Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 2 - Mar. / Apr. of 2012
Vol. 45 nº 2 - Mar. / Apr. of 2012
|
ORIGINAL ARTICLE
|
|
Extracranial doses in patients submitted to stereotactic radiosurgery for brain tumors |
|
|
Autho(rs): Maria da Salete Fonseca dos Santos Lundgren1; Helen Jamil Khoury2; Sérgio Azevedo3 |
|
|
Keywords: Brain tumor; Radiotherapy; Radiosurgery; Dosimetry. |
|
|
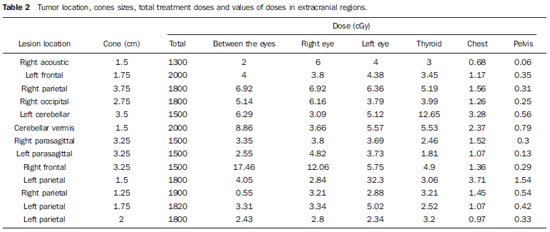
Abstract: INTRODUCTION
Cranial stereotactic radiosurgery consists in administering high doses of ionizing ration into a sterotactically defined intracranial target. Such procedure is utilized in the treatment of small-sized lesions measuring < 4 cm and is performed with Cobalt-60 gamma beams or high-energy Xray beams (linear accelerator (acelerador linear)(1,2). The advantage of this type of procedure is the application of high doses of radiation on the target to br treated with minimal radiation delivered to surrounding structures(3). However, parts of the patient's body located out of the area to be treated may receive secondary radiation because of scattering originating from parts of the apparatus and room walls, radiation leaks through the shielding of the source head, collimators scattering, as well as scattering in the patient(4,5). The estimation of the dose received by the patient in extracranial organs is relevant, particularly for those submitted to radiosurgery and with long life expectancy. Secondary effects resulting from radiation may manifest specially in pediatric patients and patients with benign brain diseases. It is important to highlight that dosimetry in patients submitted to radiosurgery is of paramount relevance, considering the possibility of occurrence of biological effects. The eyes deserve enhanced attention, considering the possibility of crystalline lens opacification, since the threshold for cataract radioinduction is only 0.5 Gy, in acute and fractionated exposures(6–9). The presente study was aimed at estimating the dose received in extracranial regions and organs such as eyes, thyroid, chest and pelvis. MATERIALS AND METHODS The present study evaluated 11 patients submitted to radiosurgery in Instituto de Radioterapia Waldemir Miranda – Centro de Radiocirurgia de Pernambuco, Recife, PE, Brazil, utilizing a Varian Clinac 600C 6 MV linear accelerator, with a Radionics radiosurgery system of circular collimators. The study sample included seven female and four male patients, whose minimum age was 26 years and maximum age was 83 years. The patients were treated for primary brain tumors (seven) and secondary brain tumors (four). Among the patients with secondary tumors, two presented two brain lesions. For estimating the dose in extracranial regions, TLD-100 thermoluminescent dosimeters encapsulated in pairs in numerically identified plastic envelopes. For each patient and for each treated lesion, envelopes with dosimeters were placed on the following regions: between the eyes, on the external corners of both eyes, on the region of the thyroid gland, on the chest (on the lower third of the sternum) and on the pelvis (hypogastric region). After the dosimeters positioning according to the tumor location and size, the treatment was performed with doses ranging from 1300 cGy to 2000 cGy. The cones diameter ranged from 1.50 cm and 3.75 cm. The number of fields (arches) ranged between three and six, and the angulation of the accelerator head, between 45° and 150°. Once the radiosurgery was completed, the TLDs were removed and taken to the Laboratory of Thermoluminescent Dosimetry of the Group of Dosimetry and Nuclear Instrumentation, Department of Nuclear Energy, Universidade Federal de Pernambuco, for reading. As each envelope contained two dosimeters, two reading were obtained for each point. The mean value was determined and a net value was obtained by subtracting the reading of the non-irradiated dosimeter (background reading). The value of the net reading obtained at each point was converted into dose by utilizing the dosimeters calibration curve previously determined with dosimeters irradiation in the linear accelerator, with previously known doses. All the patients were given explanations on the present study and signed a term of free and informed consent. RESULTS Table 1 presents the characteristics of all the patients included in the present study, as well as the tumor sites. Based on such data, one observes that 63.6% of the patients were women and 36.4% were men; and the mean patients' age was 52 years. 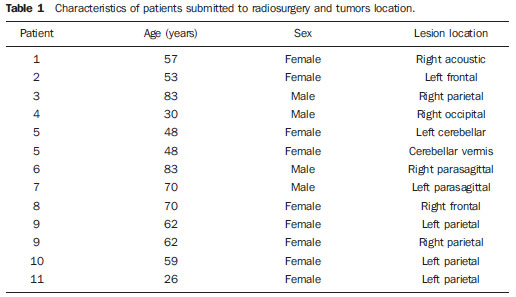 Table 2 shows the location of the tumors, the size of the utilized cone, values of total treatment doeses, as well as values of the doses observed in the evaluated extracranial regions, as follows: between the eyes, external corner of righ eye, external corner of lef eye, thyroid, chest (between the breasts) and pelvis (below the umbilicar scar). The locations of the lesions were the following: right acoustic nerve (1), frontal (2), parietal (5), right occipital (1), cerebellar (2) and parasagittal (2), which are regions whre brain tumors are typically found. Figure 1 shows the distribution of values of radiation doses received in extracranial regions according to the Box & Whiskers chart. In such type of chart, the rectangle extremities represent the first and third quartiles of the data frequency distribution, and the bar crossing the rectangle represents the median. The lower extremity represents the minimum value and the upper, the maximum value. The external circles represent the data set outliers which, generally, are represented on the chart, but are not computed in the calculations of the mean and median. 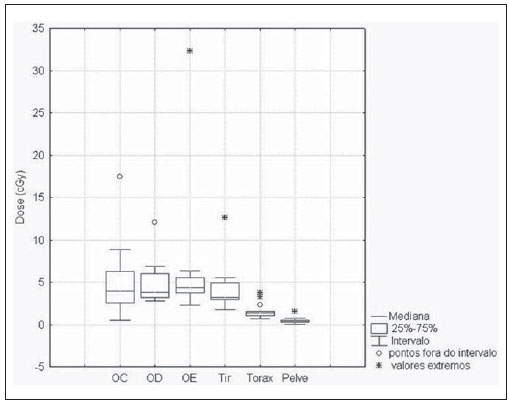 Figure 1. Radiation doses distribution in extracranial regions. (OC, between the eyes; OD, right eye; OE, left eye; Tir, thyroid). Table 3 shows the mean values and standard deviation for doses obtained at the different evaluated extracranial sites. 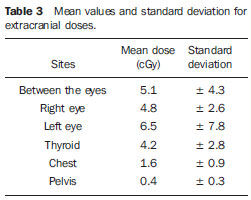 DISCUSSION The mean patients' age is similar to the one observed in the study developed by Yu et al.(5), who have studied the extracranial dose in 104 patients submitted to Gamma Knife radiosurgery. As their results are considered, it is observed that the mean value of radiation doses received by the region between the eyes was 5.1 cGy, with a maximum dose of 17.46 cGy. For the right eye region, the mean dose was 4.8 cGy and the maximum dose, 12.06 cGy. The left eye region received a mean dose of 6.5 cGy and maximum dose of 32.3 cGy. The dose in the eyes, as expected, depends on the position of the organ in relation to the primary radiation beam. The analysis of the data has shown that the mean dose value in the regions of the eyes ipsilateral to the lesion was 5.3 ± 2.4 (cGy) and in the region of the eyes contralateral to the lesion was 3.9 ± 1.1 (cGy). Such results are similar to the ones found by Ma et al.(7), corresponding to a mean dose value in the region of the eyes ipsilateral to the lesion of 7.6 ± 0.6 (cGy), and lower than the values found by these authors for the region of the eyes contralateral to the lesion, corresponding to 6.9 ± 0.6 (cGy). It is important to note that, in the present study, there was one patient who presented a dose in the region of the eye ipsilateral to the lesion corresponding to 32.3 cGy, which was excluded from the above mentioned standard deviation calculations for being much higher than the other values. Such radiation dose, in this case, may be justified by the proximity of the left eye with the treated area, the total radiation dose applied and the utilized arches angulation. The values of doses observed in the present study are similar to data in the literature and are below the threshold for occurence of opacity in the human crystalline lens, which ranges between 0.5 and 2.0 Gy, for a single exposure(9). The study developed by Yu et al.(5) presented a mean value of 24 cGy in the lateral region of the eyes for 104 patients submitted to Gamma Knife radiosurgery. A study developed by Novotný Jr et al.(10) also presents mean dose values of 22 cGy in the region of the eyes. In the thyroid, the mean dose value in the present study was 4.2 cGy, with the maximum value of 12.6 cGy. The analysis of data on Table 2 demonstrates that the dose in the thyroid varies as a function of the lesion location. Treatament of tumors in the cerebellar region result in higher doses in the region of the thyroid. Such values are similar to the ones reported by Novotný Jr et al.(10) and Yu et al.(11), and lower than the ones reported by Yu et al. in a study developed in 1997(5). The mean dose value in the region of the chest was 1.65 cGy and the maximum value was 3.71 cGy. For the region of the pelvis, the mean dose value was 0.45 cGy and the maximum value was 1.54 cGy. CONCLUSIONS In the present study, the values of radiation doses observed in extracranail regions are lower than the values reported by studies in the literature approaching treatment with cranial Gamma Knife radiosurgery. The dose values for extracranial regions of the patient reach levels as high as 30 cGy in the region of the eyes, and 12 cGy in the region of the thyroid. The dose in the thyrois varies as a function of the lesion location. Treatment of tumors in the cerebellar region result in higher doses in the thyroid. Suchs results demonstrate that, although the doses in the eyes do not exceed the tolerance threshold for occurence of opacity of the crystalline lens, it is important that radiotherapists take the risks of radiation doses in these regions into consideration during the planning of cranial radiosurgery. REFERENCES 1. Cruz JC, Salvajoli JV, Weltman E, et al. Controle de qualidade em radiocirurgia. Radiol Bras. 1997;30:163–70. 2. Cruz JC, Segreto RA, Segreto HRC. Estudo dosimétrico de campos pequenos de raios X utilizados em radiocirurgia com um acelerador linear de 6 MV. Rev Imagem. 2003;25:257–67. 3. Souza CH, Monti CR. Dosimetria dos cones radiocirúrgicos Radionics de diâmetros de 5 mm a 50 mm para um feixe de 6 MV de um acelerador linear Mevatron MD digital. Radiol Bras. 2001;34:95–100. 4. Kase KR, Svensson GK, Wolbarst AB, et al. Measurements of dose from secondary radiation outside a treatment field. Int J Radiat Oncol Biol Phys. 1983;9:1177–83. 5. Yu C, Luxton G, Apuzzo ML, et al. Extracranial radiation doses in patients undergoing gamma knife radiosurgery. Neurosurgery. 1997;41:553–9. 6. Liang CL, Ho MW, Lu K, et al. An investigation of eye lens dose of stereotactic radiosurgery for trigeminal neuralgia using Leksell Gamma Knife model C. J Neurosurg. 2006;105 Suppl:112–6. 7. Ma L, Chin L, Sarfaraz M, et al. An investigation of eye lens dose for gamma knife treatments of trigeminal neuralgia. J Appl Clin Med Phys. 2000;1:116–9. 8. International Commission on Radiological Protection. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP. 2007;37:1–332. 9. International Commission on Radiological Protection. ICRP ref 4825-3093-1464. Statement on tissue reactions. Approved by the Commission on April 21, 2011. 10. Novotný J Jr, Novotný J, Hobzová L, et al. Transportation dose and doses to extracranial sites during stereotactic radiosurgery with the Leksell Gamma Knife. Stereotact Funct Neurosurg. 1996;66:170–83. 11. Yu C, Joszef G, Apuzzo ML, et al. Fetal radiation doses for model C gamma knife radiosurgery. Neurosurgery. 2003;52:687–93. 1. PhD, MD, Radiotherapist at Instituto de Radioterapia Waldemir Miranda, Head of the Unit of Radiotherapy, Hospital Universitário Oswaldo Cruz, Recife, PE, Brazil. 2. PhD, Full Professor, Department of Nuclear Energy, Universidade Federal de Pernambuco (UFPE), Recife, PE, Brazil. 3. Medical Physicist, Instituto de Radioterapia Waldemir Miranda, Recife, PE, Brazil. Mailing Address: Dra. Maria da Salete Fonseca dos Santos Lundgren Instituto de Radioterapia Waldemir Miranda Rua Pacífico dos Santos, 60, Derby Recife, PE, Brazil, 52010-030 E -mail: salete@lundgren.med.br Received June 7, 2011. Accepted after revision February 10, 2012. Study developed at Instituto de Radioterapia Waldemir Miranda, Recife, PE, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554