INTRODUCTION
Inflammatory myofibroblastic tumors (IMTs), inflammatory pseudotumors or pseudosarcomatous fibromyxoid tumors are mesenchymal lesions originated from non-neoplastic proliferation of myofibroblastic and inflammatory cells, with uncertain etiology and malignant potential, which affect several anatomical sites, particularly lungs and liver(1). Recent studies suggest the involvement of the chromosome 2p23(2) and co-infection with
Mycobacterium tuberculosis(3) in the IMT's pathogenesis.
The authors report the case of a child admitted to the Hospital Universitário and Hospital das Clínicas da Universidade de São Paulo with diagnosis of IMT of bladder, focusing on radiological findings and the differential diagnosis of the disease.
CASE REPORT
A female, 13-year-old patient presenting abdominal pain for one month, weight loss (6 kg) and macroscopic hematuria. The patient was in good general conditions, with paleness (++/4+), and painful abdomen at palpation. Laboratory tests demonstrated normocytic/normochromic anemia (hemoglobin = 7.8 mg/dl), hematuria and leukocyturia, with negative uroculture. Unaltered leukogram and renal and hepatic function tests.
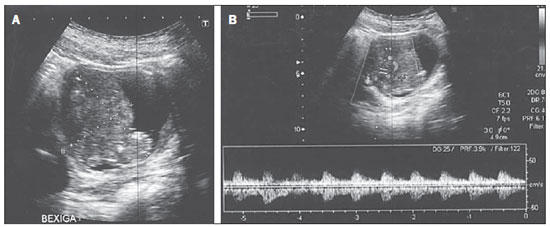
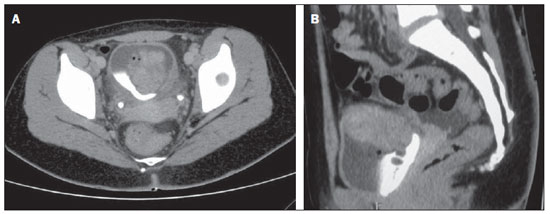
Ultrasonography revealed the presence of a heterogeneous mass measuring 6.0 × 3.0 cm on the vesical wall, with internal vascularization at Doppler (Figure 1). Computed tomography (CT) demonstrated diffuse vesical wall thickening and an expansile, heterogeneous, lobulated lesion measuring 6.0 × 4.1 cm on the upper wall, with blurring of the adjacent fat (Figure 2).
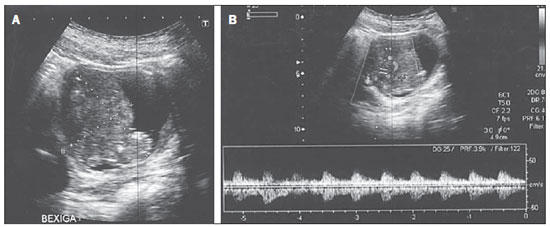
Figure 1. A: Pelvic ultrasonography demonstrating the presence of heterogeneous, lobulated mass on the vesical wall. B: Doppler mapping of a vesical mass, demonstrating arterial flow pattern within the lesion.
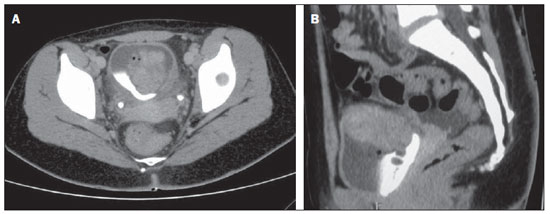
Figure 2. A: Axial computed tomography of pelvis after intravenous contrast injection (excretory phase) showing expansile, heterogeneous, lobulated lesion on the upper vesical wall, with heterogeneous enhancement and blurring of the adjacent fat. B: Sagittal computed tomography of pelvis after intravenous contrast injection (excretory phase) demonstrating diffuse bladder wall thickening and the mentioned expansile lesion.
Freezing biopsy and tumor resection were performed. The surgical specimen measured 10.0 × 7.5 × 4.0 cm, was brownish colored and had a pedicle measuring 2.0 × 1.5 cm. Anatomopathological analysis confirmed IMT with areas of ulceration of the mucosa extending up to the lamina propria and adjacent mucosa, presenting urethelial hyperplasia without atypias.
The postoperative period was uneventful. Two months later, pelvic magnetic resonance imaging demonstrated postoperative fibrotic changes, with no sign of relapse. Follow-up with abdominal ultrasonography did not demonstrate any change.
DISCUSSION
IMTs rarely affect the urinary tract and frequently are associated with trauma, infections or genitourinary tract instrumentation(1). Such tumors are most commonly found in adult individuals and rarely in children. A recent meta-analysis has identified only 35 cases describing IMT of bladder in this age range(4).
IMTs of bladder may be locally aggressive, mimicking malignant neoplasms at cytoscopy and imaging studies, the latter being its main differential diagnosis. Although any vesical site can be affected, there is a subtle predilection for the upper vesical wall(5). Essential criteria for the anatomopathological diagnosis include proliferation of fusiform myoepithelial cells and lymphocytic infiltrate(2). Immunohistochemical analysis may reveal positivity for cytokeratin, vimentin and anaplastic lymphoma kinase (ALK)(2).
At imaging evaluation, both cystic and solid variants have already been reported, although generally a single exophytic or polypoid mass is observed, almost always sparing the vesical trigone(6). At CT and ultrasonography, many lesions are ill-defined and invade circumjacent tissues, with internal vascularization identified at color Doppler(6). Large-sized lesions may present an extravesical component with difficult differentiation from malignant tumors. Generally, the lesion comprises necrotic tissue in the central region and fusiform cells in an edematous stroma with peripheral vessels and inflammatory cells, which explains the ring-shaped contrast-enhancement at CT. At MRI, T2-weighted images show hyperintense central area, with peripheral low signal intensity, while bladder carcinomas generally present hyperintense signal. After contrast agent injection, the signal intensity increases significantly in the periphery while in the central region little increase is observed(6).
The treatment consists of surgical resection, corticotherapy, radiotherapy or conservative treatment. Relapse after resection is generally rare.
Given the considerable overlap of imaging findings among IMT, rhabdomyosarcoma and leiomyosarcoma, the anatomopathological differentiation is critical in the presence of the above described findings to reduce the number of unnecessary radical surgeries.
REFERENCES
1. Lecuona AT, Van Wyk AC, Smit SG, et al. Inflammatory myofibroblastic tumor of the bladder in a 3-year-old boy. Urology. 2012;79:215-8.
2. Yagnik V, Chadha A, Chaudhari S, et al. Inflammatory myofibroblastic tumor of the urinary bladder. Urol Ann. 2010;2:78-9.
3. Androulaki A, Papathomas TG, Liapis G, et al. Inflammatory pseudotumor associated with Mycobacterium tuberculosis infection. Int J Infect Dis. 2008;12:607-10.
4. Houben CH, Chan A, Lee KH, et al. Inflammatory myofibroblastic tumor of the bladder in children: what can be expected? Pediatr Surg Int. 2007;23:815-9.
5. Kim H, Oh SN, Rha SE, et al. Inflammatory myofibroblastic tumor of the bladder: report of two cases. J Korean Soc Radiol. 2010;63:261-5.
6. Wong-You-Cheong JJ, Woodward PJ, Manning MA, et al. From the archives of the AFIP: Inflammatory and nonneoplastic bladder masses: radiologic-pathologic correlation. Radiographics. 2006;26:1847-68.
1. MD, Resident of Radiology and Imaging Diagnosis, Instituto do Coração (InCor) - Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil.
2. MDs, Physicians Assistants at Imaging Unit of Hospital Universitário - Universidade de São Paulo (HU-USP), São Paulo, SP, Brazil.
3. MD, Resident in Pathology, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil.
4. Full Professor, Department of Radiology, Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil.
5. Private Docent, Professor, Department of Radiology, Faculdade de Medicina da Universidade de São Paulo (FMUSP), Director, Unit of Imaging, Hospital Universitário - Universidade de São Paulo (HU-USP), São Paulo, SP, Brazil.
Mailing Address:
Dr. José de Arimatéia Batista Araújo Filho
Alameda Santos, 2534, ap. 51, Cerqueira César
São Paulo, SP, Brazil, 01418-200
E-mail: ariaraujocg@hotmail.com
Received February 24, 2012.
Accepted after revision May 24, 2012.
Study developed at Hospital Universitário - Universidade de São Paulo (HU-USP) and Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil.
 Vol. 45 nº 4 - July / Aug. of 2012
Vol. 45 nº 4 - July / Aug. of 2012