INTRODUCTION
Renal lymphangiectasia is a rare, benign disorder of the lymphatic system of the kidneys that generally is incidentally found. The authors present a case of bilateral renal lymphangiectasia incidentally found at computed tomography, with a literature review and description of the main imaging findings.
CASE REPORT
A female, 65-year-old patient arrived at the unit of radiology of Hospital das Forças Armadas, Brasília, DF, Brazil, complaining of dyspnea. In her clinical history, there was no report of other symptoms, comorbidities or significant family history. Physical examination was normal.
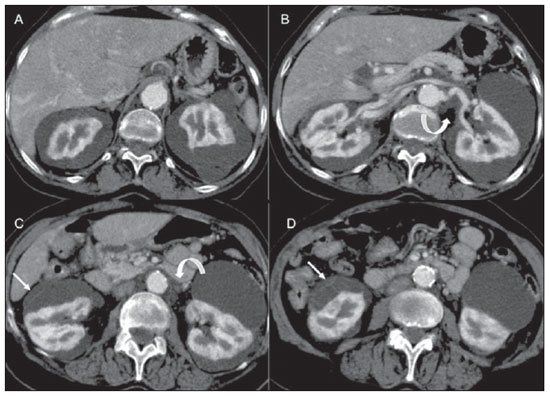
Chest computed tomography was performed and abdominal sections incidentally demonstrated bilateral perinephric and parapyelic cystic lesions with multiloculated appearance and density ranging from 7 to 20 UH (mean = 11 UH) and with no contrast uptake in the corticomedullary and excretory phases. The renal parenchyma was preserved. The parapyelic cysts determined a subtle distortion of the pyelocalyceal system, with no obstructive sign (Figures 1 to 3). Based on the mentioned imaging findings, the diagnosis was characterized as renal lymphangiectasia.
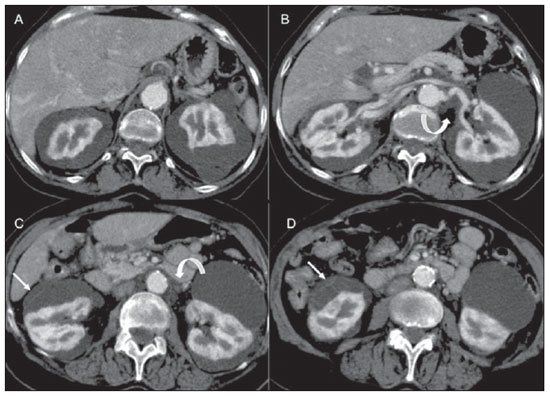
Figure 1. Axial, volumetric images acquired after intravenous iodinated contrast injection, demonstrating voluminous perinephric images, with fine internal septations (straight arrows on
C and
D) and extension towards the renal hilum and periaortic space (curved arrows on
B and
C).
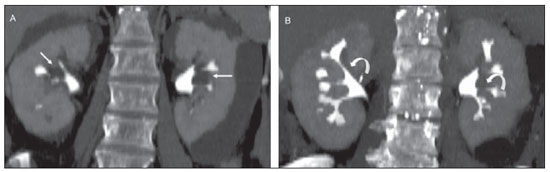
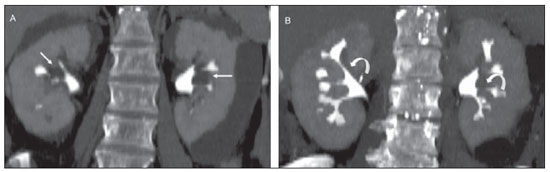
Figure 2. Coronal MIP reformation of sections in excretory phase demonstrating small parapyelic cystic images (straight arrows on
A) determining subtle elongation and deformity of calyceal groups (curved arrows on
B).
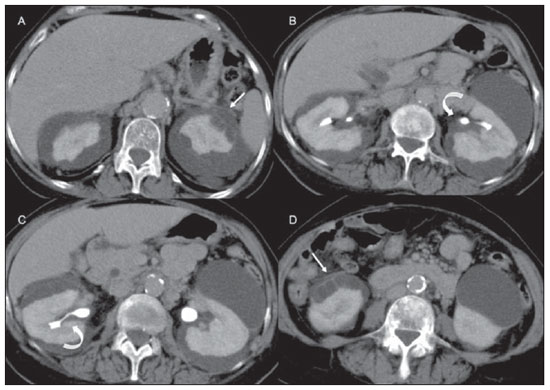
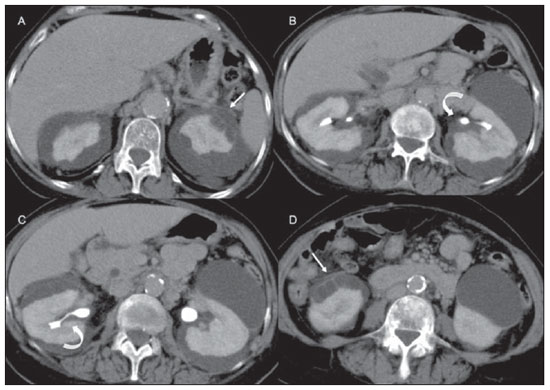
Figure 3. Axial sections in excretory phase demonstrating irregularity of the renal cortical contour bilaterally, in association with several septated perinephric (straight arrows on
A and
D) and parapyelic cystic images with calyceal elongation (curved arrows on
B and
C).
Lymphangiectasia is a rare benign malformation involving the lymphatic system of the kidneys(1).
The origin of such disorder is still controversial, but it is believed that the physiopathogenesis is connected with a failure of the regional lymphatic system in developing communication with the systemic lymphatic tissue(1-3).
This condition is found in both men and women at any age range(2,3). In most cases reported in the literature, the process involves both kidneys, and in general is found incidentally or in patients presenting palpable abdominal masses and/or flank pain(4).
Most of times, the diagnosis may be reliably achieved with just imaging methods, since the findings of this condition are quite characteristic(2,3).
At ultrasonography, such lesions are seen as anechoic septated masses with posterior acoustic shadowing, and possible fine echoes or debris in suspension in cases of hemorrhage(1,3,5). Additionally, hyperechogenicity may be observed on both kidneys, with loss of the corticomedullary differentiation(1,4,6).
Computed tomography identifies unior multiloculated, thin-walled cystic masses filled by material with fluid attenuation, with no contrast enhancement, possibly compressing the cortex, expanding the renal sinus and distorting the calyceal system(1,2,5,6). In the cases of cystic hemorrhage, increased attenuation may be observed. Also, one may visualize renal fasciae thickening(1) and retroperitoneal collections crossing the midline at the level of the renal hilum(1,2).
At magnetic resonance imaging, hypointense lesions are visualized on T1weighted sequences and hyperintense lesions on T2-weighted sequences. In cases of hemorrhage, foci of hyposignal intensity may be seen within the cysts on T1weighted sequences. Also, cortical hypersignal and relative medullary hyposignal on T2-weighted sequences. It is suggested that such pattern of corticomedullary inversion visualized only on T2-weigheted images could be a result of renal edema/congestion secondary to the lymphatic obstruction, also explaining the hyperechogenicity and loss of corticomedullary differentiation at ultrasonography(1,3).
Several hypotheses may be considered in the differential diagnosis. Abscess or urinoma can be differentiated with basis on the clinical history by eventual enhancement or contrast agent extravasation originating from the calyceal system(3,4). Hereditary polycystic renal disease presents multiple cysts predominantly the renal cortex, besides most commonly determining changes in the renal function and involvement of other organs(1,2,4). Lymphomas and other malignancies can be differentiated for affecting the cortical renal parenchyma, by their soft parts attenuation and eventual contrast enhancement(1,2).
Despite the well defined clinical/radiological findings, the natural history of this disease still remains uncertain(2). There are reports of cases where the disease was incidentally diagnosed and did not present loss of renal function over the follow-up period(1,4). However, rare cases have progressed to chronic renal failure. Another relevant situation is the occurrence of lymphangiectasia during gestation, with deterioration of the renal function and arterial hypertension, similarly to signs and symptoms of preeclampsia, with post-delivery reversion.
Other complications described in the literature were superimposed infection, intracystic hemorrhage(4), severe and prolonged arterial hypertension(7), obstructive uropathy(5) and renal vein thrombosis(8).
Since most patients are asymptomatic, no treatment is usually required(1,3). However, considering the possibility of progression to chronic renal failure and complications, clinical and imaging follow-up must be periodically performed(4,5,8). Additionally, female patients in childbearing age should be guided on the risks during gestation(4). For the great majority of asymptomatic patients with large fluid collections, percutaneous drainage may be utilized as a conservative treatment, with surgery remaining reserved for cases of recurrence and complicated or uncontrollable collections(1,3-5).
REFERENCES
1. Rastogi R, Rastogi V. Computed tomographic scan in the diagnosis of bilateral renal lymphangiectasia. Saudi J Kidney Dis Transpl. 2008;19:976–9.
2. Ramseyer LT. Case 34: renal lymphangiectasia. Radiology. 2001;219:442–4.
3. Mani NB, Sodhi KS, Singh P, et al. Renal lymphangiomatosis: a rare cause of bilateral nephromegaly. Australas Radiol. 2003;47:184–7.
4. Özmen M, Deren Ö, Akata D, et al. Renal lymphangiomatosis during pregnancy: management with percutaneous drainage. Eur Radiol. 2001;11:37–40.
5. Chiu JS, Wu CJ, Sun GH, et al. Obstructive uropathy associated with bilateral renal lymphangiomatosis. Nephrol Dial Transplant. 2004;19:2923.
6. Varela JR, Bargiela A, Requejo I, et al. Bilateral renal lymphangiomatosis: US and CT findings. Eur Radiol. 1998;8:230–1.
7. Lindsey JR. Lymphangiectasia simulating polycystic disease. J Urol. 1970;104:658–62.
8. Riehl J, Schmitt H, Schäfer L, et al. Retroperitoneal lymphangiectasia associated with bilateral renal vein thrombosis. Nephrol Dial Transplant. 1997;12:1701–3.
1. MD, Radiologist at Ecocenter - Diagnósticos Médicos por Imagem, Hospital de Base do Distrito Federal (HBDF) and Hospital Universitário de Brasília (HUB), Brasília, DF, Brazil.
2. MD, Resident of Radiology, Hospital de Base do Distrito Federal (HBDF), Brasília, DF, Brazil.
3. MD, Radiologist, Instituto de Radiodiagnóstico Rio Preto - Ultra-X and Hospital de Base de Faculdade de Medicina de São José do Rio Preto (Famerp), São José do Rio Preto, SP, Brazil.
4. MD, Radiologist, Hospital Universitário de Brasília (HUB), Brasília, DF, Brazil.
Mailing Address:
Dr. Rodrigo Abdalla de Vasconcelos
SEPS 709/909 Lote A - Centro Médico Júlio Adnet, Bloco B, sala 406
Brasília, DF, Brazil, 70390-095
E-mail: ecocenterdf@gmail.com
Received September 14, 2011.
Accepted after revision December 2, 2011.
* Study developed at Hospital de Base do Distrito Federal (HBDF), Brasília, DF, Brazil.
 Vol. 45 nº 3 - May / June of 2012
Vol. 45 nº 3 - May / June of 2012