Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 4 - July / Aug. of 2013
Vol. 46 nº 4 - July / Aug. of 2013
|
ORIGINAL ARTICLE
|
|
When the non-contrast-enhanced phase is unnecessary in abdominal computed tomography scans? A retrospective analysis of 244 cases |
|
|
Autho(rs): Danilo Manuel Cerqueira Costa1; Priscila Silveira Salvadori1; Rodrigo da Fonseca Monjardim1; Elisa Almeida Sathler Bretas2; Lucas Rios Torres2; Rogerio Pedreschi Caldana3; David Carlos Shigueoka4; Regina Bitelli Medeiros5; Giuseppe D'Ippolito6 |
|
|
Keywords: Computed tomography; Ionizing radiation; Abdomen; Contrast media. |
|
|
Abstract: INTRODUCTION
Currently, radiological studies represent one of the main sources of exposure to ionizing radiation of artificial origin(1). In such a context, computed tomography (CT) is highlighted as one of the most important radiological techniques for medical applications, whose utilization has significantly increased in the past decades(2). As a consequence of the dissemination of such technique in the medical practice, a significant increase has been observed in the radiation dose to which patients who require diagnostic exams are exposed(1). Currently, CT is responsible for slightly over 15% of all diagnostic imaging diagnostic studies and for more than 75% of the total radiation coming from imaging procedures to which the population is exposed(3). The risks associated with ionizing radiations are proportional to the exposure(4). Therefore, every diagnostic scan should be performed under accurate clinical indication and relying on as low as reasonably achievable radiation doses, without compromising diagnostic quality(5,6). Innumerable studies have been developed with a view on reducing the radiation dose in CT, by adopting several different strategies(7,8). Among such strategies, the suppression of some of the studies' phases seems to be a practical and safe way to achieve dose reduction, since the reliability and diagnostic accuracy of the exams are maintained(9). Currently, there is a wide range of specific abdominal CT protocols for the most diverse clinical suspicions(10). Most of such protocols utilize the non-contrast-enhanced phase which precedes the contrast-enhanced phases. In spite of being widely and universally adopted for determined clinical indications, the use of such protocols have implications related to radiation dose, images acquisition time and x-ray tube wear, and would only be justifiable in case it added supplementary data indispensable for the establishment of an accurate diagnosis, thus positively interfering in the approach to patients and prognosis(9). Abdominal CT scan protocols may include up to four or more phases. Each one of these phases has specific objectives and isolatedly or in conjunction allows the establishment of a diagnosis, increasing the sensitivity and accuracy of the method. On the other hand, the specific weight of each one of those CT images acquisition phases and notably the value of the non-contrast-enhanced phase in such a context are not clear for the main clinical indications. The evaluation of the usefulness of this phase in the study of abdominal organs would open the opportunity to suppress it in certain clinical situations, thus reducing the radiation dose absorbed by the patient and the inherent potential risks of the method. Thus, the present study is aimed at evaluating the need for the non-contrast-enhanced phase in different abdominal CT protocols as well as its impact on the diagnosis. MATERIALS AND METHODS The present study was approved by the Committee for Ethics in Research of Escola Paulista de Medicina – Universidade Federal de São Paulo (EPM-Unifesp), and the need for terms of free and informed consent was waived considering the retrospective nature of the study. In the period between August and November 2011 an observational, a cross-sectional and retrospective study was undertaken evaluating 244 consecutive abdominal CT scans. Of those CT studies, 107 (43.8%) were from male patients and 137 (56.2%) were from women. The mean patients' age was 66.2 years, ranging between 18 and 88 years. Of the total of 244 scans, 35.5% were performed in emergency service patients, 34.2% in inpatients, and 34.2% in outpatients. Inclusion criteria were patients above 18 years of age, with spontaneous request for abdominal CT scan with indication for utilization of intravenous contrast agent. Exclusion criteria were patients younger than 18 years, with indication for non-contrast-enhanced abdominal CT scans, or with contraindication for utilization of iodinated contrast agents. Patients whose indication for the scan was investigation of hematuria were also excluded, considering the well established theoretical groundings in literature advocating the need for non-contrast-enhanced phase in such cases(11,12). All the scans were performed in a multidetector Brilliance 64® CT equipment (Philips Medical Systems; Best, The Netherlands), following the protocols included in the Routine Procedures Manual of the CT Unit of the Department of Imaging Diagnosis of the authors' institution (available at http://ddi.unifesp.br/medicos-e-profissionais-da-saude/193/exames/). The intravenous contrast injection was made by means of an automated injection pump, at a velocity of 3–4 ml/s and at a ratio of 1.5–2 ml/kg of weight, depending upon the iodine concentration, and with a maximum volume of 150 ml. The triggering time for the different contrast-enhancement phases (arterial, portal and equilibrium) was established based upon the automatic tracking of contrast medium peak flow in the aorta. The following technical parameters were utilized: a) collimation of 64 × 0.625 mm; b) 120 kVp; c) mAs established as a function of automatic modulation of radiation dose; d) pitch of 0.891; e) reconstruction thickness of 3.0 mm. After the contrast agent injection, the images were acquired in the arterial, portal and equilibrium contrast-enhancement phases (respectively, between 15–30 seconds, 60–80 seconds and 3–5 minutes after the start of contrast medium administration), according to the clinical indication and following the scan protocols of the service. Rectal or oral administration of the contrast agent was made as described by the institutional CT scan protocol. The radiation dose was controlled by means of automatic dose modulation available in the CT apparatus, and expressed as dose length product (DLP) in mGy. The DLP represents the radiation dose of one CT slice multiplied by the extent of the scan and is measured in mGy/cm. The effective radiation dose (estimating the total risk for stochastic effects induction on an irradiated organ due to radiation exposure) can be calculated by multiplying the DLP by a correction factor as a function of the studied anatomical region. Such correction factor is utilized for the calculation of the effective dose (expressed in mSv), and, in abdominal CT scans, it ranges between 0.015 and 0.018(13). In the present study the calculation was made with a correction factor corresponding to 0.015. The result obtained from such calculation is not the exact value of estimated radiation, but it can be utilized as a reference value at a given CT service, considering the great practical difficulty in measuring an exact dose per patient because of the wide range of variables involved in the calculation, inherent to the patient (for example: body mass index, abdominal circumference, irradiated organ) and to the utilized technical factors (for example: kV, mAs, pitch)(14). All images were interpreted on a Synapse® PACS/3D (FujiFilm; USA) workstation, by one radiologist from a five-member team, all of them with at least three-year experience in abdominal radiology, who issued reports initially based only on the images acquired in contrast-enhanced phases, without evaluating the non-contrast-enhanced phase (first phase), and subsequently combining the findings of all the phases, including the non-contrast-enhanced phase (second analysis). The observers had previous access to the data on the medical requests for each CT scan, and, at the first and second analysis, classified the tomographic diagnoses into primary and secondary diagnoses, according to their clinical priority and importance for the patient. The primary diagnoses were those directly related to the clinical indication for the scans or which justified the clinical condition of the patient. The secondary diagnoses were established by consensus between observers and based on data in the literature(15). At the end of each evaluation, each one of the five observers established whether there were changes in their primary and secondary diagnoses between the first and second analyses, i.e., whether the interpretation based on the analysis of the images acquired in the non-contrast-enhanced phase modified the diagnosis, as compared with the first analysis. Statistical analysis The frequency of changes in the primary and secondary diagnoses was measured, according to the clinical indication, as the first and second analyses were compared. An extension of the Fisher's exact test was utilized to evaluate the changes in the primary diagnoses, considering results with p < 0.05 as significant. As regards secondary diagnoses, the proportion of cases of change of diagnosis considering the total number of CT scans was evaluated. RESULTS The present study included 244 patients evaluated according to the following clinical indications: neoplasm, including staging, re-staging and primary tumor investigation in 122 patients (50%); acute abdomen in 45 patients (18%); investigation of intracavitary collection in 38 patients (15%); investigation of hepatocellular carcinoma (HCC) in 19 patients (7%), among others. Among the 45 patients with clinical indication for acute abdomen, 71% were of the inflammatory subtype; 14%, of the perforative type; 5%, of the obstructive type; 5%, of the hemorrhagic type; and 5% were vascular type. The protocols directed towards investigation of adrenal nodule, trauma and foreign body, classified as "other", in spite of also being evaluated in relation to the primary diagnosis, were not submitted to statistical analysis, considering the insufficient number of patients. Furthermore, in such a group, no change was observed in the primary diagnoses. The mean radiation dose per phase was 835 mGy/cm (DLP), corresponding to an estimated effective radiation dose of 12.5 mSv per phase. Among the 122 patients whose clinical indication was neoplasm, only one (0.8%) of them had the diagnosis modified after evaluation of the non-contrast-enhanced phase (second analysis), without statistical significance (p > 0.999). The scans with protocols directed towards investigation of acute abdomen, intracavitary collection and hepatocellular carcinoma did not present changes in the primary diagnoses. Of the 244 patients, 35 (14%) had their secondary diagnoses modified for the different clinical indications, namely: a) nephrolithiasis (25 patients, 10%); b) steatosis (7 patients, 3%); c) cholelythiasis (1 patient, 0.3%); d) adrenal nodule (2 patients, 0.7%). DISCUSSION Over the past years, an increasing utilization of CT scans has been observed. Such dissemination of the utilization of CT contributes for the increase in the exposure of patients to significant doses of ionizing radiations, whose potential harmful and deleterious effects to health cannot be ignored or underestimated. The risk/benefit ratio from such an exposure must be carefully evaluated with a view on the principles of radiological protection to patients and on the optimization of the protocols and clinical practices(2,3,5). Many studies have been undertaken with the objective of reducing the radiation dose in abdominal CT scans, by adopting several strategies(9,16–18). Some authors have reported that the diagnostic accuracy of imaging methods for certain diseases is not impaired as one or more scan phases are suppressed. In 2004, Imbriacco et al.(18), evaluating patients with suspected pancreatic neoplasia, demonstrated that the utilization of a single contrast-enhanced phase in multislice CT is an effective technique for diagnosis and staging of such type of tumor. Iannaccone et al.(8), in 2005, reported that the combined use of the arterial, portal and equilibrium phases present sensitivity and positive predictive value of 92.8% and 97.3%, respectively, for detection of HCC in cirrhotic patients, concluding that the non-contrast-enhanced phase does not add value to justify its utilization for the investigation of such tumors. In 2008, Leite et al.(9) evaluated 100 patients with undefined clinical indication or in tumor staging/re-staging, demonstrating that the non-contrast-enhanced phase is not indispensable for such evaluations. In 2010, other authors such as Kim et al.(17), in a prospective study whose gold-standard was liver biopsy, that the non-contrast-enhanced phase could be suppressed in the evaluation of hepatic steatosis, being replaced by the portal phase, with high sensitivity and specificity. With a view on this contemporary and poorly consolidated theme, particularly in the Brazilian literature, the authors of the present study tried to contribute by focusing on a different approach, i.e., instead of focusing on a determined disorder or clinical situation, they approached a wide range indications for CT scans in the routine of a CT service, with the purpose of evaluating the impact of the non-contrast-enhanced phase on the main CT scan protocols. As regards the primary diagnosis, the second analysis added value in only one of the 224 cases of the four main groups of clinical indications (investigation of primary tumor, suspicion of acute abdomen, investigation of intracavitary collection and HCC detection); in the remaining 20/244 cases, no change was observed in the primary diagnoses after the second analyses. The patient who benefited from the second analysis underwent CT scan for colon cancer staging. The initial diagnosis (after the first analysis) indicated the presence of an indeterminate renal nodule. The final diagnosis (after the second analysis) demonstrated the presence of a cyst with dense contents, on account of its intermediate density at the non-contrast-enhanced phase (52 HU) and absence of enhancement at the contrast-enhanced phases(19) (Figure 1). According to the observer, the remaining imaging findings were normal, with no sign of metastatic dissemination of the colon cancer to other organs. In spite of the fact that such change in the diagnosis was considered as relevant, some considerations are necessary. 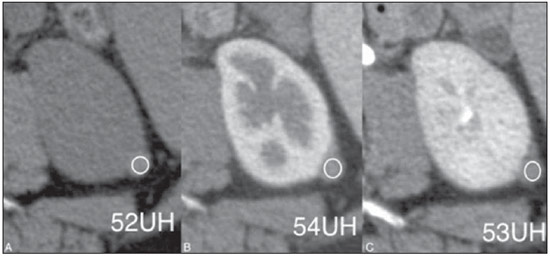 Figure 1. Change in the primary diagnosis. Cyst with dense contents, characterized at the noncontrast-enhanced phase (A), without significant enhancement in the portal (B) and equilibrium (C) phases. Renal metastases from colon tumors are rare events, Cases of metastasis from colon cancer generally are observed in other organs(20,21), a fact which was not observed in that particular case, and making the diagnosis of metastasis by implantation in the kidney unlikely in such a context. Additionally, another strategy could be utilized to differentiate a solid renal lesion from a hyperdense cyst. Chung et al.(22) have evaluated 43 histopathologically confirmed renal cysts and demonstrated that the absence of significant enhancement throughout the various contrast-enhanced phases is indicative of cystic lesion, even in cases where the pre-contrast phase is not available. In the analysis of the present case, the renal nodule classified as indeterminate at the first analysis, presented similar density at the post-contrast phases, contributing to the hypothesis of actually being a cyst. As regards secondary diagnoses, the authors observed some changes that could be better characterized in the second analysis (with the addition of the non-contrast-enhanced phase). In two non-oncologic patients (scans for investigation of trauma and acute abdomen), adrenal nodules < 1.5 cm were identified, and were indeterminate at the contrast-enhanced phase, and compatible with adenomas according to the density measurement obtained at the non-contrast-enhanced phase. In such cases, where the contrast-enhanced phase does not allow for an accurate diagnosis, it is recommended that the patient be recalled for a new evaluation with a non-contrast-enhanced phase and, if necessary, with a protocol directed towards the study of adrenal nodule, thus without any direct clinical impact(23). However, it is important to also consider that, in spite of incidental adrenal nodules being considered of high clinical relevance when indeterminate(15), it has been demonstrated that, in non-oncologic patients, the occurrence of malignancy is extremely rare in such group of lesions(24). As regards hepatic steatosis, which was not identified by the first analysis in seven of the 244 cases (3%), recent studies have demonstrated that, by utilizing formulas or evaluation methods, the portal phase, as isolatedly utilized, presents an accuracy similar to the non-contrast-enhanced phase in the diagnosis of steatosis(17,25,26). In the present study, by applying the formula proposed by Kim et al.(17), all the seven patients diagnosed with steatosis in the analysis of the non-contrast-enhanced phase (liver density lower than that of the spleen), would have also been diagnosed by means of isolated analysis of the portal phase (Figure 2). However, the formula developed by Kim et al. is complex and depends upon multiple measurements, which makes the method non-practical in spite of its high effectiveness. In a recent study undertaken by the authors of the present study, such a method was tried out in a simplified manner, with good results and specificity above 90%, reducing the number of measurements and entering the formula into a Microsoft Office Excel® worksheet, thus facilitating its use in the daily practice(27). In spite of that, and considering that this method is still poorly utilized, the authors of the present study suggest that the non-contrast-enhanced phase continues to be utilized in the investigation of steatosis. However, one should remember that magnetic resonance imaging and more recently liver elastography (Fibroscan), have been the methods recommended for such a purpose(28,29), so the indication of CT as the tool of choice for the diagnosis of hepatic steatosis becomes questionable. 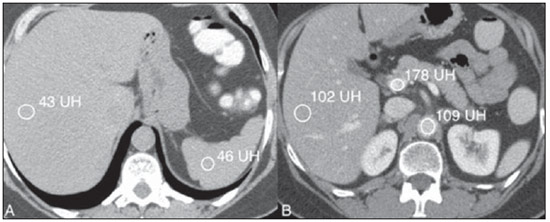 Figure 2. Changes in secondary diagnosis. A: Hepatic steatosis diagnosed in the non-contrast-enhanced phase by the lower attenuation of the liver (43 HU) in relation to the spleen (46 HU). B: Same case of hepatic steatosis retrospectively diagnosed in the portal phase with regions of interest in the liver, portal vein and aorta, utilizing the formula proposed by Kim et al. and with the simplified calculation method proposed by the authors(27). Renal calculi were identified in 25 patients by means of the non-contrast-enhanced phase. All of them were less than 5 mm in diameter, non-obstructive, and were found in asymptomatic patients (Figure 3), and such signs suggest the adoption of an expectant approach(30,31). Additionally, as such cases are re-analyzed by manipulating and changing the windowing width and level in the available phases of the study, the authors observed that it is possible to enhance the detection of renal calculi in the arterial and portal phases. 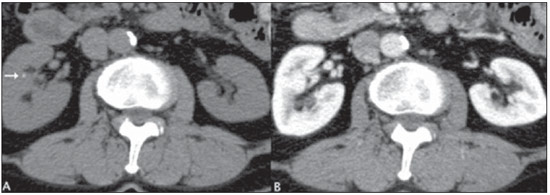 Figure 3. Change in secondary diagnosis. Renal lithiasis (arrow) diagnosed only in the second analysis, with the non-contrast-enhanced phase. A: Non-contrast-enhanced phase. B: Portal phase. Another change in secondary diagnosis occurred in a case of asymptomatic cholelythiasis. It is a known fact that even utilizing the non-contrast-enhanced phase, the evaluation of cholelythiasis is limited at CT, with sensitivity ranging between 25% and 88%, Ultrasonography is the method of choice in the study of such a disorder(32,33). It is important to observe that in spite of advocating the suppression of the non-contrast-enhanced phase in cases of acute abdomen, the CT scan protocols for pain in the right iliac fossa (in the suspicion of appendicitis) and in the left iliac fossa (in the suspicion of diverticulitis), the non-contrast-enhanced phase is performed in the authors' institution, and intravenous contrast medium is utilized only in cases of diagnostic doubt(10). In the present study, a significant number of oncologic patients investigated for acute abdomen and intra-abdominal infectious process would benefit from the suppression of the non-contrast-enhanced phase, reducing the radiation dose, with no impact on their diagnosis or approach. Such a reduction in radiation dose would range between 25% and 33% of the total dose, as one considers scans performed with four and three acquisition phases, respectively. With the utilization of any protocol (three or four phases), one observes a mean dose reduction per scan equivalent to the effective dose of 12.5 mSv, because of the suppression of the acquisition phase without intravenous contrast agent injection. The management of the radiation dose by means of a judicious utilization of the different acquisition phases in protocols of abdominal CT has been the object of several recently published studies(34,35). The number of patients evaluated in HCC investigation (19 patients) could have been higher, but it was enough to verify, by means of statistical tests, that there was no impact in suppressing the non-contrast-enhanced phase, as other studies have already suggested8). The authors believe that further studies with larger samples will be able to validate and confirm the initial results of the present study. One limitation in the present study was the wide range of analyzed protocols and several clinical indications, which led to a reduced number of patients in some groups (for example, investigation for adrenal nodules, trauma and foreign body), a fact which impaired the statistical analysis in such cases. However, the present study describes the habitual hospital routine of abdominal CT scans in the proposed period, justifying the low prevalence of such mentioned indications. Another limitation was related to the fact that the diagnostic accuracy of the two analyses were not measured, a fact which did not allow the assessment of the method's effectiveness as the non-contrast-enhanced phase is suppressed. However, in order to measure the accuracy of a diagnostic method it is necessary to utilize a test or reference standard, which is not practical in a great number of clinical situations in the daily practice and, therefore, could not be utilized in the present study. Finally, another criticism could be related to the fact that only experienced observers were utilized. Further studies, comparing the results obtained by the analyses performed by observers with different training levels may clarify such issue. CONCLUSION Based on the analysis of the present study results, it is possible to conclude that the non-contrast-enhanced phase can be suppressed in abdominal CT scans protocols aimed at investigating acute abdomen, intracavitary collections, cancer staging and re-staging as well as investigation of HCC, without any expressive loss in the diagnostic capability of the method. REFERENCES 1. Jessen KA, Panzer W, Shrimpton PC, et al. EUR 16262: European Guidelines on Quality Criteria for Computed Tomography. Luxembourg: Office for Official Publications of the European Communities; 2000. 2. Brenner DJ, Hall EJ. Computed tomography – an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–84. 3. Kalra MK, Maher MM, Toth TL, et al. Strategies for CT radiation dose optimization. Radiology. 2004;230:619–28. 4. Wolbarst AB, Wiley AL Jr, Nemhauser JB, et al. Medical response to a major radiologic emergency: a primer for medical and public health practitioners. Radiology. 2010;254:660–77. 5. No authors listed. 1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP. 1991;21:1–201. 6. McCollough CH, Guimarães L, Fletcher JG. In defense of body CT. AJR Am J Roentgenol. 2009;193:28–39. 7. Meagher T, Sukumar VP, Collingwood J, et al. Low dose computed tomography in suspected acute renal colic. Clin Radiol. 2001;56:873–6. 8. Iannaccone R, Laghi A, Catalano C, et al. Hepatocellular carcinoma: role of unenhanced and delayed phase multi-detector row helical CT in patients with cirrhosis. Radiology. 2005;234:460–7. 9. Leite APK, Mattos LA, Pinto GADH, et al. O valor da fase sem contraste na tomografia computadorizada do abdome. Radiol Bras. 2008;41:289–96. 10. D'Ippolito G, Nunes Jr JAT, Wolosker AMB, et al. O valor da tomografia computadorizada sem contraste na avaliação da região cecoapendicular normal. Radiol Bras. 1996;29:247–51. 11. Kawashima A, Vrtiska TJ, LeRoy AJ, et al. CT urography. Radiographics. 2004;24 Suppl 1:S35–54. 12. Joffe SA, Servaes S, Okon S, et al. Multi-detector row CT urography in the evaluation of hematuria. Radiographics. 2003;23:1441–56. 13. Huda W, Ogden KM, Khorasani MR. Converting dose-length product to effective dose at CT. Radiology. 2008;248:995–1003. 14. Birnbaum S. Radiation protection in the era of helical CT: practical patient based programs for decreasing patient exposure. Semin Ultrasound CT MR. 2010;31:46–52. 15. Yee J, Sadda S, Aslam R, et al. Extracolonic findings at CT colonography. Gastrointest Endosc Clin N Am. 2010;20:305–22. 16. Dalmazo J, Elias J, J, Brocchi MAC, et al. Otimização da dose em exames de rotina em tomografia computadorizada: estudo de viabilidade em um hospital universitário. Radiol Bras. 2010;43:241–8. 17. Kim DY, Park SH, Lee SS, et al. Contrast-enhanced computed tomography for the diagnosis of fatty liver: prospective study with same-day biopsy used as the reference standard. Eur Radiol. 2010;20:359–66. 18. Imbriaco M, Megibow AJ, Ragozzino A, et al. Value of the single-phase technique in MDCT assessment of pancreatic tumors. AJR Am J Roentgenol. 2005;184:1111–7. 19. Bosniak MA. The use of the Bosniak classification system for renal cysts and cystic tumors. J Urol. 1997;157:1852–3. 20. Aksu G, Fayda M, Sakar B, et al. Colon cancer with isolated metastasis to the kidney at the time of initial diagnosis. Int J Gastrointest Cancer. 2003;34:73–7. 21. Kim AY, Ha HK, Seo BK, et al. CT of patients with right-sided colon cancer and distal ileal thickening. AJR Am J Roentgenol. 2000;175:1439–44. 22. Chung EP, Herts BR, Linnell G, et al. Analysis of changes in attenuation of proven renal cysts on different scanning phases of triphasic MDCT. AJR Am J Roentgenol. 2004;182:405–10. 23. Korobkin M, Brodeur FJ, Francis IR, et al. CT time-attenuation washout curves of adrenal adenomas and nonadenomas. AJR Am J Roentgenol. 1998;170:747–52. 24. Song JH, Chaudhry FS, Mayo-Smith WW. The incidental adrenal mass on CT: prevalence of adrenal disease in 1,049 consecutive adrenal masses in patients with no known malignancy. AJR Am J Roentgenol. 2008;190:1163–8. 25. Brunt EM. Pathology of fatty liver disease. Mod Pathol. 2007;20 Suppl 1:S40–8. 26. Lawrence DA, Oliva IB, Israel GM. Detection of hepatic steatosis on contrast-enhanced CT images: diagnostic accuracy of identification of areas of presumed focal fatty sparing. AJR Am J Roentgenol. 2012;199:44–7. 27. Monjardim RF, Costa DMC, Romano RFT, et al. Diagnóstico da esteatose hepática pela tomografia computadorizada de abdome com meio de contraste intravenoso. Radiol Bras. 2013;46:134–8. 28. Qayyum A, Chen DM, Breiman RS, et al. Evaluation of diffuse liver steatosis by ultrasound, computed tomography, and magnetic resonance imaging: which modality is best? Clin Imaging. 2009;33:110–5. 29. Ma X, Holalkere NS, Kambadakone RA, et al. Imaging-based quantification of hepatic fat: methods and clinical applications. Radiographics. 2009;29:1253–77. 30. Türk C, Knoll A, Petrik A, et al. Guidelines on urolithiasis. Update March 2011. Arnhem, The Netherlands: European Association of Urology (EAU); 2011. 31. Burgher A, Beman M, Holtzman JL, et al. Progression of nephrolithiasis: long-term outcomes with observation of asymptomatic calculi. J Endourol. 2004;18:534–9. 32. Chan WC, Joe BN, Coakley FV, et al. Gallstone detection at CT in vitro: effect of peak voltage setting. Radiology. 2006;241:546–53. 33. Bortoff GA, Chen MY, Ott DJ, et al. Gallbladder stones: imaging and intervention. Radiographics. 2000;20:751–66. 34. D'Ippolito G, Braga FA, Resende MC, et al. Enterografia por tomografia computadorizada: uma avaliação de diferentes contrastes neutros. Radiol Bras. 2012;45:139–43. 35. Parente DB. Contrastes orais neutros para enterografia por tomografia computadorizada. Radiol Bras. 2012;45(3):v–vi. 1. MDs, Residents, Department of Diagnostic Imaging, Escola Paulista de Medicina – Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil 2. MDs, Radiologists, Department of Diagnostic Imaging, Escola Paulista de Medicina – Universidade Federal de São Paulo (EPM-Unifesp), and Hospital São Luiz, São Paulo, SP, Brazil 3. PhD, Physician Assistant, Department of Diagnostic Imaging, Escola Paulista de Medicina – Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil 4. Assistant Professor, Department of Diagnostic Imaging, Escola Paulista de Medicina – Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil 5. Associate Professors, Department of Diagnostic Imaging, Escola Paulista de Medicina – Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil Mailing Address: Dr. Giuseppe D'Ippolito Departamento de Diagnóstico por Imagem – EPM-Unifesp Rua Napoleão de Barros, 800, Vila Clementino São Paulo, SP, Brazil, 04024-002 E-mail: giuseppe_dr@uol.com.br Received October 13, 2012. Accepted after revision May 10, 2013. * Study developed at Department of Diagnostic Imaging, Escola Paulista de Medicina – Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554