Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 6 - Nov. / Dec. of 2012
Vol. 45 nº 6 - Nov. / Dec. of 2012
|
CASE REPORT
|
|
Primary bone lymphoma simultaneous to osteochondroma simulating sarcomatous degeneration: case report |
|
|
Autho(rs): Laura de Moraes Gomes1; Felipe Augusto Rozales Lopes2; Décio Valente Renck3 |
|
|
Keywords: Primary bone lymphoma; Osteochondroma; Sarcomatous degeneration; Bone tumors. |
|
|
Abstract: INTRODUCTION
Primary bone lymphoma and sarcomatous degeneration secondary to osteochondroma are rare tumors and no relation between such entities is found in the literature. Primary bone lymphoma represents 1% of extranodal non-Hodgkin's lymphomas, occurring predominantly in the sixth and seventh decades of life(1). On the other hand, osteochondroma represents 20% of benign bone tumors and usually is found in the second and third decades of life. Malignant transformation if found in 1% of cases of solitary osteochondromas(2). Since no study reporting the concomitant presence of these two tumors in a single bone region has been found in the literature, the present report is aimed at describing a case of primary bone lymphoma simultaneous to osteochondroma which, at imaging studies, simulated sarcomatous degeneration in the proximal third of the tibia. CASE REPORT A 65-year-old, male patient with no history of trauma presented intense and disabling pain in the proximal third of his tibia for nine months. At physical examination a small palpable mass was found with local sensation of heat. Radiography demonstrated the presence of an osteochondroma in the posterosuperior portion of the tibia with radiolucent areas and centrally located radiodense areas suggesting the presence of calcifications within the osteochondroma (Figure 1). Magnetic resonance imaging (MRI) revealed the presence of an infiltrative bone lesion with heterogeneous contrast enhancement and marked bone marrow infiltration extending to the adjacent soft tissues, with no noticeable cortical bone destruction. MRI also demonstrated intra-articular compromise by the lesion and bone marrow involvement by the osteochondroma. Such imaging findings were initially interpreted as sarcomatous degeneration secondary to osteochondroma (Figures 2, 3 and 4).  Figure 1. Radiological findings compatible with osteochondroma located on the postero-superior margin of the proximal tibia. Radiodense areas (arrow) are observed, suggesting the presence of calcifications within the osteochondroma. 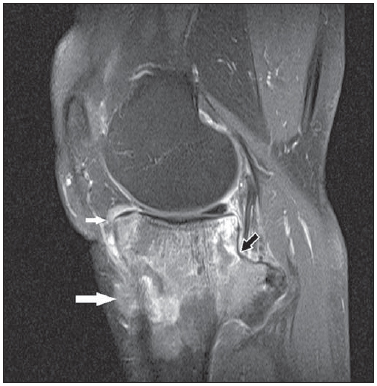 Figure 2. Sagittal MRI T1-weighted image with fat saturation demonstrating neoplastic involvement of osteochondroma (black arrow), intra-articular compromise by the tumor (smaller white arrow), as well as lesion extension towards soft tissues (larger white arrow). 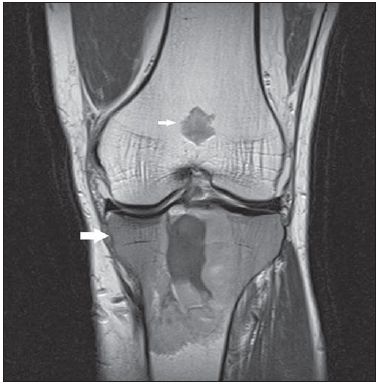 Figure 3. Coronal MRI T1-weighted image showing an infiltrative lesion in the proximal epiphysis and diaphysis of the tibia (larger arrow). A focal, well-defined bone lesion is observed in the femoral metaphysis (smaller arrow) with lobular configuration and presence of calcifications, suggestive of chondroma. 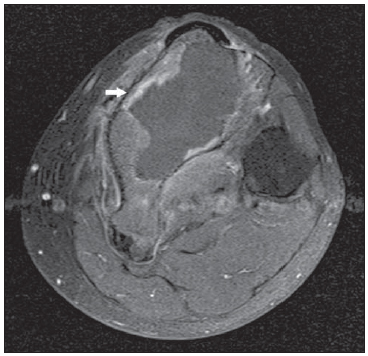 Figure 4. Post-gadolinium, axial MRI T1-weighted with fat saturation showing contrastenhanced infiltrative lesion (arrow) with relatively preserved cortical bone.. Additionally to the infiltrative lesion identified in the tibia, a well-defined focal lesion was found in the bone marrow of the femoral metaphysis, with hyposignal on Tl-weighted sequences, lobular configuration and presence of calcifications suggestive of chondroma. Biopsy identified a diffuse peripheral B-cell non-Hodgkin's lymphoma, with positive CD20, CD3, CD5 markers; and staging computed tomography (CT) did not demonstrate the presence of enlarged lymph nodes, which confirmed primary bone lymphoma. It is important to note that among the described imaging findings, the cortical bone was relatively preserved, even with the adjacent soft tissues infiltration, corroborating the histopathological diagnosis of lymphoma. DISCUSSION According to Nava et al.(3), MRI has been utilized for staging lymphomas because of its high sensitivity for detecting malignant tumors, constituting an excellent alternative to the method utilized in the present study, CT. Primary bone lymphoma is characterized by intermittent local pain that may persist for months(4). It is commonly located in long bones, preferentially in the femur and pelvic bones. Primary bone lymphomas originated in the center of the bone may disrupt the cortical bone as the medullary cavity is already occupied by the lesion and there is a risk for involvement of soft tissues(5). As regards the radiological appearance of bone lymphomas, there is a permeative or motheaten pattern, causing periosteal reaction. The most common pattern is the lytic-destructive one, with radiolucent foci on an ill delimited area. A blastic/sclerotic pattern may be observed, although rarely as compared with bone metastases from lymphoma. At MRI, Tl-weighted sequences are the most appropriate to demonstrate medullary changes, showing areas of hyposignal within the bone marrow. Both on T2-weighted sequences and fluid-sensitive MRI sequences with fat suppression demonstrate areas of hypersignal. In cases of radiological permeative pattern, soft tissues involvement is observed. Both CT and MRI reveal cortical bone erosion(6). Like bone lymphomas, osteochondromas are most commonly found in long bones, particularly the humerus and the femur, and are preferentially located in metaphyseal regions. Osteochondromas present easily recognisable radiological signs at conventional radiography, demonstrating cortical and spongy bone continuity with adjacent bone tissues. Both MRI and CT confirm such characteristic. The radiological aspect of sarcomatous degeneration includes characteristics of osteochondroma growth with irregular surface, focal regions of radiolucency within the lesion, erosion or destruction of adjacent bone tissues. MRI characterizes low-grade chondrosarcomas with hypersignal on T2-weighted sequences and hyposignal on tumor septations with post-contrast enhancement(7). The definitive diagnosis of bone lymphoma is achieved by means of histological study of the lesion. For immunohistochemical diagnosis, LCA, CD20 and CD3 markers should be investigated(8). The differential diagnosis includes osteosarcoma, Ewing's tumor and neoplastic metastases(5). Finally, the occasional finding of an osteochondroma simultaneous to a bone lymphoma in a single bone region has raised doubts regarding the imaging diagnosis, initially leading to the belief that the findings corresponded to sarcomatous degeneration secondary to osteochondroma. Additionally, the diagnostic difficulty was determined by the disease rarity, and hence the relevance of differential diagnoses should be emphasized. REFERENCES 1. Krishnan A, Shirkhoda A, Tehranzadeh J, et al. Primary bone lymphoma: radiographic-MR imaging correlation. Radiographics. 2003;23:1371-83. 2. Kurimori CO, Bordalo-Rodrigues M, Cerri GG. Degeneração maligna para condrossarcoma de um osteocondroma pediculado da tíbia. Radiol Bras. 2010;43(1):xi-xii. 3. Nava D, Oliveira HC, Luisi FA, et al. Aplicação da ressonância magnética de corpo inteiro para o estadiamento e acompanhamento de pacientes com linfoma de Hodgkin na faixa etária infanto-juvenil: comparação entre diferentes sequências. Radiol Bras. 2011;44:29-34. 4. Pires de Camargo O, Machado TMS, Croci AT, et al. Primary bone lymphoma in 24 patients treated between 1955 and 1999. Clin Orthop Relat Res. 2002;(397):271-80. 5. Edeiken J. Diagnóstico radiológico de las enfermedades de los huesos. 3ª ed. Buenos Aires: Editorial Medica Panamericana; 1984; p. 66-73, 30314. 6. Gomes FSE, Lewin F, Mariotti GC, et al. Osteocondromas: avaliação por imagem das complicações. Rev Imagem. 2007;29:53-9. 7. Hicks DG, Gokan T, O'Keefe RJ, et al. Primary lymphoma of bone. Correlation of magnetic resonance imaging features with cytokine production by tumor cells. Cancer. 1995;75:973-80. 8. Neupatimagem-Unicamp. Linfoma não-Hodgkin de grandes células B de osso occipital, com extensão intra- e extracraniana. [acessado em 15 de dezembro de 2011]. Disponível em: http://anatpat.unicamp.br/xnptlinfoma3.html 1. Master, MD, Radiologist, Hospital Santa Casa de Misericórdia de Pelotas, Pelotas, RS, Brazil. 2. Graduate Student (6th year) of Medicine, Universidade Católica de Pelotas (UCPel), Pelotas, RS, Brazil. 3. Master, MD, Radiologist, Chief of the Center of Imaging Diagnosis, Hospital Santa Casa de Misericórdia de Pelotas, Pelotas, RS, Brazil. Mailing Address: Felipe Augusto Rozales Lopes Rua Emílio Jorge dos Reis, 512, Três Vendas Pelotas, RS, Brazil, 96020440 E-mail: felipearlopes@gmail.com Received February 24, 2012. Accepted after revision July 5, 2012. * Study developed in the Center of Imaging Diagnosis at Hospital Santa Casa de Misericórdia de Pelotas, Pelotas, RS, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554