Biopsy revealed the presence of a central neurocytoma. Ganglioglioma Gangliomas are benign tumors affecting principally children and young adults, most frequently located in the temporal lobes. Exclusively intraventricular location is rarely observed. MRI findings are nonspecific. Most commonly, the mass presents iso- or hyposignal on T1-weighted images, and iso- or hypersignal on T2-weighted images. Peripheral gross ("bizarre") calcifications may be observed. The pattern of enhancement of the mass by the paramagnetic contrast agent ranges from none to intense(1) (Figure 4). 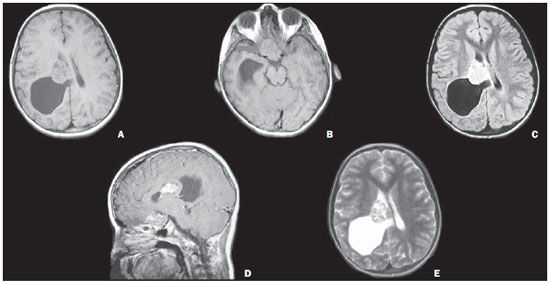 Figure 4. Female, 10-year-old patient. Axial MRI T1-weighted sequences (A) demonstrate the presence of a solid-cystic lesion located in the right lateral ventricle, with solid component presenting isosignal and cystic component with hyposignal. Also, an isointense lesion is observed in the optic chiasm (arrow on B) at axial T1-weighted image. After contrast injection (D), intense, but heterogeneous uptake is observed. Axial FLAIR sequence (C) shows a lesion with hyperintense signal, and at T2-weighted sequence (E) the lesion presents with heterogeneous, mixed signal, with internal hydrated foci. There is a lesion with similar characteristics in the optic chiasm (B,D – arrows). Anatomopathological analysis was conclusive for ganglioglioma in both lesions. Choroid plexus papilloma Amongst intracranial tumors, choroid plexus mass lesions are rare, representing about 0.4–0.6% of cases in patients of all ages. Such tumors occur predominantly in the first decade of life (38%), especially in the first two years. Papillomas are the most common choroid plexus mass lesions in children, principally before the fifth year of life and predominantly located in the lateral ventricles. The second most frequent location is the fourth ventricle, most commonly in adult individuals, and rarely in the third ventricle(1,9). At CT, papillomas are isodense or slightly hyperdense to the gray matter. Calcifications are found in 25% of cases. The contours are lobulated, with slightly irregular margins(3). The contrast enhancement is intense and slightly heterogeneous. At MRI, a large lobulated mass isointense to the white matter is observed at T1-weighted sequences. Calcifications and intralesional flow voids may be observed. Intense enhancement is observed after intravenous contrast injection(1,9) (Figure 5). 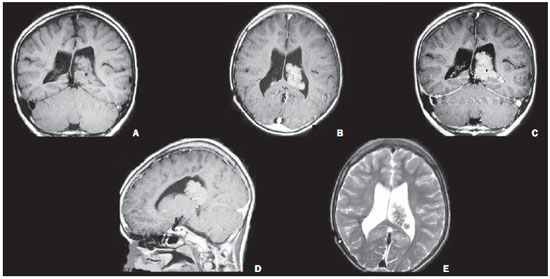 Figure 5. Male, 10-year-old patient. Coronal MRI T1-weighted sequence (A) demonstrates a solid, microlobulated, cauliflower-like lesion located in the left lateral ventricle, with isosignal at T1-weighet sequence, with foci of hyposignal (calcifications or vessels). At contrast-enhanced T1-weighted sequence (B,C,D) intense contrast uptake is observed. Axial T2-weighted sequence (E) shows isosignal with foci of hyposignal. Hydrocephalus is present. Anatomopathological analysis revealed choroid plexus papilloma. 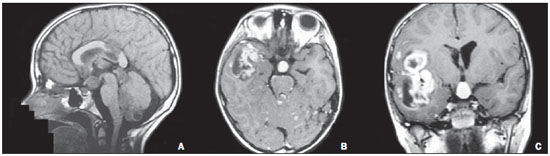 Figure 6. Male, 10-year-old patient. Sagittal MRI (A) T1-weighted sequence shows heterogeneous lesion with hyposignal located in the fourth ventricle, suprasellar cistern, pineal gland, septum pellucidum, lateral ventricle and hypophyseal stalk. At contrast-enhanced T1-weighted sequence (B,C) there is contrast uptake by the lesion and also an intraparenchymal mass or liquoric lesions in the right fronto-temporo-insular region (intraventricular metastasis from primary central nervous system lesion). Histopathological analysis revealed PNET dissemination. Primitive neuroectodermal tumors Primitive neuroectodermal tumor (PNET) is a generic name for the classification that includes medulloblastomas and histologically indistinguishable neoplasms located in the central nervous system, at other sites than the cerebellum. Medulloblastoma is a type of PNET that most frequently affects the central nervous system, particularly in the first decade of life. It is located in the posterior fossa, typically filling the fourth ventricle, with about 67%-93% being located in the cerebellar vermis(1). At CT, medulloblastomas are seen as a spontaneously hyperdense lesion, and evidence of vasogenic edema may be found(5). In children, MRI demonstrates a usually intraventricular mass located on the median or paramedian line, with relatively homogeneous signal intensity. Usually, isosignal is observed on T1-weighted sequences, and iso- or hyposignal on T2-weighted sequences, besides typical diffusion restriction and intense enhancement following contrast agent injection. In adult individuals, the spectrum of signal intensity is similar to that of children, frequently presenting isosignal on T2-weighted sequences(1). Meningioma It is the most common benign neoplasm of the central nervous system(1), representing 33% of all (asymptomatic) intracranial incidentalomas. In adult individuals, intraventricular meningiomas are amongst the most common tumors found in the lateral ventricles. CT reveals a sharply delineated, lobulated mass with periventricular edema(4,5). Focal or diffuse ventricular dilatation may be present, depending on the degree of obstruction to the drainage of cerebrospinal fluid (CSF). Calcifications are commonly found (in 50% of cases)(2). At MRI (Figure 7), the lesion may be seen as an iso- to hypointense mass on T1-weighted sequences and, in general isointense on T2-weighted sequences(2), with intense contrast-enhancement(5). 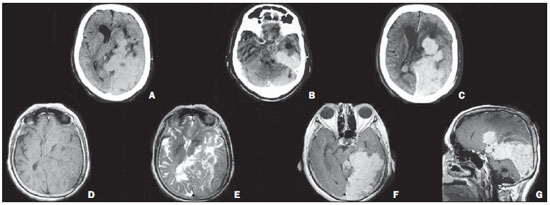 Figure 7. Female, 67-year-old patient. Pre-contrast axial CT (A) and post-contrast axial CT (B,C) demonstrate spontaneously hyperdense, lobulated lesion with intense contrast uptake. Axial MRI T1-weighted sequence (D) shows expansile lesion with isosignal located in the posterior and inferior horns of the left lateral ventricle infiltrating the adjacent parenchyma, characterized by extensive nodularity with intense contrast enhancement (F,G). At T2-weighted sequence (E) the lesion presents hyposignal. The patient underwent surgery for resection of intraventricular meningioma in the left lateral ventricle (images not available), which revealed the presence of an atypical meningioma with frequent figures of mitosis positive for the Ki-67 marker in 20% of the nuclei, which indicates a high degree of cell proliferation. The images refer to the lesion recurrence. Epidermoid tumor Intracranial epidermoid tumors are congenital inclusion cysts corresponding to 0.2-1.8% of primary intracranial neoplasias(10) (it is the most common congenital tumor of the nervous central system(1)). Its most common site is the cerebellopontine angle cistern(10) and the incidence peak is at the fourth decade of life(1). Such tumors develop within the ventricular spaces, surrounding adjacent vessels and nerves(10). The lesion margins are generally irregular and associated obstructive hydrocephalus may be observed. Calcifications are present on the lesion borders in 25% of cases(1). At CT, the typical appearance is that of an extra-axial hypodense mass without venous contrast uptake. At MRI such tumors may presents with iso- or subtle hypersignal to the CSF on T1- and T2-weighted sequences (Figure 8). The main differential diagnosis is made with arachnoid cyst, generally by means of FLAIR and diffusion-weighted sequences. The arachnoid cyst follows the CSF signal intensity at all sequences, while epidermoid tumors are not hypointense at FLAIR sequences, showing areas of hypersignal to CSF. Contrarily to arachnoid cysts, epidermoid tumors typically present diffusion restriction(10). 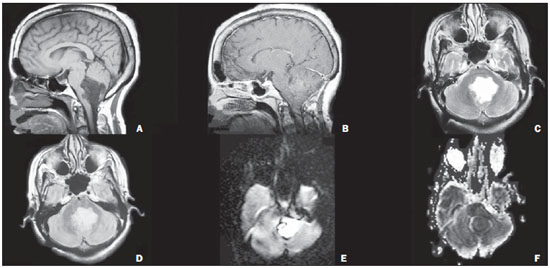 Figure 8. Female, 60-year-old patient. Sagittal MRI T1-weighted sequence (A) demonstrates cystic lesion with lobulated margins, irregular contours and low signal intensity. At contrast-enhanced T1-weighted sequence (B), the lesion presented enhancement, and at T2-weighted sequence (C) was hyperintense. Heterogeneous signal is observed at FLAIR sequence (D), with hypersignal at diffusion-weighted image and hyposignal at ADC mapping (diffusion restriction) (E,F). The lesion is located in the fourth ventricle. Anatomopathological analysis revealed epidermoid tumor. CONCLUSION Imaging findings of intraventricular tumors are quite variable, probably because of the diversity of tissues in the central nervous system which give origin to such lesions. Thus, the study of the skull, particularly by MRI, playa a relevant role in the attempt to define the differential diagnoses based on their location and characteristics of signal at the different sequences, as well as in the detection of hemorrhagic elements and calcifications. It is the responsibility of the radiologist to know the main imaging findings of each lesion in the attempt to narrow the differential diagnosis. REFERENCES 1. Leite CC, Sequeiros IM, Lacerda MTC, et al. Tumores intraventriculares: achados à ressonância magnética. Rev Imagem. 2001;23:73-85. 2. Koeller KK, Sandberg GD; Armed Forces Institute of Pathology. From the archives of the AFIP. Cerebral intraventricular neoplasms: radiologic-pathologic correlation. Radiographics. 2002;22:1473-505. 3. Smith AB, Smirniotopoulos JG, Horkanyne-Szakaly I. From the radiologic pathology archives: intraventricular neoplasms: radiologicpathologic correlation. Radiographics. 2013;33:21-43. 4. Fenchel M, Beschorner R, Naegele T, et al. Primarily solid intraventricular brain tumors. Eur J Radiol. 2012;81:e688-96. 5. Shogan P, Banks KP, Brown S. AJR teaching file: Intraventricular mass. AJR Am J Roentgenol. 2007;189(6 Suppl):S55-7. 6. Tien RD. Intraventricular mass lesions of the brain: CT and MR findings. AJR Am J Roentgenol. 1991;157:1283-90. 7. Conrad MD, Morel C, Guyotat J, et al. Neurocitomas do sistema nervoso central - análise clínico-patológica de três casos. Arq Neuropsiquiatr. 2000;58:1100-6. 8. Chen H, Zhou R, Liu J, et al. Central neurocitoma. J Clin Neurosci. 2012;19:849-53. 9. Glastonbury CM, Osborn AG, Salzman KL. Masses and malformations of the third ventricle: normal anatomic relationships and differential diagnoses. Radiographics. 2011;31:1889-905. 10. Forghani R, Farb RI, Kiehl TR, et al. Best cases from the AFIP. Fourth ventricle epidermoid tumor: radiologic, intraoperative, and pathologic findings. Radiographics. 2007;27:1489-94. 1. MD, Resident of Radiology and Imaging Diagnosis at Hospital de Clínicas - Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil 2. PhD, Docent responsible for the Division of Neuroradiology, Professor, Department of Radiology, Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil 3. Graduate Student of Medicine, Faculdade de Ciências Médicas - Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil Mailing Address: Dr. Fabiano Reis Faculdade de Ciências Médicas - Universidade Estadual de Campinas, Departamento de Radiologia Rua Tessália Vieira de Camargo, 126, Cidade Universitária Zeferino Vaz Caixa Postal: 6111 Campinas, SP, Brazil, 13083-887 E-mail: fabianoreis2@gmail.com Received February 17, 2013. Accepted after revision September 11, 2013. Study developed at Hospital de Clínicas - Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554