Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 2 - Mar. / Apr. of 2013
Vol. 46 nº 2 - Mar. / Apr. of 2013
|
ORIGINAL ARTICLE
|
|
What is the real role of the equilibrium phase in abdominal computed tomography? |
|
|
Autho(rs): Priscila Silveira Salvadori1; Danilo Manuel Cerqueira Costa2; Ricardo Francisco Tavares Romano2; Breno Vitor Tomaz Galvão2; Rodrigo da Fonseca Monjardim2; Elisa Almeida Sathler Bretas3; Lucas Torres Rios3; David Carlos Shigueoka4; Rogerio Pedreschi Caldana5; Giuseppe D'Ippolito6 |
|
|
Keywords: X-ray computed tomography; Ionizing radiation; Neoplasm staging; Acute abdomen. |
|
|
Abstract: INTRODUCTION
The number of computed tomography (CT) scans performed every year has been growing since the introduction of this method into clinical practice, particularly because of the increase in the number of indications for its utilization(1). Such growth has been determining a significant increase in the average individual radiation dose in the United States(2). It has recently been demonstrated that the average annual radiation dose received per individual, secondary to medical care, and particularly because of the use of CT, has overcome the dose received by the general population as a result of environmental factors(3). As a consequence of such facts, there is an increasing preoccupation in the medical community, among patients and even among equipment manufacturers, with respect to the control of radiation doses originated from the utilization of the different radiological imaging methods(3,4). In this context, several ways to reduce the radiation dose in CT scans are currently being studied, and among them the reduction in the number of image acquisition phases(5). Theses strategies utilized in combination determine a significant decrease in the radiation dose to which the patient is exposed, thus limiting the potential occurrence of deleterious effects related to ionizing radiation(6). Several studies have been undertaken to evaluate the dose reduction by decreasing the number of image acquisition phases in abdominal and pelvic CT(7-11), attempting to not affect the diagnostic accuracy of the method. Among the phases that might be suppressed is the equilibrium phase(8-10), which is acquired approximately three to five minutes after the contrast agent injection and corresponds the approximate time span required for the plasma-contrast concentration to become similar or equal to the interstitial concentration(12). Some studies establish specific indications for the performance of the equilibrium phase(13,14), however this phase has often been indiscriminately performed as a routine in most contrast-enhanced abdominal scans(15,16). The use of such study protocols has implications related not only to the radiation dose, but also to the acquisition time and X-ray tube life span(17), and would only be justifiable if it actually produced supplementary data to establish an accurate diagnosis. Based on the above considerations, the present investigation has been developed to evaluate the necessity of performing the equilibrium phase image acquisition upon several indications, and at which indications such phase might be suppressed in abdominal and pelvic CT protocols. MATERIALS AND METHODS The present study was approved by the Committee for Ethics in Research of the institution, without need for application of a term of free and informed consent. A retrospective, cross-sectional and observational study was undertaken, evaluating 219 consecutive abdominal and pelvic CT images acquired in the period between August and October of 2011, in a university hospital. Inclusion criteria were the following: patients aged above 18 years, with medical indication for abdominal and pelvic contrast-enhanced CT. Exclusion criteria were the following: a) contraindication for the iodinated contrast agent; b) scans performed with inappropriate contrast injection or presence of artifacts impairing the images interpretation; c) scans whose study protocol had not routinely included the contrast-enhanced phases (ex.: urolithiasis study); d) CT angiography of abdominal vessels. Additionally, those patients whose indications for CT were investigation of hepatocellular carcinoma, evaluation of adrenal nodule and CT urography, were excluded, as the authors understand that for such indications the equilibrium phase is still well established and justified(18-21). Of the 219 evaluated patients, 101 (46.1%) were men and 118 (53.9%) were women. The mean age was 55.5 years, ranging between 18 and 88 years. Out of all the images, 37.0% were from patients referred by the emergency room, 24.7% were from inpatients, and 38.3% were from outpatients. All scans were performed in a CT Brilliance 64® equipment (Philips Medical Systems; Best, The Netherlands), following study protocols described in the manual of routine procedures of the Unit of Computed Tomography - Department of Diagnostic Imaging. The scans were performed from the diaphragm to the pubic symphysis, before and after intravenous injection of water-soluble iodinated contrast medium. The injection was made by an automated injection pump at the rate of 3-4 ml/s, at a volume of 1-2 ml/kg of weight, limited to 150 ml, and detection of the arterial and/or portal phase by means of sustained, automated bolus tracking (ScanTools Pro®). The technical parameters included collimation of 64 x 0.625 mm, voltage of 120 kVp, 0.891 pitch, and reconstruction thickness of 3.0 mm. The radiation dose was controlled by automatic modulation of the absorbed dose, available in the CT equipment, with transcription of the report generated by the apparatus itself to the database at the end of each scan. The values are expressed in DLP (dose length product), representing the radiation dose of a CT section multiplied by the CT scan length(22). The effective radiation dose (estimating the total risk for induction of stochastic effects secondary to the exposure to radiation on an irradiated organ) can be estimated by multiplying the DLP by a correction factor as a function of the studied anatomic region. The correction factor utilized for the calculation of the effective dose (expressed in mSv) in abdominal CT studies range from 0.015 to 0.018 according to several authors(22,23). In the present study, the correction factor of 0.016 was utilized to estimate the effective radiation dose. Considering the clinical indication and the adopted study protocol, the images were acquired before the intravenous contrast medium injection, corresponding to the non-contrast-enhanced phase, and after the contrast injection, in the contrast-enhanced arterial phase (15-30 seconds after initiating the contrast agent injection), the portal phase (60-80 seconds after initiating the contrast agent injection), and the equilibrium phase (three to five minutes after initiating the contrast agent injection). Oral or rectal contrast medium was utilized as indicated by the institutional protocol. For example, in cases of appendicitis and diverticulitis, the scan is initiated with rectal contrast administration and only with one non-contrast-enhanced phase (in such circumstances, the scans were not included in the study); only in cases where this scan phase is inconclusive, the portal and equilibrium phases are performed (in such cases, the scans were included in the study). The images interpretation and data collection were organized and recorded on Microsoft® Office Excel 2003 worksheets. All the images were interpreted in the digital mode on a Synapse® PACS/3D workstation (FujiFilm; USA) by a radiologist out of a five-member team with 3- to 21-year experience in abdominal imaging, whose reports were initially based only on the non-contrast-enhanced phase and on the initial phases following contrast medium injection (arterial phase and/or portal phase), without evaluating the equilibrium phase. This analysis was named "first analysis". Then, a new reading was performed combining the findings from all the scan phases, including the equilibrium phase. Such a reading was named "second analysis". For the purpose of results analysis, CT scan findings were divided into two groups, namely, main findings, i.e., those directly related to the clinical indication for the study; and secondary diagnoses, i.e., those not related to the clinical indication and /or incidental findings. The criteria for inclusion in the secondary diagnosis group were consensually established by the observers with basis on data reported in the literature(24). At the end of each evaluation, it was established whether there had been changes in the main and secondary diagnoses from the first in relation to the second analysis. The frequency of changes in the main and secondary diagnoses was measured, according to the clinical indication, after comparing the first and second analyses. An extension of the Fisher's exact test was utilized to evaluate the modification of the main diagnoses, considering results with p < 0.05 as being statistically significant. As regards secondary diagnoses, a proportional percentage was calculated in relation to the total number of CT scans. RESULTS The main clinical indications for the reviewed CT studies were: 1) oncological indications, comprising staging, restaging and investigation of primary neoplasia, corresponding to 126 studies (57.5%); 2) acute abdomen, comprising inflammatory (28/49), obstruction (8/49), perforation (2/49), vascular involvement (4/49), besides seven cases of acute abdomen whose nature still remained to be clarified, in a total of 49 CT studies (22.4%); 3) investigation and follow-up of intra-abdominal collection, corresponding to 31 CT studies (14.2%); and 4) others, corresponding to 13 CT studies (5.9%) whose indications were blunt abdominal trauma, foreign body investigation, post-operative evaluation/follow-up, among others. In five patients with suspected acute appendicitis, and in two with suspected acute diverticulitis, the contrast-enhanced phases were performed, as the non-contrast-enhanced phase alone was not sufficient to establish the diagnosis, thus such cases were included in the present study. In regard to the radiation dose to which the patient was exposed, the estimated average dose per scan was 2.775 mGy*cm (DLP), or about 835 mGy*cm per phase, corresponding to an estimated mean effective dose of 12.5 mSv per phase (minimum = 9 mSv; maximum = 24 mSv). Such calculations originate from 64 patients (29%) who underwent four acquisition phases (non-contrast-enhanced, arterial, portal and equilibrium phases) due to different clinical indications and the scan protocol adopted by the institution; and from 155 patients (71%) who underwent three acquisition phases (non-contrast-enhanced, portal and equilibrium phases). The measured radiation dose was similar in the different imaging phases for each patient (non-contrast-enhanced, arterial, portal and equilibrium phases) in the study sample. Among all the evaluated patients, only one had a change in the main diagnosis after the second analysis (0.46%; p > 0.999; not significant). Such case was a patient in restaging for colon neoplasia, with no available previous image, with undetermined nodule in the right adrenal gland evaluated at the non-contrast-enhanced and portal phases. After evaluation of the equilibrium phase, it was observed that the nodule presented wash-out > 50%, characterizing the presence of an adenoma (Figure 1). The remaining clinical indications did not present any change in the main diagnosis. 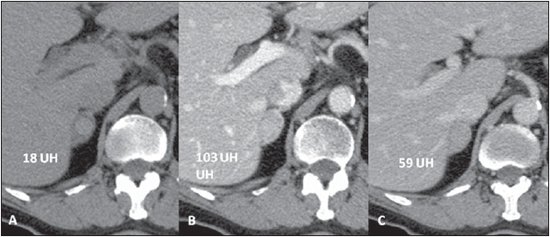 Figure 1. Nodule in the right adrenal gland, in a patient undergoing colon neoplasia restaging, with a density of 18 UH, 103 UH and 59 UH, respectively, at the non-contrast-enhanced phase (A), portal phase (B) and equilibrium phase (C). The absolute wash-out was 52%. As regards the secondary diagnoses, there were five studies with modifications after the second analysis. There were diagnostic doubts about the characterization of bilateral delayed renal excretion (in one case of acute abdomen and one case of investigation of intracavitary collection), both confirmed at the equilibrium phase; and differentiation between focal caliectasis and parapyelic cyst, confirmed at the equilibrium phase (in one case of acute abdomen, one case of intracavitary collection investigation and one case of abdominal trauma), corresponding to a total of 2.3% of changes in secondary diagnosis. DISCUSSION Currently, there has been an increasing concern about the control of the radiation dose received by patients in CT scans, and several ways to reduce it have been studied(3,4), among them tube voltage modulation, automatic exposure control, reduction of scan range, peak kilovoltage optimization, use of special filters to reduce skin dose, post-processing of images to increase the signal/noise ratio(5), among others. When such strategies are applied together, a significant reduction is observed in the radiation dose to which the patient is exposed(6), in some specific clinical situations attaining equivalent doses lower than 2 mSv(23), which correspond to three views of plain abdominal radiography or one cranial CT(25). Besides the above mentioned strategies, suppression of one or more imaging phases has been showing to be a feasible and effective alternative(7,11). In the present study, considering the evaluation of a wide range of clinical indications, frequently with four acquisition phases, the authors obtained an estimated mean effective dose of 41.2 mSv per scan, with an average of 12.5 mSv per phase. Therefore, by suppressing the equilibrium phase, the patient radiation exposure would be reduced by 25-33% (25% when considering four acquisition phases, i.e., non-contrast-enhanced, arterial, portal and equilibrium phases; and 33% considering three acquisition phases, i.e., non-contrast-enhanced, portal and equilibrium phases), with undeniable benefit to the patient. It is important to observe that the result obtained from such calculation is not the accurate values of estimated radiation, however it can be utilized as a reference value at a given CT unit, as there are great practical difficulties in measuring the exact dose per patient, because of the wide range of variables involved in the calculation, which are inherent to each patient (for example: body mass index, abdominal circumference, irradiated organ), and to the utilized technical factors (ex.: kV, mAs, pitch, etc.), as demonstrated in the literature(23). However, even by applying such inaccurate calculation method, the radiation dose reduction by suppressing an acquisition phase is undeniable. Some authors have reported that diagnostic accuracy of imaging studies in certain diseases is not impaired when the equilibrium phase is suppressed(8-10). In 2004, Ibriacco et al.(8), evaluating patients with suspected pancreatic neoplasia, demonstrated that the utilization of a single phase after contrast agent injection at multidetector CT is an accurate technique for the diagnosis and staging of this tumor. In 2006, Iezzi et al.(9) demonstrated that the equilibrium phase is not necessary to characterize high output endoleak after abdominal aorta aneurysm surgeries, with 93% sensitivity and 97% specificity. In 2012, Metser et al.(10) proved that the portal phase is more efficient than the equilibrium phase for the characterization of lower and upper urinary tract tumors, so the portal phase alone can characterize such lesions. Considering such current theme in the literature, the present study was aimed at contributing with a different approach where, instead of focusing on a determined disease or clinical situation, some of the main routine indications were addressed, with the purpose of evaluating the main CT scan protocols. In the authors' institution, most of the contrast-enhanced abdominal and pelvic scans are performed for oncologic purposes, comprising diagnosis, staging and restaging. On account of their baseline condition, such patients undergo study series over their lifetime, thus making the concern with the radiation dose to which they are exposed, more relevant. As demonstrated in the present study, the equilibrium phase presented added value in only one of 219 scans, corresponding to a patient undergoing colon neoplasia restaging, with no previous image available, and who presented a nodule in the adrenal gland with 18 UH attenuation at the contrast-enhanced phase (Figure 1). Such diagnostic doubt is relatively common in abdominal CT for tumors staging. Adrenal nodules correspond to metastasis in 45-73% of oncologic patients(26), and in these cases the differentiation between benign lesions and metastasis is crucial to define the management strategy. The protocol for the appropriate characterization of adrenal nodules consists encompasses a non-contrast-enhanced phase, a portal phase and a delayed phase 10 to 15 minutes after contrast injection(21), with no need for the performance of the equilibrium phase 3 to 5 minutes following the contrast injection. Several authors have demonstrated that it is possible to characterize an adrenal nodule as adenoma by calculating the wash-out with high sensitivity and specificity(27-29). In the present study, the analysis of images obtained at the equilibrium phase has allowed suggesting that the adrenal nodule in the patient was probably of a benign origin, based on the calculation of absolute wash-out > 50% and confirmed by the lesion stability, at the imaging follow-up after 12 months. On the other oncologic studies and on those for investigation of acute abdomen and intra-abdominal collection, no changes were observed in the primary diagnoses. As regards secondary diagnoses, the authors observed some changes which could be better characterized in the second analysis. In two cases whose indications were acute abdomen investigation and collection investigation, the first analysis could not demonstrate the delayed contrast medium clearance (Figure 2), a finding which is typically characterized only at the equilibrium phase, suggesting decreased renal function. However, it is important to remember that CT is not the method of choice to investigate the renal function. For such a purpose, urea and creatinine tests are the methods of choice; hence the lower clinical significance of not identifying the impaired renal function at the tomographic images, on account of the equilibrium phase suppression, since the diagnosis was made by means of the mentioned laboratory tests. 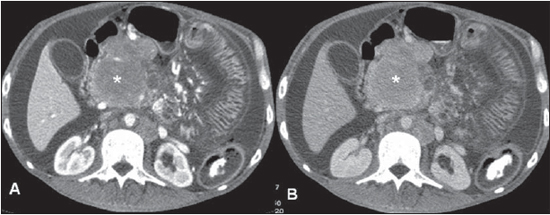 Figure 2. Patient with small bowel lymphoma. As secondary finding there are signs of renal excretion deficit characterized by delayed clearance of the intravenous contrast medium at the equilibrium phase (B), not suspected at the portal phase (A). There was diagnostic doubt in three cases, in the differentiation between focal caliectasis and parapyelic cyst, as the equilibrium phase was not evaluated (Figure 3). Focal caliectasis corresponds to a small dilation of one or more renal calyces typically of cicatricial/residual origin, while parapyelic cysts are simple cystic masses originated at the medial portion of the renal parenchyma, projecting into the renal sinus(30). Both situations, when asymptomatic, require a conservative approach, and in the present study they were classified as being of low clinical relevance, in agreement with data in the literature(24). Thus, despite the difficulty in differentiating focal caliectasis and parapyelic cysts at the first analysis, such a fact would not represent a significant practical impact on the approach to those cases. 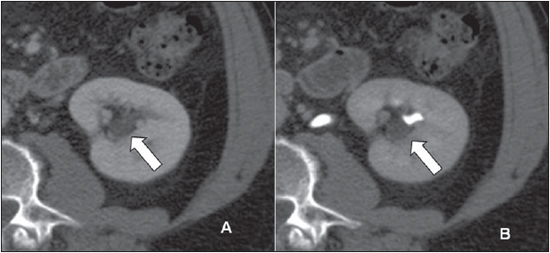 Figure 3. Staging CT in a patient with metastatic melanoma. As a secondary diagnosis, a cystic image was observed adjacent to the renal hilum (arrow), at the portal phase (A). At the equilibrium phase, the cystic image did not present contrast enhancement, proving to be a parapyelic cyst. As a further reasoning, in the six cases where diagnostic information were added after the second analysis, either regarding the main diagnosis (one case) or the secondary diagnosis (five cases), the isolated evaluation of the first analysis would not have determined a harmful therapeutic approach to the patients, as in cases of inconclusive first analysis, there would be the possibility of further investigation, defining the diagnosis. Additionally, the availability of image manipulation tools on the workstation allows changing the CT window level and width, improving the diagnostic capacity of each image acquisition phase isolatedly, contrary to what occurs at hard copy readings(31). A study reviewing 200 chest and abdomen CT images has found significant changes in the final diagnoses in 18% of the images, with an additional reading time of 40 seconds, when resorting to manipulation of visualization window parameters(32). Most recently, the use of dual energy CT has demonstrated the possibility of reducing the radiation dose, by suppressing the non-contrast-enhanced phase in several clinical indications(33), with encouraging results, but questionable in some cases, such as in the characterization of adrenal nodules, where the method presented high specificity, but low sensitivity(34,35). Further studies will be necessary to establish the actual value of the method in different clinical scenarios, also taking the availability of such type of equipment in our environment into consideration. The main limitation in the present study was the fact that on account of the usual profile of the patients seeking the authors' institution, the analysis of the impact of suppressing the equilibrium phase was performed in a universe of clinical indications which, in spite of being comprehensive, had a small number of cases in some situations, such as blunt abdominal trauma and foreign body investigation, among others, thus limiting the power of analysis of the study in such clinical situations. However, such spectrum and distribution of clinical indications represent not only the reality in the authors' institution, but also in many other services where indications for CT in the evaluation of oncologic patients, in the diagnosis of acute abdomen and in the investigation of intracavitary collection correspond to an expressive number of cases. The impact of equilibrium phase suppression in less frequent clinical situations could be evaluated in subsequent studies. Other limitation to be mentioned is related to the retrospective nature and to the comprehensiveness of the study. However, as the objectives of the present study are considered, one will realize that the methodological model did not affect the investigation results. The authors proposed reproducing the environment of indications faced by CT services in general or in university hospitals such as the authors' institution, with an expressive number not only of outpatients, but also inpatients and patients coming from emergency room, establishing the role of the equilibrium phase in the diagnostic evaluation of abdominal CT scans. In this context, the authors understand having contributed to the suppression, in determined clinical situations, of an apparently unnecessary imaging phase. Further studies may be undertaken in order to confirm the present study results. It is also important to observe that, in spite of the current utilization of the equilibrium phase on a routine basis in Brazil, in other countries such imaging phase has only been indicated for a few clinical situations. Finally, the analysis of the present study results allowed the conclusion that the equilibrium phase can be suppressed in abdominal CT scans for the main oncologic indications, investigation of acute abdomen and investigation/follow-up of intracavitary collection, with no significant loss of the diagnostic capability of the method. REFERENCES 1. Dalmazo J, Elias Jr J, Brocchi MAC, et al. Otimização da dose em exames de rotina de tomografia computadorizada: estudo de viabilidade em um hospital universitário. Radiol Bras. 2010;43:241-8. 2. Huda W. What ER radiologists need to know about radiation risks. Emerg Radiol. 2009;16:335-41. 3. Kalra MK, Maher MM, Toth TL, et al. Strategies for CT radiation dose optimization. Radiology. 2004;230:619-28. 4. Kalender WA, Buchenau S, Deak P, et al. Technical approaches to the optimisation of CT. Phys Med. 2008;24:71-9. 5. Yu L, Liu X, Leng S, et al. Radiation dose reduction in computed tomography: techniques and future perspective. Imaging Med. 2009;1:65-85. 6. McCollough CH, Bruesewitz MR, Ko?er JM Jr. CT dose reduction and dose management tools: overview of available options. Radiographics. 2006;26:503-12. 7. Leite APK, Mattos LA, Pinto GADH, et al. O valor da fase sem contraste na tomografia computadorizada do abdome. Radiol Bras. 2008;41:289-96. 8. Imbriaco M, Megibow AJ, Ragozzino A, et al. Value of the single-phase technique in MDCT assessment of pancreatic tumors. AJR Am J Roentgenol. 2005;184:1111-7. 9. Iezzi R, Cotroneo AR, Filippone A, et al. Multidetector CT in abdominal aortic aneurysm treated with endovascular repair: are unenhanced and delayed phase enhanced images effective for endoleak detection? Radiology. 2006;241:915-21. 10. Metser U, Goldstein MA, Chawla TP, et al. Detection of urothelial tumors: comparison of urothelial phase with excretory phase CT urography - a prospective study. Radiology. 2012;264:110-8. 11. Hamilton JD, Kumaravel M, Censullo ML, et al. Multidetector CT evaluation of active extravasation in blunt abdominal and pelvic trauma patients. Radiographics. 2008;28:1603-16. 12. Dawson P, Morgan J. The meaning and significance of the equilibrium phase in enhanced computed tomography of the liver. Br J Radiol. 1999;72:438-42. 13. Liu YI, Kamaya A, Jeffrey RB, et al. Multidetector computed tomography triphasic evaluation of the liver before transplantation: importance of equilibrium phase washout and morphology for characterizing hypervascular lesions. J Comput Assist Tomogr. 2012;36:213-9. 14. Sahara S, Kawai N, Sato M, et al. Differentiation of pancreatic serous cystadenoma from endocrine tumor and intraductal papillary mucinous neoplasm based on washout pattern on multiphase CT. J Comput Assist Tomogr. 2012;36:231-6. 15. Kim SK, Lim JH, Lee WJ, et al. Detection of hepatocellular carcinoma: comparison of dynamic three-phase computed tomography images and four-phase computed tomography images using multidetector row helical computed tomography. J Comput Assist Tomogr. 2002;26:691-8. 16. Wong YC, Wang LJ, Fang JF, et al. Multidetectorrow computed tomography (CT) of blunt pancreatic injuries: can contrast-enhanced multiphasic CT detect pancreatic duct injuries? J Trauma. 2008;64:666-72. 17. Marconato JA, Mazzola AA, Sanvitto PC, et al. Redução de dose e aumento na vida útil do tubo de raios X em tomografia computadorizada. Radiol Bras. 2004;37:351-6. 18. Baron RL, Peterson MS. From the RSNA refresher courses. Screening the cirrhotic liver for hepatocellular carcinoma with CT and MR imaging: opportunities and pitfalls. Radiographics. 2001;21 Spec No:S117-32. 19. Kawashima A, Vrtiska TJ, LeRoy AJ, et al. CT urography. Radiographics. 2004;24 Suppl 1:S35-58. 20. Joffe SA, Servaes S, Okon S, et al. Multi-detector row CT urography in the evaluation of hematuria. Radiographics. 2003;23:1441-56. 21. Johnson PT, Horton KM, Fishman EK. Adrenal imaging with multidetector CT: evidence-based protocol optimization and interpretative practice. Radiographics. 2009;29:1319-31. 22. Huda W, Ogden KM, Khorasani MR. Converting dose-length product to effective dose at CT. Radiology. 2008;248:995-1003. 23. Birnbaum S. Radiation protection in the era of helical CT: practical patient based programs for decreasing patient exposure. Semin Ultrasound CT MR. 2010;31:46-52. 24. Hara AK, Johnson CD, MacCarty RL, et al. Incidental extracolonic findings at CT colonography. Radiology. 2000;215:353-7. 25. Davies HE, Wathen CG, Gleeson FV. Risks of exposure to radiological imaging and how to minimise them. BMJ. 2011;342:589-93. 26. Barzon L, Sonino N, Fallo F, et al. Prevalence and natural history of adrenal incidentalomas. Eur J Endocrinol. 2003;149:273-85. 27. Korobkin M, Brodeur FJ, Francis IR, et al. CT time-attenuation washout curves of adrenal adenomas and nonadenomas. AJR Am J Roentgenol. 1998;170:747-52. 28. Mayo-Smith WW, Boland GW, Noto RB, et al. State-of-the-art adrenal imaging. Radiographics. 2001;21:995-1012. 29. Lockhart ME, Smith JK, Kenney PJ. Imaging of adrenal masses. Eur J Radiol. 2002;41:95-112. 30. Rha SE, Byun JY, SE Jung, et al. The renal sinus: pathologic spectrum and multimodality imaging approach. Radiographics. 2004;24 Suppl 1:S117-31. 31. Eberhardt SC, Johnson JA, Parsons RB. Oncology imaging in the abdomen and pelvis: where cancer hides. Abdom Imaging. 2012 Aug 9. [Epub ahead of print]. 32. Pomerantz SM, White CS, Krebs TL, et al. Liver and bone window settings for soft-copy interpretation of chest and abdominal CT. AJR Am J Roentgenol. 2000;174:311-4. 33. Hartman R, Kawashima A, Takahashi N, et al. Applications of dual-energy CT in urologic imaging: an update. Radiol Clin North Am. 2012;50:191-205. 34. Gupta RT, Ho LM, Marin D, et al. Dual-energy CT for characterization of adrenal nodules: initial experience. AJR Am J Roentgenol. 2010;194:1479-83. 35. Johnson PT, Fishman EK. Routine use of precontrast and delayed acquisitions in abdominal CT: time for change. Abdom Imaging. 2012 Nov8. [Epub ahead of print]. 1. MD, Resident, Department of Diagnostic Imaging, Fellow Master degree, Professional Master's Program Associated with Medical Residency (Meparem), Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 2. MDs, Residents, Department of Diagnostic Imaging, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 3. MDs, Fellows, Abdominal Imaging, Department of Diagnostic Imaging, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), MDs, Radiologists, Hospital São Luiz, São Paulo, SP, Brazil. 4. Associate Professor, Department of Diagnostic Imaging, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 5. PhD, Assistant Physician, Department of Diagnostic Imaging, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 6. Associate Professor, Department of Diagnostic Imaging, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. Mailing Address: Dr. Giuseppe D'Ippolito Departamento de Diagnóstico por Imagem - EPM-Unifesp Rua Napoleão de Barros, 800, Vila Clementino São Paulo, SP, Brazil, 04024-002 E-mail: giuseppe_dr@uol.com.br Received October 24, 2012. Accepted after revision January 10, 2013. * Study developed in the Department of Diagnostic Imaging, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554