Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 3 - May / June of 2014
Vol. 47 nº 3 - May / June of 2014
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Maria Clara Fernandes; Gláucia Zanetti; Bruno Hochhegger; Edson Marchiori |
|
|
A 26-year-old male patient, drugs user, presenting with dry cough and fever for two weeks. The patient has a diagnosis of acquired immunodeficiency syndrome (AIDS), with poor adherence to the treatment. His CD4 count was 20 cells/mm3 and the viral load was 495,208 cps/ml. Chest radiography demonstrated opacity in the right upper lobe of the lung. Chest computed tomography was performed (Figure 1).
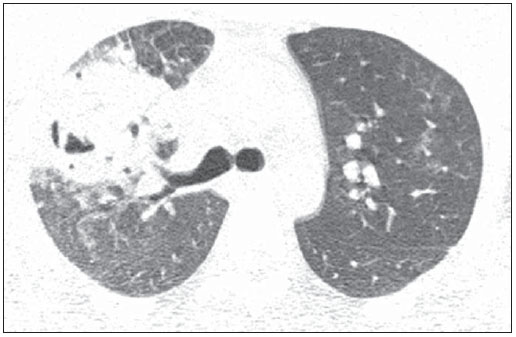 Figure 1. Computed tomography with window for pulmonary parenchyma. Section at the level of the carina. Image description Figure 1. Chest computed tomography shows cavitated consolidation in the right upper lobe of the lung. Also, one observes small nodules and ground glass opacities adjacent to the described image as well as in the contralateral lung. Diagnosis: Rhodococcus equi pneumonia in an AIDS patient. Open biopsy was performed and culture demonstrated bacterial growth. COMMENTS R. equi is a Gram-positive cocci that commonly causes infection in horses and other animals. R. equi infection is rarely found in humans(1), affecting particularly individuals at advanced degree of immunodeficiency. About 80% of cases occur in AIDS patients, most of times in those presenting CD4 lymphocyte count lower than 200 cell/mm3(2,3). In humans, the main infection site is the lung(1). The most frequent clinical presentation is a slow-growing pneumonic process, with cough, fever and constitutional symptoms. R. equi represents a frequent cause of bacteremia and extra-pulmonary signs may be found. The etiological agent can be easily isolated from the sites of infection(2). The main pattern of lung involvement is that of masses with heterogeneous contrast impregnation or foci of pulmonary consolidation intermingled with air bronchograms, either with or without cavitated lesions. Although cavitation may be not present at the moment of the diagnosis, it ends up developing along the disease progression(4). Other findings include ground glass opacities, air-space nodules, small nodules with predominantly centrilobular distribution and the tree-in-bud pattern predominantly located around consolidations. Probably, such findings represent bronchogenic dissemination of the infection. Mediastinal lymph nodes enlargement may be present(1,2,4-8). The typical histopathological finding of R. equi infection corresponds to necrotizing cavitation or soft tissue mass composed of a dense histiocytic infiltrate with abundant eosinophilic granular cytoplasm. Polymorphonuclear leukocytes are numerous in disseminated microabscesses. Periodic acid Schiff staining demonstrates highly positive histiocytes similar to those observed in Whipple's disease. Gram-positive cocci are easy demonstrated at Gram tissue stain. Pulmonary malakoplakia is another finding described in R. equi infection(9). The differential diagnoses for pulmonary R. equi infection in AIDS patients include cavitated infections (tuberculosis, nocardiosis, fungal diseases, lung abscess), lung neoplasms, and more remotely Pneumocystis jiroveci pneumonia (7,10,11). Micobacterium tuberculosis infection, however, is the main differential diagnosis to be considered for patients with R. equi pneumonia, since both bacilli are alcohol-acid resistant. The diagnosis of disease activity in patients with pulmonary tuberculosis depends on multiple factors, namely, clinical signs, physical examination, tuberculin test results and, mainly, detection of the bacillus in sputum, bronchoalveolar lavage, transtracheal aspirate or in lung biopsy specimen, being reinforced by other factors such as sequential alterations at serial chest radiography and previous history of antituberculosis therapy. However, the diagnosis may be difficult considering the facts that sputum bacilloscopy may be negative in 21-66% of cases and it may take up to six weeks for a bacillus colony to grow in a culture, and that findings at chest radiography are frequently classified as indeterminate(12-14). High-resolution computed tomography (HRCT) has shown to be superior to plain radiography in the detection and evaluation of extent of parenchymal alterations, considering that because of its effectiveness in the evaluation of the secondary lung lobe, it allows for a better characterization of pathological pulmonary processes. A recent series of studies published by Brazilian authors(15-23) corroborates such assertion. Thus, HRCT plays an extremely relevant role in the diagnosis of pulmonary tuberculosis. HRCT findings in patients with post-primary tuberculosis include centrilobular nodules, air space nodules, nodular opacities, tree-in-bud pattern, miliary nodules, consolidations, cavitations, bronchial walls thickening, tuberculomas, calcifications, parenchymal bands, interlobular septal thickening, ground glass opacities, pericicatricial emphysema and fibrotic alterations(12,13,24-32). Other manifestations recently described include reversed halo sign and clusters of micronodules, either with or without confluence(33-35). Most of such findings can also be observed in patients with R. equi pneumonia. In conclusion, R. equi infection should be considered in the differential diagnosis of cavitated consolidations in AIDS patients, with a particular difficult differentiation from lesions caused by tuberculosis. REFERENCES 1. Alves J, Cerqueira EMFP, Nanni L, et al. Rhodococcus equi: infecção pulmonar em pacientes imunocomprometidos - relato de um caso e revisão da literatura. Radiol Bras. 1997;30:347-9. 2. Capdevila JA, Buján S, Gavaldà J, et al. Rhodococcus equi pneumonia in patients infected with human immunodeficiency virus. Report of 2 cases and review of the literature. Scand J Infect Dis. 1997;29:535-41. 3. Haramati LB, Jenny-Avital ER. Approach to diagnosis of the pulmonary disease in patients infected with human immunodeficiency virus. J Thorac Imaging. 1998;13:247-60. 4. Arlotti M, Zoboli G, Moscatelli GL, et al. Rhodococcus equi infection in HIV-positive subjects: a retrospective analysis of 24 cases. Scand J Infect Dis. 1996;28:463-7. 5. Wicky S, Cartei F, Mayor B, et al. Radiological findings in nine AIDS patients with Rhodococcus equi pneumonia. Eur Radiol. 1996;6:826-30. 6. Marchiori E, Müller NL, Mendonça RG, et al. Rhodococcus equi pneumonia in AIDS: high-resolution CT findings in five patients. Br J Radiol. 2005;78:783-6. 7. Marchiori E, Müller NL, Souza Jr AS, et al. Pulmonary disease in patients with AIDS: high-resolution CT and pathologic findings. AJR Am J Roentgenol. 2005;184:757-64. 8. Marchiori E, Mendonça RG, Capone D, et al. Rhodococcus equi infection in acquired immunodeficiency syndrome. Computed tomography aspects. J Bras Pneumol. 2006;32:405-9. 9. Scott MA, Graham BS, Verrall R, et al. Rhodococcus equi - an increasingly recognized opportunistic pathogen. Report of 12 cases and review of 65 cases in the literature. Am J Clin Pathol. 1995;103:649-55. 10. Marchiori E, Gasparetto EL, Escuissato DL, et al. Pulmonary paracoccidioidomycosis and AIDS: high-resolution CT findings in five patients. J Comput Assist Tomogr. 2007;31:605-7. 11. Silva Filho FP, Marchiori E, Valiante PM, et al. AIDS-related Kaposi sarcoma of the lung presenting with a "crazy-paving" pattern on highresolution CT: imaging and pathological findings. J Thorac Imaging. 2008;23:135-7. 12. Hatipoğlu ON, Osma E, Manisali M, et al. High resolution computed tomographic findings in pulmonary tuberculosis. Thorax. 1996;51:397-402. 13. Im JG, Itoh H, Shim YS, et al. Pulmonary tuberculosis: CT findings - early active disease and sequential change with antituberculous therapy. Radiology. 1993;186:653-60. 14. McGuinness G, Naidich DP, Jagirdar J, et al. High resolution CT findings in miliary lung disease. J Comput Assist Tomogr. 1992;16:384-90. 15. Amorim VB, Rodrigues RS, Barreto MM, et al. Computed tomography findings in patients with H1N1 influenza A infection. Radiol Bras. 2013;46:299-306. 16. Zanetti G, Nobre LF, Mançano AD, et al. Nodular reversed halo sign caused by pulmonary tuberculosis confirmed by sputum culture. Radiol Bras. 2013;46(6):ix-x. 17. Costa AN, Giassi KS, Bachion GH, et al. Post-traumatic pulmonary pseudocyst in a soccer player: a case report. Radiol Bras. 2013;46:122-4. 18. Amoedo MK, Souza LVS, Souza AS, et al. Pulmonary interstitial emphysema: a case report and review of the literature. Radiol Bras. 2013;46:317-9. 19. Souza VF, Chaves RT, Balieiro VS, et al. Qualitative and quantitative pulmonary density analysis in a patient with polymyositis and pulmonary fibrosis. Radiol Bras. 2013;46(3):ix-x. 20. Pereira e Silva JL. The virus-drug-host dynamics in the tomographic characterization of pulmonary influenza A (H1N1) infection - a clinical-radiological-pathological view. Radiol Bras. 2013;46(5):vii-ix. 21. Koenigkam-Santos M, Barreto ARF, Chagas Neto FA, et al. Neuroendocrine tumors of the lung: major radiologic findings in a series of 22 histopathologically confirmed cases. Radiol Bras. 2012;45:191-7. 22. Bozi LCF, Melo ASA, Marchiori E. Pulmonary metastatic calcification: a case report. Radiol Bras. 2012;45:297-9. 23. Canellas R, Kanaan D, Martins PHR, et al. Spontaneous regression of pulmonary alveolar proteinosis: a case report. Radiol Bras. 2012;45:294-6. 24. Campos CA, Marchiori E, Rodrigues R. Pulmonary tuberculosis: findings on high resolution computerized tomography of active disease on patients with bacteriological confirmation. J Pneumol. 2002;28:23-9. 25. Carneiro da Silva VM, Luiz RR, Barreto MM, et al. Competence of senior medical students in diagnosing tuberculosis based on chest X-rays. J Bras Pneumol. 2010;36:190-6. 26. Marchiori E, Zanetti G, Irion KL, et al. Reversed halo sign in active pulmonary tuberculosis: criteria for differentiation from cryptogenic organizing pneumonia. AJR Am J Roentgenol. 2011;197:1324-7. 27. Lee JY, Lee KS, Jung KJ, et al. Pulmonary tuberculosis: CT and pathologic correlation. J Comput Assist Tomogr. 2000;24:691-8. 28. Marchiori E, Francisco FA, Zanetti G, et al. Lymphobronchial fistula: another complication associated with lymphobronchial tuberculosis in children. Pediatr Radiol. 2013;43:252-3. 29. Jeong YJ, Lee KS. Pulmonary tuberculosis: up-to-date imaging and management. AJR Am J Roentgenol. 2008;191:834-44. 30. Hochhegger B, Zanetti G, Marchiori E. Mass invading the trachea: a rare presentation of tuberculosis simulating lung cancer. Infection. 2013:41:599-600. 31. Nakanishi M, Demura Y, Ameshima S, et al. Utility of high-resolution computed tomography for predicting risk of sputum smear-negative pulmonary tuberculosis. Eur J Radiol. 2010;73:545-50. 32. Ceratti S, Pereira TR, Velludo SF, et al. Pulmonary tuberculosis in a patient with rheumatoid arthritis undergoig immunosuppressive treatment: case report. Radiol Bras. 2014;47:60-2. 33. Marchiori E, Grando RD, Simões Dos Santos CE, et al. Pulmonary tuberculosis associated with the reversed halo sign on high-resolution CT. Br J Radiol. 2010;83:e58-60. 34. Marchiori E, Zanetti G, Mano CM. Pulmonary tuberculosis with the sarcoid cluster sign in high-resolution chest CT. Radiologia. 2010;52:273-4. 35. Heo JN, Choi YW, Jeon SC, et al. Pulmonary tuberculosis: another disease showing clusters of small nodules. AJR Am J Roentgenol. 2005;184:639-42. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil Mailing Address: Dr. Edson Marchiori Rua Thomaz Cameron, 438, Valparaíso Petrópolis, RJ, Brazil, 25685-120 E-mail: edmarchiori@gmail.com Study developed at Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554