Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 6 - Nov. / Dec. of 2013
Vol. 46 nº 6 - Nov. / Dec. of 2013
|
CASE REPORT
|
|
Prenatal diagnosis of Beckwith-Wiedemann syndrome by two- and three-dimensional ultrasonography |
|
|
Autho(rs): Edward Araujo Júnior1; Christiane Simioni2; Luciano Marcondes Machado Nardozza1; Antonio Fernandes Moron3 |
|
|
Keywords: Prenatal diagnosis; Beckwith-Wiedemann syndrome; Two-dimensional ultrasonography; Three-dimensional ultrasonography. |
|
|
Abstract: INTRODUCTION
Beckwith-Wiedemann syndrome (BWS) is a congenital overgrowth disorder characterized by macroglossia, gigantism, omphalocele, visceromegaly and increased risk for embryonic neoplasia. Its incidence is one case in every 13,500 live births(1). Most cases are sporadic, but the mode of inheritance is complex and includes a dominant autosomal pattern with variable expressivity and gene deregulation in the chromosomal region 11p15.5(2). Generally, the diagnosis of this condition is made in the postnatal period by means of findings of macroglossia, omphalocele, gigantism, visceromegaly, advanced bone age, renal dysplasia, facial nevi and ear creases(1). The prenatal diagnosis of such condition is of paramount importance to the perinatal follow-up as well as for determining the way of delivery, pediatric care due to neonatal hypoglycemia, superior airways obstruction, congestive heart failure, risk for malignancy and genetic tests for family members. The prenatal diagnosis of BWS by means of two-dimensional ultrasonography (2DUS) may be based on two major criteria or on one major and one minor criterion. Major criteria include macroglossia, macrosomia (estimated weight > 90th percentile for the gestational age), and defective abdominal wall. Minor criteria include polyhydramnios, nephromegaly, renal dysplasia and adrenal cytomegaly confirmed by pathological diagnosis. Three-dimensional ultrasonography (3DUS) in rendering mode allows a better assessment of the fetal surface, contributing to a more comprehensive understanding of the malformation by the parents. Only one report of prenatal diagnosis of BWS by 3DUS is found in the literature(3). The authors present a case of BWS diagnosed by 2DUS at the 28th gestational week, and emphasize the main findings of such disorder at 3DUS in rendering mode. CASE REPORT A 32-year-old, white, primigesta was referred to the Department of Obstetrics at Universidade Federal de São Paulo (Unifesp), São Paulo, Brazil, with a diagnosis of renal dysplasia and polyhydramnios. The patient presented gestational age of 28 weeks and five days, based on the date of her last menstruation, and denied previous history of familial genetic diseases. 2DUS demonstrated biometry compatible with 29 weeks, polyhydramnios (amniotic fluid index 255 mm), estimated fetal weight 2,661 g (90th percentile = 1,416 g), increased placental thickness, multicystic left kidney. Abdominal cystic mass measuring 5.4 × 5.7 × 5.9 cm and macroglossia (Figure 1). Based on such findings, the authors raised the hypothesis of BWS. Echocardiography revealed a normal heart, while karyotyping by amniocentesis demonstrated normal male karyotype (46,XY). In order to supplement the 2D diagnosis. 3DUS was performed with a Voluson 730 Expert equipment (General Electric Health-care; Zipf, Austria) coupled to a multifrequency convex transducer (RAB 4-8L). 3DUS in the rendering mode clearly demonstrated the remarkable fetal abdominal distension and macroglossia (Figure 2). The patient remained under prenatal follow-up in the authors' institution and presented preterm labor at 30 weeks and one day, which was inhibited with intravenous terbutaline. During her hospital stay, fetal hemodynamic centralization was identified at Doppler US. A single corticoid cycle (betamethasone, 12 mg/day for two days) was performed and the patient underwent Cesarean section three days afterwards and gave birth to a male child weighting 2,450 g (above the 97th percentile for the gestational age). Immediately after birth, the neonate presented severe hypoglycemia, and progressed to respiratory insufficiency and death after three hours of life. Anatomopathological study confirmed the diagnosis of BWS. 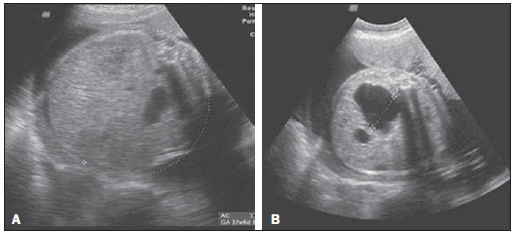 Figure 1. 2DUS findings in a fetus with BWS at the 28th gestational week. A: Abdominal circumference compatible with a gestational age of 37 weeks and six days (> the 98th percentile). B: Cystic dysplasia in the right kidney.  Figure 2. 3DUS rendering mode findings in a fetus with BWS at the 28th gestational week. A: Remarkable fetal abdominal distension. B: Macroglossia. DISCUSSION BWS was first described by Beckwith in 1963 and by Wiedemann in 1964(4). According to Eliott et al.(5) who followed-up 74 pediatric patients with BWS, the most frequent findings were the following: macroglossia (97%), gigantism (88%), abdominal wall defect (80%), ear creases (76%), hypoglycemia (63%), facial nevi (62%), multicystic dysplasia or nephromegaly (59%) and hemihypertrophy (24%). Hemihypertrophy is the only sign significantly associated with the development of embryonic tumors, particularly Wilms' tumor. In the present case, the authors observed the presence of macrosomia and macroglossia, which represent the two major signs for the diagnosis of BWS, besides polyhydramnios and renal dysplasia (minor signs). O'Connor et al.(6) have described a case of BWS diagnosed by 2DUS at the 22nd week, in association with omphalocele and placentomegaly with cystic areas. In the present case, the authors have also observed placentomegaly, but without cystic areas. Prenatal and neonatal ultrasonography has been utilized for many years in the assessment of fetal malformations(7-9). 3DUS in rendering mode has clearly demonstrated the remarkable fetal abdominal distension and macroglossia. For many years, 3DUS in rendering mode has been utilized in the assessment of fetal malformations, allowing a better understanding of the parents in relation to the fetal anomalies and aiding in the definition of the approach to be adopted during the prenatal period(10,11). In spite of not being essential for the diagnosis of BWS, 3DUS was extremely important for a better understanding on the disease by the parents and by the involved multidisciplinary team. In the literature, there is only one report about prenatal diagnosis of BWS by means of 3DUS, in a study developed by Eckmann-Scholz et al.(3). Such authors have described a case that was also diagnosed at the 28th. gestational week, where, like in the present case, 3DUS has clearly demonstrated the presence of macroglossia. In summary, the authors believe that 3DUS in association with 2DUS can contribute to a better prenatal assessment of some fetal malformations such as BWS, allowing a better understanding of this disease by the parents as well as by the multidisciplinary clinical team. REFERENCES 1. Harker CP, Winter T 3rd, Mack L. Prenatal diagnosis of Beckwith-Wiedemann syndrome. AJR Am J Roentgenol. 1997;168:520-2. 2. Tilghman SM. The sins of the fathers and mothers: genomic imprinting in mammalian development. Cell. 1999;96:185-93. 3. Eckmann-Scholz C, Jonat W. 3-D ultrasound imaging of a prenatally diagnosed Beckwith-Wiedemann syndrome. Arch Gynecol Obstet. 2011;284:1051-2. 4. Wiedemann HR. Complexe malformatif familial avec hernie ombilicale et macroglossie: un "syndrome nouveau"? J Genet Hum. 1964;13:223-32. 5. Elliott M, Bayly R, Cole T, et al. Clinical features and natural history of Beckwith-Wiedemann syndrome: presentation of 74 new cases. Clin Genet. 1994;46:168-74. 6. O'Connor C, Levine D. Case 49: Beckwith-Wiedemann syndrome. Radiology. 2002;224:375-8. 7. Baldisserotto M, Fiori H, Fiori R, et al. Neonato com ascite urinária e ruptura de cálice renal secundárias a válvula de uretra posterior: diagnóstico ultrassonográfico. Radiol Bras. 2011;44:68-70. 8. Barros LM, Fernandes DA, Melo EV, et al. Malformações do sistema nervoso central e malformações associadas diagnosticadas pela ultrassonografia obstétrica. Radiol Bras. 2012;45:309-14. 9. Rios LT, Araújo Júnior E, Nardozza LM, et al. Rânula congênita: diagnóstico ultrassonográfico antenatal. Radiol Bras. 2012;45:300-1. 10. Araujo Júnior E, Kawanami TE, Nardozza LM, et al. Prenatal diagnosis of bilateral anophthalmia by 3D "reverse face" view ultrasound and magnetic resonance imaging. Taiwan J Obstet Gynecol. 2012;51:616-9. 11. Barros FS, Araujo Júnior E, Rolo LC, et al. Prenatal diagnosis of lethal multiple pterygium syndrome using two- and three-dimensional ultrasonography. J Clin Imaging Sci. 2012;2:65. 1. Private Docents, Associate Professors of Fetal Medicine, Department of Obstetrics, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil 2. Master, Volunteer Physician, Division of Fetal Medicine, Department of Obstetrics at Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil 3. Private Docent, Full Professor, Department of Obstetrics, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil Mailing Address: Dr. Edward Araújo Júnior Rua Carlos Weber, 956, ap. 113, Visage, Vila Leopoldina São Paulo, SP, Brazil, 05303-000 E-mail: araujojred@terra.com.br Received March 15, 2013. Accepted after revision April 26, 2013. Study developed in the Department of Obstetrics at Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554