INTRODUCTION
Pelvic lipomatosis is a rare disease that was first described in late 1950's by Engles(1). The condition is characterized by deposition of mature fat tissue in the pelvic cavity and absence of delimitation by a capsule. Intermingled inflammatory reactions may be observed, causing compression of the bladder, rectum and blood vessels. Clinical manifestations include signs and symptoms of extrinsic obstruction of such structures. The exact incidence of this disease is still remains undetermined, but it is known that it is most prevalent in men and individuals with dark-skinned phenotype, most frequently at the third or fourth decade of life, despite the existence of reports describing the disease in the elderly and in children(2,3).
The present report describes a case of pelvic lipomatosis, considering the scarce presence of articles approaching this disease in the scientific literature, and highlighting the imaging findings at excretory urography, computed tomography and magnetic resonance imaging.
CASE REPORT
A 48-year-old male, white patient born in Barro, CE, Brazil, reported low back pain for three years, with progressive worsening in the last two months, particularly on his left side, without irradiation, of compressive nature and in stitches, with mild to moderate intensity and post-micturition relief. Besides the pain, the patient presented dysuria and pollakiuria. No relevant past medical history was reported. At physical examination, atrophic testicle was observed and the prostate was nonpalpable at digital rectal examination. The patient was 1.65 m in height and had 60 kg of weight.
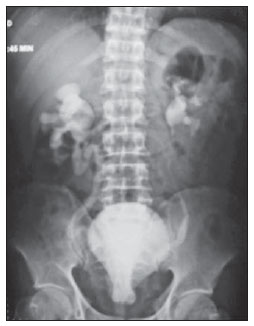
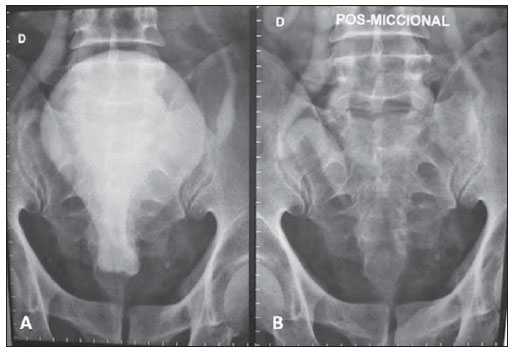
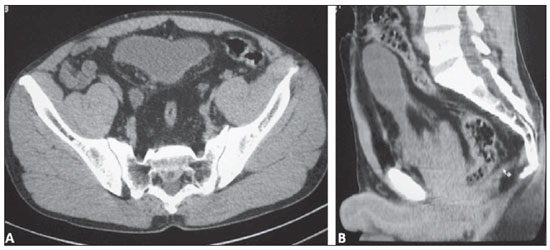
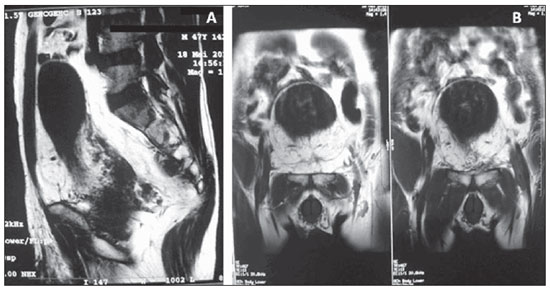
Ultrasonography demonstrated bilateral hydronephrosis, with no other findings. Excretory urography confirmed the presence of hydronephrosis and demonstrated extrinsic compression of the bladder causing deformity and elevation of the bladder floor compatible with the typical presentation of "tear- or pear-shaped bladder" (Figure 1). Post-micturition image did not demonstrate the presence of any urinary residue (Figure 2). Computed tomography demonstrated large amounts of fatty tissue occupying the pelvis from the bottom of the pelvic cavity, causing extrinsic compression and elevation of the bladder with anterocranial deformity, besides occupation of the prostatic compartment. Additionally, signs of extrinsic rectosigmoid compression with widening of the rectosacral space (Figure 3). Magnetic resonance imaging was also performed, demonstrating deformation of the bladder and rectum caused by fatty tissue both in the sagittal and coronal planes (Figure 4).
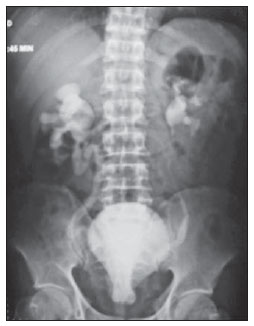
Figure 1. Excretory urography demonstrating the finding of moderate bilateral hydronephrosis and "tear- or pear-shaped bladder".
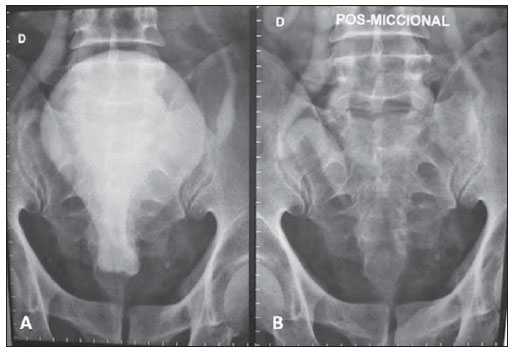
Figure 2. Excretory urography demonstrating a "tear- or pear-shaped bladder" with elevation of its floor, without filling failure (
A) and absence of post-micturition urinary residue (
B).
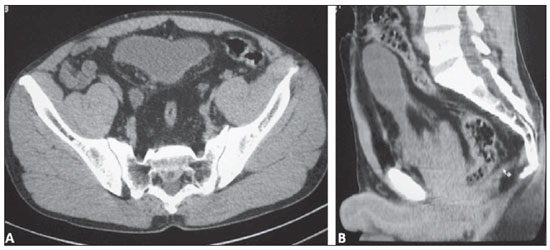
Figure 3. Computed tomography. Axial (A) and sagittal (B) images showing the development of hypodense fat in the pelvis, causing extrinsic compression of the bladder and of the rectum.
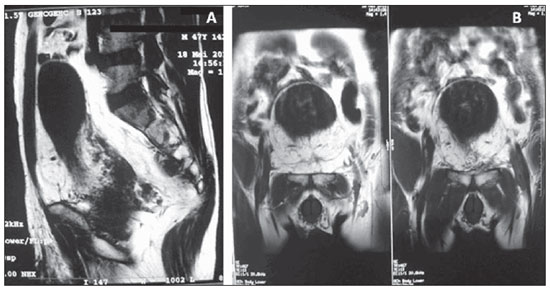
Figure 4. Magnetic resonance imaging, sagittal (A) and coronal (B) T1-weighted sequences. Observe the anatomical deformity caused by the deposition of fatty tissue. Anterocranial deformation of the bladder and enlargement of the presacral space.
Taking the unknown etiology of pelvic lipomatosis into consideration, some authors have proposed some theories in an attempt to explain the development of this disease whose genesis would be associated with a localized manifestation of generalized obesity(4); other authors have raised the hypothesis of a response to repeated urological infections, attributing the origin of the fatty tissue deposition to the inflammatory process. Additionally, other authors suggest that pelvic lipomatosis might represent a variant of Dercum's disease, or other who raise the hypothesis of a localized response to hormonal and metabolic phenomena, as well as those who based on the observation of the highest incidence in black men, suggest the possibility of a genetic basis for the disease(5).
The clinical manifestations result from the extrinsic compression of the structures comprising the urinary system, the lower intestinal tract and the vascular system. Thus, the occurrence of dysuria, pollakiuria, nocturia, hematuria (less frequently), urgency, urinary incontinence and retention, besides repeated urological infections may be observed. Equally, constipation, tenesmus, diarrhea, lower limbs edema and thrombophlebitis, low back pain, suprapubic and perineal pain, painful ejaculation, epidydimitis and orchitis may be observed. Additionally, there is the possibility of renal failure, also with development of arterial hypertension(6).
At physical examination, one may observe pain at abdominal palpation, presence of a palpable mass in the hypogastric region, urinary retention, elevation of the prostate at digital rectal examination, lower limbs edema and arterial hypertension.
The diagnosis is done by means of imaging methods which demonstrate deposition of fatty tissues causing compression of adjacent structures, possibly resulting in relevant morphological deformities. It is important to highlight the relevant role of excretory urography in the demonstration of the typical presentation of tear- or pearshaped bladder, besides uretero-hydronephrosis. Computed tomography defines the cause of the extrinsic compression of the bladder, demonstrating the perivesical and perirectal involvement by fat, thus being sufficient for establishing the diagnosis of pelvic lipomatosis. Magnetic resonance imaging presents the advantage of not utilizing ionizing radiation, constituting a highly accurate method for studying affected anatomic structures, contributing with accurate high-definition images.
Treatment options are limited. Conservative approaches utilizing dietary management, use of antimicrobial agents and corticoids and even attempts with radiotherapy have not demonstrated to be eminently efficacious. Surgery faces difficulties because of the absence of clearly defined dissection planes to allow the release of pelvic organs. Some authors have reported achievement of therapeutic success with lipoaspiration techniques(7). Management of symptoms can be achieved with urinary derivation, but the potential risk for malignization must be taken into consideration e further treatment modalities must be studied.
Additionally to the consequences of the obstructive phenomena, the chronic vesical wall irritation or even the compression of lymph chains caused by the deposition of fat tissue may explain the frequent finding of proliferative processes involving the bladder mucosa in patients affected by this disease, such as cystic and glandular cystitis. In spite of being considered benign lesions, the possibility of development of vesical adenocarcinoma should be considered, justifying the periodic follow-up with cystoscopy and biopsy of suspicious lesions, besides urinary cytology(8).
REFERENCES
1. Engels EP. Sigmoid colon and urinary bladder in high fixation: roentgen changes simulating pelvic tumor. Radiology. 1959;72:419–22.
2. Zaman W, Singh V, Kumar B, et al. Pelvic lipomatosis in a child. Urol Int. 2002;69:238–40.
3. Buitrago Sivianes S, Tallada Buñuel M, Vicente Prados FJ, et al. Pelvic lipomatosis. Diagnostic and therapeutic considerations apropos of 3 cases. Arch Esp Urol. 2002;55:900–6.
4. Sacks SA, Drenick EJ. Pelvic lipomatosis: effect of diet. Urology. 1975;6:609–15.
5. Tong RS, Larner T, Finlay M, et al. Pelvic lipomatosis associated with proliferative cystitis occurring in two brothers. Urology. 2002;59:602.
6. Hudolin T, Kastelan Z, Goluza E, et al. Pelvic and retroperitoneal lipomatosis: case report. Acta Clin Croat. 2010;49:465–8.
7. Halachmi S, Moskovitz B, Calderon N, et al. The use of an ultrasonic assisted lipectomy device for the treatment of obstructive pelvic lipomatosis. Urology. 1996;48:128–30.
8. Heyns CF, De Kock ML, Kirsten PH, et al. Pelvic lipomatosis associated with cystitis glandularis and adenocarcinoma of the bladder. J Urol. 1991;145:364–6.
1. Post-graduation in Radiology, Professor of Human Anatomy and Radiology, Universidade Federal do Ceará (UFC) - Campus Cariri, Barbalha, CE, Brazil.
2. Graduate Students of Medicine, Universidade Federal do Ceará (UFC) - Campus Cariri, Barbalha, CE, Brazil.
3. Graduate Student of Medicine, Faculdade de Medicina Estácio de Juazeiro do Norte, Juazeiro do Norte, CE, Brazil
Mailing Address:
Dr. José Marcílio Nicodemos da Cruz
Avenida Padre Cícero, 2085, Salesiano
Juazeiro do Norte, CE, Brazil, 63010-000
E-mail: nicodemosmarcilio@hotmail.com
Received September 28, 2011.
Accepted after revision March 1st, 2012.
* Study developed at Universidade Federal do Ceará (UFC) - Campus Cariri, Barbalha, CE, Brazil.
 Vol. 45 nº 3 - May / June of 2012
Vol. 45 nº 3 - May / June of 2012