Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 6 - Nov. / Dec. of 2012
Vol. 45 nº 6 - Nov. / Dec. of 2012
|
CASE REPORT
|
|
Caroli's disease complicated with liver abscess: case report |
|
|
Autho(rs): Artur Guimarães Filho1; Luiz Augusto Carneiro Neto2; Michel Santos Palheta3; Priscila Távora Campos4; Lorena Machado Santos5; Bárbara Góis Cordeiro Barroso4 |
|
|
Keywords: Caroli's disease; Magnetic resonance cholangiography; Liver abscess. |
|
|
Abstract: INTRODUCTION
Caroli's disease is a rare congenital malformation characterized by multifocal dilatation of intrahepatic bile ducts, described by Caroli and collaborators in 1958. The ecstatic segments form cysts of varied sizes separated by normal or poorly dilated bile ducts(1). The disease results from an embryonic derangement of the bile ducts. As major bile ducts are affected, the result is Caroli's disease, whereas abnormality affecting small ducts results in congenital hepatic fibrosis. In cases where the whole biliary tree is involved, findings of both congenital fibrosis and Caroli's disease are present, corresponding to a condition that is known as Caroli's syndrome(1). The multifocal dilation may either be diffuse, affecting the whole intrahepatic biliary tree, or may be confined to part of the liver. The authors describe the case of a patient with Caroli's disease complicated with a liver abscess, with emphasis on clinical and radiological findings. CASE REPORT A previously healthy, male, 16-year-old patient admitted with complaints of pain in the right hypochondrium associated with jaundice, vomiting and daily fever peaks with chills, whose onset occurred seven days before his admission. Physical examination revealed a regular general condition, icterus (2+/4+), tachycardia, abdomen with subtle hepatosplenomegaly. Laboratory tests results were the following: Hb: 10.5 g/dl; VCM: 82 fl; CHCM: 33 g/dl; leukocytes: 12000/mm3; total bilirrubin: 10.0 mg/dl (direct: 4.5 mg/dl and indirect: 5.5 mg/dl); alkaline phosphatase: 237 U/l; gamma-GT: 292 U/l. Normal liver function and transaminase. Magnetic resonance imaging and magnetic resonance cholangiography revealed cystic dilatation of intrahepatic bile ducts, but with common hepatic duct with normal dimensions (Figures 1 and 2). 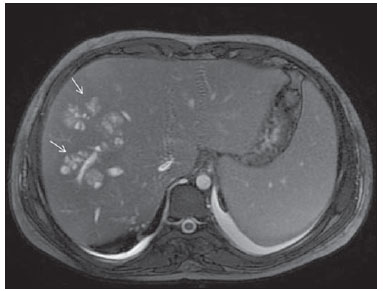 Figure 1. Abdominal magnetic resonance imaging. Axial section, FSE, T2-weighted image showing subtle cystic dilatation of intrahepatic bile ducts in the right hepatic lobe. 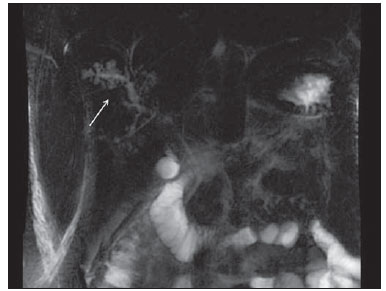 Figure 2. Magnetic resonance cholangiography demonstrating cystic dilatation of intrahepatic bile ducts in the right hepatic lobe. After hospital admission and antibiotic treatment for seven days, the patient progressed with symptoms remission and was discharged, with follow-up on an out-patient basis. Seven days after being discharged, the patient came back with recurrent fever and pain in the right hypochondrium. Abdominal ultrasonography revealed the presence of a liver abscess measuring 5.0 cm in diameter (Figure 3), confirmed by magnetic resonance cholangiography (Figure 4). The patient underwent open surgical drainage and progressed with symptoms remission and abscess healing, being discharged with instructions to maintain regular follow-up.  Figure 3. Abdominal ultrasonography: well defined cystic lesions with thickened, hyper-refringent septa, located in the hepatic segment VII, with adjacent satellite lesions, suggesting the presence of liver abscess. 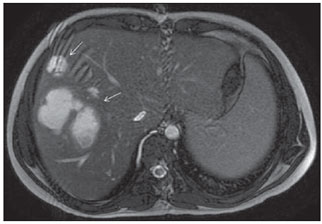 Figure 4. Abdominal magnetic resonance imaging. Axial section, FSE T2-weighted image demonstrating cystic dilatation in intra-hepatic bile ducts in the right hepatic lobe complicated with liver abscess. DISCUSSION Although structural changes in Caroli's disease are already present at birth, the disease is frequently diagnosed around the age of 20, with onset of abdominal pain, fever, hyperbilirrubinemia, increase in alkaline phosphatase levels, hepatomegaly or symptoms of portal hypertension in most of the patients(2). Most rarely, the disease may remain asymptomatic throughout life, being diagnosed by imaging studies requested for evaluation of other non-related conditions. The structural alterations predispose to cholestasis and recurrent episodes of acute cholangitis, and may complicate with development of intrahepatic biliary calculi, liver abscess and sepsis(3). Additionally, there is a relative risk of 7% to 24% for development of cholangiocarcinoma(4). In most of the patients, the first episode of cholangitis occurs in the absence of a triggering factor, but new episodes may occur after surgery or invasive examinations of bile ducts, such as cholecystectomy, choledocotomy or retrograde endoscopic cholangiopancreatography (RECP). The primary symptom of bacterial cholangitis is fever, without abdominal pain and jaundice. Such finding is in contrast to those of cholangitis triggered by biliary calculus, which is associated with abdominal pain, jaundice, or both. Frequently, the liver is increased in volume, with no alteration in laboratory tests results, except for increase in alkaline phosphatase and gamma-GT levels, as observed in the present case. In Caroli's disease associated with congenital hepatic fibrosis, signs of portal hypertension may be present(3). The radiological diagnosis is established by the visualization of cystic lesions of variable sizes distributed within the liver or in a hepatic segment communicating with the biliary tree, by means of ultrasonography, computed tomography, RECP or magnetic resonance cholangiography. RECP is the most sensitive method for diagnosis of Caroli's disease, but there are evidences that magnetic resonance cholangiography is a noninvasive technique with good diagnostic correlation with RECP, besides being exempt of risks inherent to invasive methods(5). The disease course is marked by recurrent episodes of bacterial cholangitis. Patients with a greater number of episodes in a year present reserved long-term prognosis, with progressive worsening in their quality of life. Generally, the death of such patients is related to the presence of liver abscess and septicemia(5). Partial hepatotectomy may represent a definitive treatment, with acceptable morbidity for focal Caroli's disease, and complete symptoms regression. Diffuse disease complicated with recurrent cholangitis or cirrhosis is of difficult management, and liver transplantation is the only and last option for a definitive treatment(6). REFERENCES 1. Levy AD, Rohrmann CA Jr, Murakata LA, et al. Caroli's disease: radiologic spectrum with pathologic correlation. AJR Am J Roentgenol. 2002;179:1053–7. 2. Millwala F, Segev DL, Thuluvath PJ. Caroli's disease and outcomes after liver transplantation. Liver Transpl. 2008;14:11–7. 3. Habib S, Shaikh OS. Caroli's disease and liver transplantation. Liver Transpl. 2008;14:2–3. 4. Lefere M, Thijs M, De Hertogh G, et al. Caroli disease: review of eight cases with emphasis on magnetic resonance imaging features. Eur J Gastroenterol Hepatol. 2011;23:578–85. 5. Yonem O, Bayraktar Y. Clinical characteristics of Caroli's disease. World J Gastroenterol. 2007;13:1930–3. 6. Wang ZX, Yan LN, Li B, et al. Orthotopic liver transplantation for patients with Caroli's disease. Hepatobiliary Pancreat Dis Int. 2008;7:97–100. 1. Master, Titular Member of Colégio Brasileiro de Cirurgiões, Assistant Professor, Course of Medicine, Universidade Federal do Ceará (UFC) – Campus Sobral, Sobral, CE, Brazil. 2. MD, Universidade Federal do Ceará (UFC) – Campus Sobral, Sobral, CE, Brazil. 3. Master, Titular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MD, Radiologist Assistant, Santa Casa de Misericórdia de Sobral, Sobral, CE, Brazil. 4. Graduate Students of Medicine, Universidade Federal do Ceará (UFC) – Campus Sobral, Sobral, CE, Brazil. 5. MD, Medical Resident, Santa Casa de Misericórdia de Sobral, Sobral, CE, Brazil. Mailing Address: Dr. Luiz Augusto Carneiro Neto Avenida Gerardo Rangel, 754, ap. 205, Pedrinhas Sobral, CE, Brazil, 62041-380 E-mail: luizcarneiro@yahoo.com.br Received April 30, 2012. Accepted after revision July 5, 2012. * Study developed at Course of Medicine, Universidade Federal do Ceará (UFC) – Campus Sobral and at Santa Casa de Misericórdia de Sobral, Sobral, CE, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554