Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 3 - May / June of 2012
Vol. 45 nº 3 - May / June of 2012
|
CASE REPORT
|
|
Lymphoma of uterine cervix: magnetic resonance imaging findings |
|
|
Autho(rs): Daniel Kanaan1; Daniella Braz Parente2; Carolina Pesce Lamas Constantino1; Rodrigo Canellas de Souza1 |
|
|
Keywords: Lymphoma; Uterus. |
|
|
Abstract: INTRODUCTION
Lymphomas represent 3.5% of malignant neoplasms in women. Among such neoplasms, 25% arise in extranodal tissues - 1.0% to 1.5% of them in the female genital tract(1). Uterine lymphoma corresponds to 29% of primary lymphomas of the female genital tract, and lymphomas of uterine cervix are even rarer. The primary involvement of the uterine cervix is also less frequent than involvement of multiple organs. The literature reports cases in women aged between 20 and 80 years, with a peak of incidence at the fifth decade of life(2). The most common symptom if abnormal vaginal bleeding, but other symptoms such as post-coital pain, dyspareunia, pelvic pain, fetid leucorrhea and, most rarely, B symptoms and urinary symptoms have been reported(1). Colpocytopathology presents low diagnostic accuracy and transvaginal ultrasonography (TVUS) for detecting and staging cervical cancer(1-4). The objective of this paper was to present a case of lymphoma of uterine cervix, with emphasis on imaging findings which led to suspicion of the diagnosis, as well as the characteristics that differentiate this disease from epidermoid carcinoma of uterine cervix, that is the main differential diagnosis. CASE REPORT A female 80-year-old patient sought the emergency unit complaining of low back pain with progressive worsening, coursing with nausea, vomiting, headache and appetite loss. At admission, the physical examination was normal. Laboratory tests showed increased levels of urea and creatinine. Gynecological examination and TVUS performed one year ago had not demonstrated any alteration. At admission, ultrasonography (US) showed marked left-sided pyelocalyceal and ureteral dilatation caused by voluminous pelvic expansile mass, without cleavage plane with the uterus. Abdominal and pelvic computed tomography (CT) demonstrated thickening and irregularity of the uterine contour, with densification of the adjacent fat and intermingled lymph nodes, causing left-sided pyelocalyceal system and ureteral dilatation, besides pericardiophrenic in the perivascular retroperitoneum, mesenteric root and external iliac chain. Pelvic magnetic resonance imaging (MRI) demonstrated isointense infiltrative lesion on T1-weighted images (Figure 1), slightly hyperintense on T2-weighted images (Figures 2 and 3) and with diffusion restriction (Figure 4), occupying the whole uterus, with bilateral extension towards the parametrium, attachments and vagina. The lesion also determined ureteral ectasia at left. 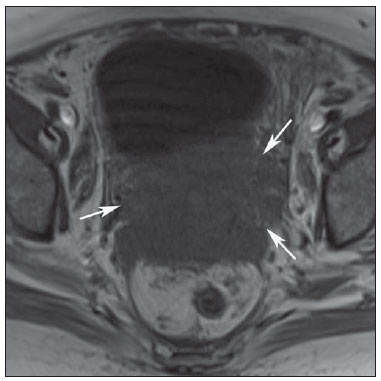 Figure 1. MRI. T1-weighted short-axis image of uterus demonstrates a seemingly infiltrative lesion with isosignal on the uterine cervix, presenting extension towards the adjacent fat tissue (arrows). 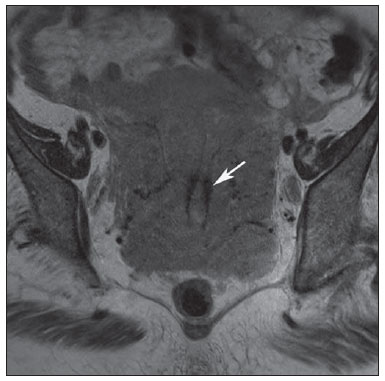 Figure 2. MRI. T2-weighted long-axis image of uterus demonstrates a large uterine lesion with subtle hypersignal intensity, but with preserved zonal anatomy (arrow).  Figure 3. MRI. Sagittal T2-weighted image demonstrates a centered endometrium, with preserved thickness and signal (arrow). 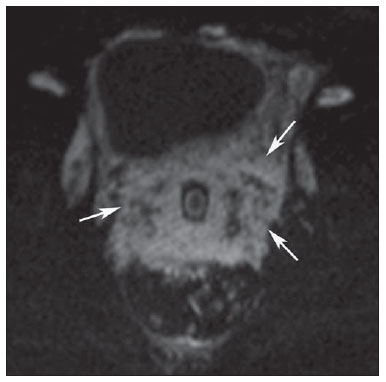 Figure 4. MRI. Diffusion-weighted, short-axis image demonstrates diffusion restriction (arrows), indicating the presence of a lesion with high cellularity. Despite the presence of the large infiltrative lesion compromising the whole uterus, the preserved zonal anatomy of the organ and the diffuse enlargement of the lymph nodes were the focus of attention. Videolaparoscopic-guided biopsy revealed the presence of a diffuse large B-cell lymphoma. Chest CT performed as a part of the disease staging demonstrated infiltration of the mediastinal fat and mediastinal lymph nodes enlargement. According the Ann Arbor classification for extranodal lymphomas, the lesion was staged as IIIA (voluminous pelvic mass). The treatment selected was exclusive chemotherapy according to a schedule of three sessions with cyclophosphamide, vinblastin and prednisone. Neutropenia determined chemotherapy suspension and the patient remained under palliative care until death. DISCUSSION Lymphoma of uterine cervix is rare and, most of times, is related to involvement of multiple organs. The diagnosis is hardly achieved with colpocytopathology and imaging methods. The main differential diagnosis is epidermoid carcinoma of uterine cervix, and the differentiation between both entities is quite difficult. MRI plays a relevant role in the diagnostic suspicion of lymphoma of uterine cervix. The main MRI findings in such cases are increased uterine volume at the expense of a lesion with infiltrative appearance, with intermediate signal intensity on T1- and T2-weighted images, moderate and uniform contrast enhancement and diffusion restriction, presenting preserved junctional and endometrial zones, despite the extensive uterine involvement(5,6). The lesion is homogeneous and presents no or little necrosis(2,5- 7). The definitive diagnosis is achieved by means of lesion biopsy(1-4). The current programs for uterine cervix cancer prevention have sensitively reduced the number of advanced stage cases. Thus, the presence of large uterine cervix masses without necrosis and with preserved zonal anatomy, despite the extensive involvement of the uterine cervix, should point towards less common differential diagnoses such as non-Hodgkin's lymphoma(8). The differential diagnosis of lymphomas of uterine cervix must include benign inflammation, small-cell carcinoma or poorly-differentiated carcinoma and sarcomas(7). In the present case, the disease onset was atypical, with uremic syndrome caused by ureteral obstruction. Initially, there was the suspicion of advanced epidermoid carcinoma of uterine cervix. The finding of a large expansile lesion occupying the whole uterus, with preserved zonal anatomy and endometrium, in association with diffuse lymph nodes enlargement lead to the questioning the initial diagnosis of squamous cell carcinoma, that usually does not preserve the zonal anatomy and the endometrium. Also, the previous gynecological history of normal preventive examination and TVUS did not corroborate the initial hypothesis. In such a circumstance, lymphoma was included among the diagnostic hypotheses. Videolaparoscopicguided biopsy was critical for diagnostic confirmation. The reported case presents most of the imaging findings associated with diffuse nodal involvement described in the literature. Additionally, the clinical progression also was not compatible with squamous cell carcinoma. Vaginal bleeding, abdominal and low back pain are the main symptoms reported in the literature. Initially the patient presented persistent low back pain(3,4). The histological type corresponded to diffuse large B-cell lymphoma that is the most frequent type of lymphoma of uterine cervix (3). Differently from the experience reported in the literature that makes reference to a good prognosis, the patients has not tolerated the chemotherapy scheme and died(3). In summary, in cases where the patient presents a large infiltrative uterine mass with preserved junctional zone and endometrium, without necrosis, one should consider uterine cervix lymphoma as a diagnostic hypothesis whose treatment and prognosis are quite distinct from those for squamous cell carcinoma of uterine cervix. REFERENCES 1. Köhler HF, Novik PR, Campos AH. Lymphoma of the uterine cervix: report of two cases and review of the literature. Rev Bras Ginecol Obstet. 2008;30:626–30. 2. Thyagarajan MS, Dobson MJ, Biswas A. Case report: appearance of uterine cervical lymphoma on MRI: a case report and review of the literature. Br J Radiol. 2004;77:512–5. 3. Sohaib SA, Verma H, Attygalle AD, et al. Imaging of uterine malignancies. Semin Ultrasound CT MR. 2010;31:377–87. 4. Okamoto Y, Tanaka YO, Nishida M, et al. MR imaging of the uterine cervix: imaging-pathologic correlation. Radiographics. 2003;23:425–45. 5. Michniewicz K, Oellinger J. Diagnostic imaging in invasive cervical carcinoma: MRI, CT, and ultrasonography. Zentralbl Gynakol. 2001;123:222–8. 6. Bellin MF, Roy C, Kinkel K, et al. Lymph node metastases: safety and effectiveness of MR imaging with ultrasmall supermagnetic iron oxide particles – initial clinical experience. Radiology. 1998;207:799–808. 7. Dursun P, Gultekin M, Bozdag G, et al. Primary cervical lymphoma: report of two cases and review of the literature. Gynecol Oncol. 2005;98:484–9. 8. Cheong IJ, Kim SH, Park CM. Primary uterine lymphoma: a case report. Korean J Radiol. 2000;1:223–5. 1. MDs, Residents of Radiology, Department of Radiology, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. 2. Fellow PhD degree of Radiology, Universidade Federal do Rio de Janeiro (UFRJ), Researcher, Instituto D'Or de Pesquisa e Ensino, Radiologist at Rede Labs D'Or, Rio de Janeiro, RJ, Brazil. Mailing Address: Dr. Daniel Kanaan Rua Maria Angélica, 643, ap. 201, Jardim Botânico Rio de Janeiro, RJ, Brazil, 22461-151 E-mail: daniel.kanaan@hotmail.com Received September 27, 2011. Accepted after revision November 22, 2011. * Study developed at the Service of Radiology, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554