Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 2 - Mar. / Apr. of 2012
Vol. 45 nº 2 - Mar. / Apr. of 2012
|
CASE REPORT
|
|
Gastric arteriovenous malformation: treatment by embolization |
|
|
Autho(rs): Karenn Barros Bezerra1; Expedito Aguiar Bacelar Júnior2; Nárjara Caroline de Sousa Pereira3; Fábio Alves da Costa3 |
|
|
Keywords: Arteriovenous malformation; Gastrointestinal hemorrhage; Embolization. |
|
|
Abstract: INTRODUCTION
Gastrointestinal bleeding is a common cause of admission to emergency services in hospitals(1). Amongst the main etiologies, esophageal varices, gastric ulcers and gastrointestinal neoplasms are highlighted. Bleedings originated from arteriovenous malformations (AVM) in the stomach have been rarely described in the international literature(2,3). The authors describe the case of a patient admitted with recurrent hematemesis and melena, without elucidation of the diagnosis by upper digestive endoscopy (UDE), whose angiogram detected AVM in the greater curvature of the stomach. The hemorrhage management was performed by means of arterial embolization. CASE REPORT A male, black, 55-year-old patient was admitted to the emergency unit with hematemesis and melena for five hours. The patient reported previous personal history of arterial hypertension under drug therapy and three episodes of mild hematemesis over the last year which were controlled with clinical treatment. No other comorbidity was known. After hemodynamic stabilization, the patient was submitted to UDE which revealed moderate erosive body-fundus gastritis. During the hospital stay, the patient presented new episodes of hematemesis (hemoglobin: 4.3 g/dl; hematocrit: 11.8%), evolving to hypovolemic shock. Repeated UDEs could not identify the origin of the digestive bleeding. Considering the persistence of the hemorrhagic condition (hemoglobin: 6.6 g/dl; hematocrit: 18.5%), the patient was submitted to abdominal CT angiography and celiac trunk angiography which demonstrated the presence of a AVM with plexiform nidus, located on the wall of the greater curvature of the stomach, supplied principally by the short gastric arteries and also by the left gastric artery, with drainage into the splenic vein, where an aneurysm was further demonstrated in the collector vein (Figure 1). 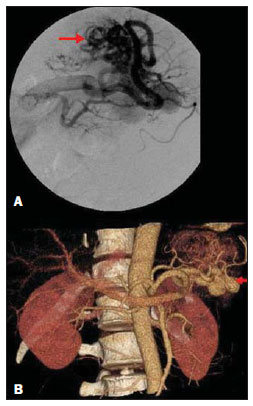 Figure 1. Selective arteriography of splenic artery demonstrating arteriovenous malformation supplied by short gastric arteries (arrow). Early filling of the splenic vein is observed, with venous aneurysms (arrow). Reconstruction volume rendering CT angiography image. After angiography, embolization of the supplying arteries was selected for treatment of the AVM. The procedure was performed by right transfemoral approach, utilizing the Seldinger technique. Initially, a 6F pressure transducer was placed followed by selective catheterization of the celiac trunk and splenic artery with a crossover maneuver utilizing a 260 cm hydrophilic guidewire and a curved 6F Cobra 2 catheter. Subsequently, a superselective characterization of the arterial pedicles of the gastric AVM (short gastric arteries) was performed with a SL 1018 microcatheter aided by a transend 0.014 guidewire. Occlusion of those arterial branches was performed with six GDC microcoils and one Nester microcoil, followed by infusion of N-butyl cyanoacrylate (NBCA) with lipiodol (Figure 2). The day after the procedure, the patient presented a new episode of hematemesis and was submitted to a new UDE which could not identify the origin of the bleeding. Complete embolization of the left gastric artery was chosen for treatment. The procedure was performed with the same previously described technique (Seldinger), utilizing microcoils and NBCA to occlude the arterial vessel (Figures 3 and 4). With no other episode of hematemesis, the patient was discharged. He is currently asymptomatic, presenting normal hematometric levels.  Figure 2. Post-short gastric arteries embolization angiographic follow-up. Angiographic exclusion of the shunt is observed (arrow).  Figure 3. Post-left gastric arteries embolization angiographic follow-up, with angiographic exclusion of the shunt (arrows). 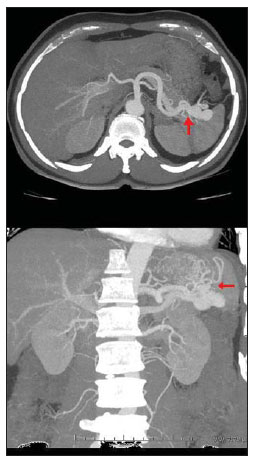 Figure 4. CT angiography with multiplanar reconstruction – axial and coronal sections demonstrating post-treatment management of AVM with embolization (arrows). DISCUSSION Arteriovenous malformation is a congenital lesion where persistent abnormal connection is observed between veins and arteries originating from an embryonic failure in the vascular development of the affected region(4). The authors describe the case of a male, 55-year-old patient with bleeding in the digestive system treated with embolization. The literature reports equal distribution of such malformation between men and women, a mean age of 56 years at the diagnosis, with 75% of patients aged between 50 and 80 years – data compatible with the findings of the present case report(5). Clinically, AVM lesions in the gastrointestinal tract may be either asymptomatic or manifest with hematemesis, melena or iron deficiency anemia. The presence of AVM should be suspected in cases of difficulty in identifying the bleeding origin at UDE(1,6,7). Endoscopy is the method most frequently utilized in the management of these patients, and CT angiography and angiography remaining reserved for cases of difficult diagnostic elucidation. Currently, with the wider availability of these techniques, the diagnosis and treatment of AVMs have become more effective(1). Arteriovenous malformation of the gastrointestinal tract has been determined as the most common cause of chronic and massive hemorrhage in cases where conventional diagnostic tools failed to reveal the cause of the bleeding(8). In the present case, successive UDEs failed to detect the focus of bleeding, likewise in other cases reported in the literature(1,3,8), proving the difficulty in the diagnosis of this condition by means of endoscopy. In the present case, computed tomography angiography and celiac trunk angiography could readily identify AVM in the patient. The differential diagnosis of the arteriographic findings should be made with diseases such as gastric cancer, hemangioma and leiomyosarcoma( 5,9). According to Latar et al., the site of bleeding may be accurately determined by selective angiography with 50%-75% or up to 90% accuracy, provided the procedure is performed while the patient is actively bleeding(5). In the present case, the studies demonstrated that the arterial supply of the AVM was made by the short gastric arteries and by the left gastric artery, with venous drainage into the splenic vein. Previous history of less significant manifestations of hematemesis was reported, hence the inference of the congenital nature of the defect. In the last decades, the treatment by means of embolization has gained widespread acceptance, offering a good chance for controlling the bleeding(2,7,10). An European study has observed that arterial embolization could control upper gastrointestinal bleeding in 88% of patients referred to a center of interventional radiology, and in 77% of such cases, the objective was achieved with a single procedure(10). In the patients with lower gastrointestinal bleeding, the technique was successful in 78% of cases(10). In the present case, the bleeding could not be completely controlled after the first procedure, probably because of the large size of the AVM, which presented more than one feeding source, making the treatment more difficult. With the decision of performing a second intervention with occlusion of the left gastric artery, absolute success was achieved in the hemorrhage management. The technique utilized in the treatment was the same established for controlling digestive bleedings of other etiologies: superselective embolization with occlusion of the arterial branch of the bleeding digestive tract segment with microcoils and NBCA, by means of selective catheterism of celiac trunk or mesenteric artery, depending on the site of the bleeding(11). Intestinal ischemia is the most feared complication of embolization in the gastrointestinal tract. The literature reports rates of such a complication of 14% a 20%(10). The rates of immediate and late postoperative bleeding range from 5% to 37%, hence the relevance of long-term follow-up of these patients. Such a complication may be secondary to incomplete initial resection or metachronous AVM, which have been reported in 11% of cases(8). In the present case, the patient progressed favorably with no complication and total control of the bleeding. Even with the decision to embolize the whole left gastric artery, the stomach vascularization was not affected by the great number of arterial anastomoses in this organ which remained perfused in the postoperative period. Percutaneous embolization represents a less invasive treatment option in cases of gastrointestinal tract hemorrhage which may be utilized in those patients who had not the bleeding controlled by UDE(2,4,12). REFERENCES 1. Elazary R, Verstandig A, Rivkind AI, et al. Gastric arterio-venous malformation emerging from splenic artery. World J Gastroenterol. 2008;14:4091–2. 2. Ibrahim AS, Allangawi MH, al-Muzrakchi AM. Massive bleeding from an arteriovenous malformation in the gastric fundus following gastric biopsy treated by embolisation. Int J Clin Pract. 2003;57:354–5. 3. Khan MI, Baqai MT, Baqai MF, et al. Exsanguinating upper GI bleeds due to unusual arteriovenous malformation (AVM) of stomach and spleen: a case report. World J Emerg Surg. 2009;4:15. 4. Vaccaro P, Zollinger RW 3rd, Sharma H, et al. Massive upper gastrointestinal hemorrhage from an arteriovenous malformation of the stomach. J Clin Gastroenterol. 1985;7:285–8. 5. Latar NH, Phang KS, Yaakub JA, et al. Arteriovenous malformation of the stomach: a rare cause of upper gastrointestinal bleeding. Med J Malaysia. 2011;66:142–3. 6. Lewis TD, Laufer I, Goodacre RL. Arteriovenous malformation of the stomach. Radiologic and endoscopic features. Am J Dig Dis. 1978;23:467–71. 7. Cavett CM, Selby JH, Hamilton JL, et al. Arteriovenous malformation in chronic gastrointestinal bleeding. Ann Surg. 1977;185:116–21. 8. Ng SC, Thomas-Gibson S, Harbin LJ, et al. Gastric arteriovenous malformation: a rare cause of upper GI bleed. Gastrointest Endosc. 2009;69: 155–6. 9. Wato M, Inaba T, Ishikawa S, et al. A case of gastric arteriovenous malformation forming faded depression. Nihon Shokakibyo Gakkai Zasshi. 2006;103:438–43. 10. Krämer SC, Görich J, Rilinger N, et al. Embolization for gastrointestinal hemorrhages. Eur Radiol. 2000;10:802–5. 11. Pitta GBB, Silva CRA. Radiologia vascular e intervencionista na urgência. In: Angiologia e cirurgia vascular: guia ilustrado. [acessado em 15 de fevereiro de 2011]. Disponível em: http://www.lava.med.br/livro 12. Charbonnet P, Toman J, Bühler L, et al. Treatment of gastrointestinal hemorrhage. Abdom Imaging. 2005;30:719–26. 1. MD, São Luís, MA, Brazil. 2. MD, Specialist in Therapeutic Neuroradiology, Radiologist, Instituto de Radiologia São Luís, São Luís, MA, Brazil. 3. MDs, Specialists in Radiology, Ragiologists, Instituto de Radiologia São Luís, São Luís, MA, Brazil. Mailing Address: Dra. Karenn Barros Bezerra Rua das Cegonhas, lote 4, quadra 14, Condomínio Portal do Atlântico, casa 16, Bairro Olho D'Água São Luís, MA, Brazil, 65065-100 E-mail: karennbezerra@hotmail.com Received June 17, 2011. Accepted after revision November 4, 2011. Study developed at Instituto de Radiologia São Luís, São Luís, MA, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554