Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 5 - Sep. / Oct. of 2012
Vol. 45 nº 5 - Sep. / Oct. of 2012
|
CASE REPORT
|
|
Anterior tibial artery recanalization through dorsalis pedis artery: a case report* |
|
|
Autho(rs): Abdo Farret Neto1; Eduardo Dantas Baptista de Faria2; Ernesto Pantaleo3; Marcelo José Carlos Alencar4; George Anderson da Penha Andrade4; Célia Maria Guedes de Lima5 |
|
|
Keywords: Angioplasty; Arterial occlusive disease; Percutaneous transluminal angioplasty; Tibial arteries; Endovascular procedures. |
|
|
Abstract: INTRODUCTION
Diabetic arteriopathy is one of the main disorders referred to centers for treatment of peripheral ischemias. Revascularization of tibial arteries is frequently required for such treatment(1-3). The development of new dedicated techniques and materials compatible with the anatomical and stenotic characteristics of affected vessels, particularly the tibial vessels, in most cases, allows the reestablishment of the distal blood flow to the foot by means of angioplasty of at least one of such vessels(1,3). However, a recent study has reported the failure in approximately 20% of most complex cases where the antegrade approach was utilized for revascularization(4). Thus, in the setting of failure by the antegrade approach in overcoming the lesion, angioplasty by retrograde approach can be utilized(5). CASE REPORT A female, 79 year-old diabetic patient with hypertension and coronary artery disease. The patient presented with ischemic ulcers in her left leg, with slow course in spite of the instituted clinical treatment. The patient had normal popliteal and femoral pulses and absence of pulses in the left foot. The ankle-brachial index (ABI) at the dorsalis pedis artery was 0.58. Angiography demonstrated segmental occlusion in the proximal third of the anterior tibial artery and occlusion of the fibular and posterior tibial arteries (Figure 1).  Figure 1. Segmental occlusion of the left anterior tibial artery (arrows). Observe the absence of opacification of the fibular and posterior tibial arteries. Treatment with acetylsalicylic acid 100 mg/day + clopidogrel 75 mg/day was initiated and anterior tibial artery recanalization by means of homolateral antegrade approach was indicated. After the positioning of a 5F long introducer sheath (Angio-Line®; Biometrix, Jerusalem, Israel), heparinization was initiated according to the protocol utilized in the authors' institution, as follows: continuous drip at 40 drops/ minute through the sheath (20 UI of heparin per minute) of a solution obtained from the dilution of 5000 UI in 500 ml of 0.9% saline solution. After unsuccessful attempts to overcome the occlusion, the antegrade approach was abandoned. The retrograde approach through the dorsalis pedis artery was adopted utilizing a Jelco® 21 G device guided by the roadmap obtained by infusion of contrast media through the femoral sheath. A 0.018" × 300 cm J-type guidewire (Scitech®; Goiânia, GO, Brazil) was inserted and the anterior tibial artery occlusion was successfully overcome without difficulties. The flexible tip of the guidewire end exited after negotiating its penetration into the distal end of a Cobra1 5F catheter which was partially inserted in the 5F sheath, thus allowing the hemostatic valve to be overcome. The rigid end of the guidewire was kept outside the dorsal region of the foot (Figure 2). A Passeo® 2.5 × 80 × 130 (Biotronik Ag®, Bulach, Switzerland) balloon was inserted through the end of the femoral sheath and then inflated up to a nominal pressure of 6 atmospheres (Figure 3). Angiographic follow-up demonstrated a good flow along the entire anterior tibial artery and spasm of the dorsalis pedis artery at the level of the site where the guidewire was inserted (Figure 4). The guidewire was removed through the femoral path, considering that the length of guidewire passing through the dorsalis pedis artery would be smaller. After the guidewire removal, the dorsalis pedis artery was gently compressed during 10 minutes, and no bleeding or hematomas were observed in the location. The ABI measured on the left dorsalis pedis artery 24 hours after the procedure was 0.62. The patient progressed with stable palpable pedal pulse (+++/++++) and healing of the lesions within three weeks.  Figure 2. Guidewire implanted in the dorsalis pedis artery (arrow), with ischemic lesions being also observed in the leg.  Figure 3. Inflated 2.5 × 80 balloon. 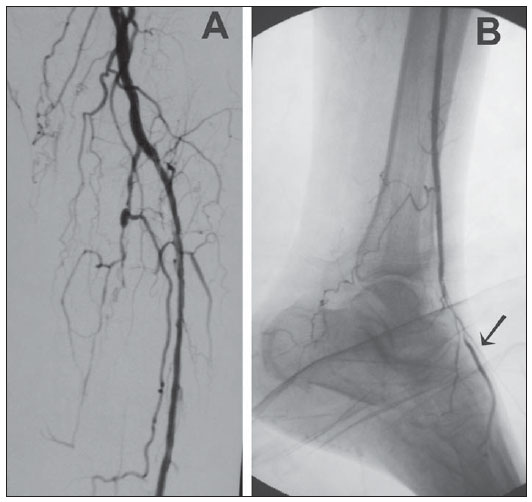 Figure 4. Follow-up angiography. Observe the dorsalis pedis artery spasm and the exteriorized guidewire (arrow on B). DISCUSSION In endovascular therapeutics, different techniques and devices may be utilized during a single procedure(5). Recanalization of lower limb arteries is routinely performed by antegrade approach, but sometimes it is impossible to overcome certain occlusions through this path(6). Among the techniques utilized in cases of occlusive conditions, subintimal angioplasty is highlighted. Such technique is not always successful, with its incapability of re-entering the true lumen of the vessel and perforations being the main reasons for failures(7). It is interesting to observe the difference between retrograde angioplasty and angioplasty by means of distal retrograde puncture. In retrograde angioplasty, the percutaneous access is the conventional one - femoral, for example -, taking advantage of the existence of patent anatomical pathways such as the plantar arch or collaterals, in order to retrogradely reach the lesion(7). In the retrograde puncture, the percutaneous access is obtained distally to the lesion to be treated - in the foot for example -, and from that peripheral point, the guidewire is inserted. Some technical particularities are highlighted in the present case: the non-utilization of systemic full heparinization, as per the authors' long-standing routine(8); the passage of the guidewire within the dorsalis pedis artery through the Jelco® 21G device without utilizing an introducer, thus avoiding unnecessary trauma and facilitating the hemostasis after the procedure completion; the puncture obtained by means of roadmapping instead of echo Doppler, which makes the access possible even in cases where such imaging equipment is not available, besides avoiding the need of surgical exposure of the vessel to be punctured. REFERENCES 1. Graziani L, Silvestro A, Bertone V, et al. Vascular involvement in diabetic subjects with ischemic foot ulcer: a new morphologic categorization of disease severity. Eur J Vasc Endovasc Surg. 2007;33:453-60. 2. Hynes N, Mahendran B, Manning B, et al. The in?uence of subintimal angioplasty on level of amputation and limb salvage rates in lower limb critical ischaemia: a 15-year experience. Eur J Vasc Endovasc Surg. 2005;30:291-9. 3. Kawarada O, Yokoi Y, Sekii H, et al. Retrograde crossing through the pedal arch for totally occluded tibial artery. J Interv Cardiol. 2008;21:342-6. 4. Rogers RK, Dattilo PB, Garcia JA, et al. Retrograde approach to recanalization of complex tibial disease. Catheter Cardiovasc Interv. 2011;77:915-25. 5. Graziani L, Morelli LG. Combined retrogradeantegrade arterial recanalization through collateral vessels: rede?nition of the technique for below-theknee arteries. Cardiovasc Intervent Radiol. 2011;34 Suppl 2:S78-82. 6. Bozlar U, Shih MCP, Harthun NL, et al. Outback catheter-assisted simultaneous antegrade and retrograde access for subintimal recanalization of peripheral arterial occlusion. Clin Imaging. 2008;32:236-40. 7. Biondi-Zoccai GC, Bollati M, Moretti C, et al. Retrograde percutaneous recanalization of coronary chronic total occlusions: outcomes from 17 patients. Int J Cardiol. 2008;130:118-20. 8. Farret Neto A, Faria EB, Laurentino A. Angioplastia infra-inguinal em pacientes com isquemia crítica grau III, categoria 5 de Rutherford. Radiol Bras. 2008;41:173-6. 1. Full Member of Colégio Brasileiro de Cirurgiões (CBC) and Sociedade Brasileira de Angiologia e Cirurgia Vascular (SBACV), Professor, Faculdade de Medicina da Universidade Federal do Rio Grande do Norte (UFRN), Angioradiologist and Vascular Surgeon, Hospital Universitário Onofre Lopes, Natal, RN, Brazil. 2. Professor, Faculdade de Medicina da Universidade Federal do Rio Grande do Norte (UFRN), Angiologist and Vascular Surgeon, Hospital Universitário Onofre Lopes, Natal, RN, Brazil. 3. Angiologist, Vascular Surgeon, Vascular Sonographer and Trainee at the Unit of Hemodynamics - Hospital Universitário Onofre Lopes, Natal, RN, Brazil. 4. Graduate Students (6th year), Faculdade de Medicina da Universidade Federal do Rio Grande do Norte (UFRN), Trainees at the Unit of Vascular Surgery and Angioradiology - Hospital Universitário Onofre Lopes, Natal, RN, Brazil. 5. Master of Surgical Nursing, Nurse at Hospital Universitário Onofre Lopes, Natal, RN, Brazil. Mailing Address: Dr. Abdo Farret Neto Rua Doutor Múcio V. Ribeiro Dantas, 500, casa E/27, Ponta Negra. Natal, RN, Brazil, 59092-580 E-mail: abdofarret@gmail.com Received April 3, 2012. Accepted after revision July 2, 2012. * Study developed at Hospital Universitário Onofre Lopes, Natal, RN, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554