INTRODUCTION
Langerhans cell histiocytosis is a rare disease that normally affects children, involving different parts of the body. Its diagnosis is based on histological and immuno-histochemical studies of the lesions. The treatment depends on the form of disease. The present report is aimed at describing the case of a 63-year-old patient affected by the disease, as well as presenting his imaging studies and the whole case progression. At the end, the authors also present a brief review of the literature on the disease.
CASE REPORT
The present report describes the case of a male, 63-year-old patient complaining of proptosis of his right eye for six months. Previous personal history: smoking and alcohol use. The screening for infecto-contagious diseases was negative.
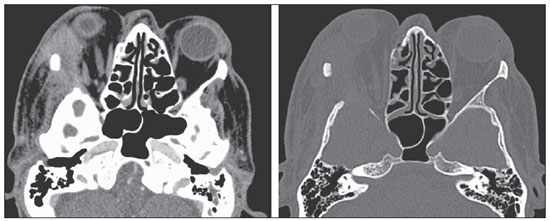
Physical examination did not present any other finding, except the right-sided proptosis itself. Skull computed tomography (Figure 1) revealed a lesion affecting the lateral wall of the orbit (with bone destruction) and the right intraorbital region, externally extending towards the perizygomatic region. Right-sided ocular globe proptosis and invasion of the corresponding lateral extrinsic orbital muscle were observed. Then, the patient was submitted to complete exeresis of the lesion.
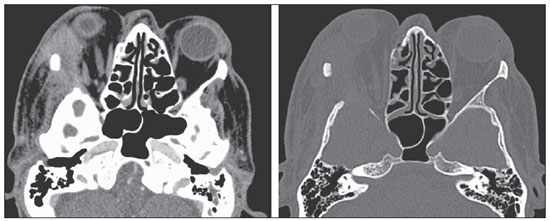
Figure 1. Contrast-enhanced axial computed tomography of skull. Intraorbital expansile lesion extending toward the intra- and extraconal spaces, extracranial soft tissues and bone erosion of the lateral wall (zygomatic bone and major sphenoid wing) of the right orbit.
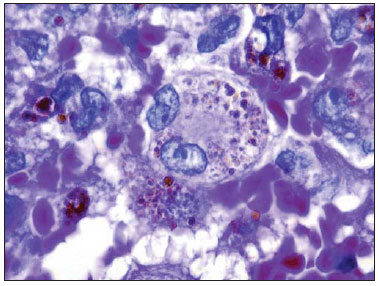
Histopathological study revealed proliferation of abundant macrophages (histiocytes) with epithelioid cells and multinucleated gigantocytes with some figures of mitosis compatible with Langerhans cell histiocytosis (Figure 2).
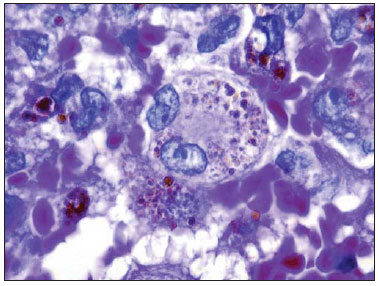
Figure 2. Hematoxylin eosin staining demonstrates fagocytosis of hemosiderin by Langerhans cells recognizable by their irregular nuclei with a round or elongated contour, frequently with cleavage and indentation, loose and welldistributed cromatin.
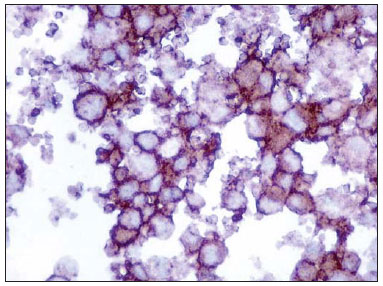
Immuno-histochemical analysis was positive for CD1a, CD 68, HAM56 and S100 in the neoplastic cells, negative for HMB45, AE1, AE3, CD20, CD3, and positive for KI67 in 5-10% of the nuclei, corroborating the diagnostic hypothesis of Langerhans cell histiocytosis (Figure 3).
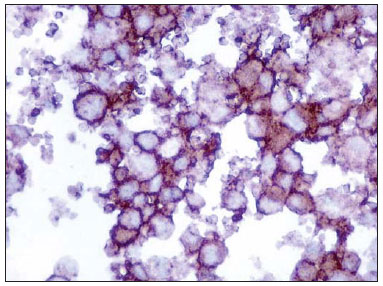
Figure 3. Immuno-histochemical study demonstrates positivity for CD1a with a membranous pattern, which is a
sine qua
non condition for Langerhans cell diagnosis.
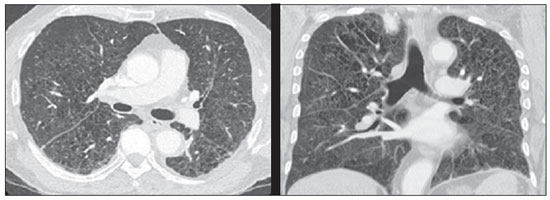
Then, the patient underwent further investigation to determine the presence of additional foci of histiocytosis which demonstrated a lesion in the fifth left coastal arch and the pulmonary involvement typically observed in cases of histiocytosis (Figure 4). The patient underwent hematological follow-up and was submitted to two cycles of chemotherapy with vimblastine, etoposide and prednisone, and progressed to death in February 2012 because of complications resulting from his lung disease.
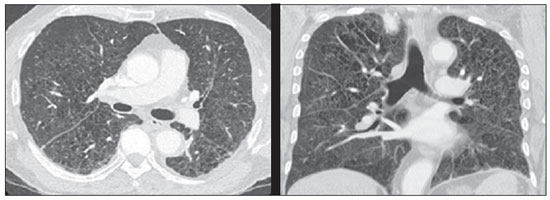
Figure 4. Chest computed tomography of the patient demonstrating multiple cysts diffusely scattered throughout the lung parenchyma, with irregular walls and variable dimensions (bizarre cysts) in association with diffuse micronodules, a typical pattern of pulmonary involvement by Langerhans cell histiocytosis.
Langerhans cell histiocytosis is a rare disease (incidence of 2-5 cases per million)(1) characterized by proliferation of Langerhans cells(2), most commonly affecting male children in the age range between one and three years(1).
The etiology of this disease still remains unknown. It is believed that the disease is consequence of an immunological deregulation resulting in excessive production of cytokines and prostaglandins, which cause injury to several organs(1).
The disease may affect either single or multiple organs. The clinical presentation depends on the dysfunction degree and on the involved organs(1) and the main complications include hypophyseal dysfunction, particularly diabetes insipidus(3), and neurodegenerative diseases(4).
The most common ophthalmological manifestation is the presence of a solitary bone lesion in the orbit(5), which, likewise the presence of lesions in the mastoid and temporal bones(6), is considered as a risk factor for the onset of complications in the central nervous system (CNS)(7).
Langerhans cell histiocytosis, particularly in its disseminated presentation, may be associated with other conditions such as leukemia, Hodgkin's and non Hodgkin's lymphoma, history of neonatal infection, exposure to solvents, thyroid diseases, infectious diseases (adenovirus, parvovirus, Epstein-Barr virus, cytomegalovirus, HIV and HTLV) and smoking(1), like it may have occurred in the present case.
The imaging method of choice to assess the CNS is magnetic resonance imaging for its highest sensitivity in the detection of lesions notwithstanding the lack of a characteristic radiological pattern of the disease(3).
The diagnosis of Langerhans cell histiocytosis can be made either by means of histological analysis of the lesions (presumed diagnosis) or by immuno-histochemical analysis. At optical microscopy, monoclonal neoplastic infiltrate of Langerhans cells is observed with a lobulated nucleus of thin chromatin and moderately abundant eosinophilic cytoplasm with some nuclear atypias and variable mytotic activity(3). On the other hand, immuno-histochemical study reveals the presence of Birbeck granules, positivity for S-100 and CD1a (representing diagnostic certainty)(1), as in the present case.
Local intervention is the treatment for Langerhans cell histiocytosis(6) in cases of a single lesion. Systemic treatment is reserved for cases of incomplete response to treatment, lesion reactivation or onset of other lesions(7), and chemotherapy is the gold standard(2), as observed in the present case.
The prognosis depends of the extent of the disease: patients with focal disease typically have a good prognosis, while patients with disseminated disease and those with involvement of the central nervous system present a worse prognosis(6).
Thus, the authors conclude that Langerhans cell histiocytosis is a rare and severe disease which may affect several organs. Therefore, such disease must be included in the list of differential diagnosis for patients with proptosis, since orbital involvement indicates a probable CNS compromise, i.e. worse prognosis. The authors consider the present case as being relevant, since it illustrates well the unfavorable natural progression of the disease, even with appropriate treatment, thus serving to emphasize the importance of an early diagnosis. Additionally, the present case was rare, since the disease onset occurred in an elderly patient, while the onset in the childhood is most frequent. Also, it should be observed that involvement of the orbit, like in the present case, is seldom found.
REFERENCES
1. Duda-Szymańska J, Wierzchniewska-ºawska A. Langerhans cell histiocytosis in a 3-year-old girl: a case report and literature review. Pol J Pathol. 2009;60:134-7.
2. Ng Wing Tin S, Martin-Duverneuil N, Idbaih A, et al. Efficacy of vinblastine in central nervous system Langerhans cell histiocytosis: a nationwide retrospective study. Orphanet J Rare Dis. 2011;6:83.
3. Grois N, Tsunematsu Y, Barkovich AJ, et al. Central nervous system disease in Langerhans cell histiocytosis. Br J Cancer Suppl. 1994;23:S24-S28.
4. Imashuku S. High dose immunoglobulin (IVIG) may reduce the incidence of Langerhans cell histiocytosis (LCH)-associated central nervous system involvement. CNS Neurol Disord Drug Targets. 2009;8:380-6.
5. Margo CE, Goldman DR. Langerhans cell histiocytosis. Surv Ophthalmol. 2008;53:332-58.
6. Allen CE, McClain KL. Langerhans cell histiocytosis: a review of past, current and future therapies. Drugs Today (Barc). 2007;43:627-43.
7. Harris GJ. Langerhans cell histiocytosis of the orbit: a need for interdisciplinary dialogue. Am J Ophthalmol. 2006;141:374-8.
1. Master, MD, Ophthalmologist at Hospital de Clínicas - Universidade Estadual de Campinas (HC-Unicamp), Campinas, SP, Brazil.
2. MD, Resident, Department of Radiology of Faculdade de Ciências Médicas - Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil.
3. PhD, Teacher at Department of Radiology, Faculdade de Ciências Médicas - Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil.
4. PhD, Physician Assistant at Department of Radiology, Faculdade de Ciências Médicas - Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil.
5. PhD, Teacher at Department of Pathological Anatomy, Faculdade de Ciências Médicas - Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil.
6. Private Docent, Teacher at Department of Ophthalmo-Otorhinolaryngology, Faculdade de Ciências Médicas - Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil.
Mailing Address:
Dr. Fabiano Reis
Hospital de Clínicas da Universidade Estadual de Campinas (HC-Unicamp)
Rua Vital Brasil, 251, Cidade Universitária Zeferino Vaz, Caixa Postal 6142
Campinas, SP, Brazil, 13083-888
E-mail: fabianoreis2@ gmail.com
Received March 21, 2012.
Accepted after revision June 15, 2012.
Study developed at Hospital de Clínicas - Universidade Estadual de Campinas (HC-Unicamp), Campinas, SP, Brazil.
 Vol. 45 nº 4 - July / Aug. of 2012
Vol. 45 nº 4 - July / Aug. of 2012