Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 1 - Jan. /Feb. of 2012
Vol. 45 nº 1 - Jan. /Feb. of 2012
|
CASE REPORT
|
|
Arterial embolization in the treatment of hemobilia after hepatic trauma: a case report |
|
|
Autho(rs): Hercilia Maria Carvalho Queiroz1; Francisco de Assis Costa2; Manoel Messias de Campos Junior3; Ricardo Leite de Aquino4; Frederico Augusto de Carvalho Linhares Filho5; Marcelo Otoch6 |
|
|
Keywords: Penetrating hepatic trauma; Hemobilia; Angiography. |
|
|
Abstract: INTRODUCTION
The term hemobilia was first utilized by Sandblom in 1948 to describe bleeding into the biliary tree after liver trauma. It is an uncommon condition and should be considered in the differential diagnosis of upper gastrointestinal bleeding(1). It is caused by a communication between the splanchnic circulation and the biliary tract(2). There are several causes for hemobilia, such as iatrogenic and accidental traumas, biliary lithiasis, inflammation, vascular malformations and tumors. Iatrogenic trauma is the most common cause of hemobilia(3). The clinical presentation is characterized by abdominal pain, digestive hemorrhage and jaundice. Traditionally, the treatment for symptomatic hemobilia used to be surgical, by means of partial hepatectomy or hepatic artery ligation. However, hepatic artery embolization is currently the gold standard, because of 80% to 100% success rate in the management of bleeding associated with low morbidity and mortality indices(3). CASE REPORT Male, 22-year-old patient, victim of firearm injury in the right thoracic-abdominal region for three months ago, when he was submitted to exploratory laparotomy and hepatorrhaphy for injuries in the segments V and VI. Two months after the trauma, the patient presented intense abdominal pain in the right hypochondrium associated with hematemesis, melena and fluctuating jaundice. Abdominal ultrasonography (US) was performed, demonstrating a dilated structure in segments V and VI of the liver, with 2 cm in diameter, with presence of flow at Doppler (Figure 1). Upper gastrointestinal endoscopy (UGIE) did not demonstrate any alteration. Abdominal multislice computed tomography (CT) revealed a hypodense amorphous band-shaped area, located in the right hepatic lobe, involving the segment V and the transition VI/VII, extending over the capsular surface, with subtle dilation of the intra- and extrahepatic bile ducts. The patient was submitted to hepatic arteriography and selective catheterization that demonstrated hepatic artery pseudoaneurysm with arteriobiliary fistula (Figure 2). Embolization was successfully performed with four GDC microcoils with detachment control system (Figure 3). The patient progressed with no symptoms and was discharged seven days after the procedure. 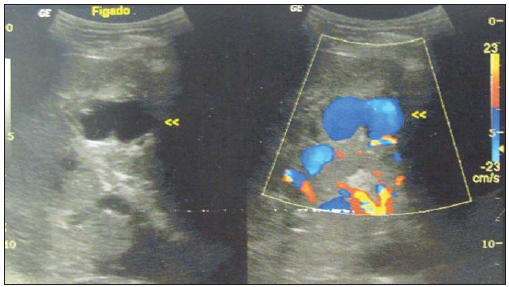 Figure 1. Doppler ultrasonography demonstrating a dilated and tortuous structure with 2 cm in diameter, and presence of flow in the liver segments V and VI. 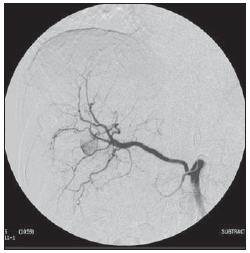 Figure 2. Right hepatic artery arteriography identifying pseudoaneurysm. 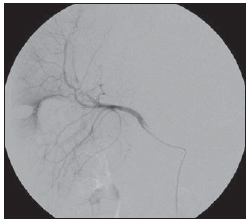 Figure 3. Selective arteriography after embolization with microcoils in the right hepatic artery. DISCUSSION Hemobilia occurs in 2.5% of accidental hepatic traumas and in 3% to 7% of incidental hepatic traumas, and its onset may be observed several months after the trauma(4,5). The clinical presentation of this condition is characterized by jaundice (60%), right hypochondrium pain (70%) and digestive hemorrhage whose results may range from secondary anemia to chronic bleeding or massive bleeding with hypotension(6). The diagnostic investigation of patients with hemobilia should include UGIE to rule out other most common causes of upper digestive hemorrhage, but the intermittent nature of bleeding in cases of hemobilia makes such finding uncertain. Ultrasonography is a rapid, useful, noninvasive and effective method to detect hemobilia, and can demonstrate the presence of blood clots or echogenic intraluminal material in the biliary tree or gallbladder(6,7). Computed tomography can detect common bile duct obstruction, pseudoaneurysms as well as identify intrahepatic cavities that may require surgical debridement(6,7). Hepatic angiography is the diagnostic procedure of choice(6,7). The treatment of post-traumatic hemobilia varies, depending on the bleeding severity, baseline disease, the patient's age and general conditions(6). Bleedings can be controlled in approximately half of cases with only supportive treatment(4). In cases of minimal blood loss, patients may be observed and monitored by means of laboratory tests (hemoglobin, hematocrit, hepatic enzymes and bilirubin dosage). In major bleedings, it is necessary to perform angiography with selective catheterization and embolization of the bleeding vessels. Most frequently, the underlying cause for post-traumatic hemobilia is a pseudoaneurysm(5). The definitive treatment may include liver resection, ligation of the bleeding vessels or hepatic artery embolization(5,6,8). Currently, selective arterial embolization constitutes the treatment of choice with a cure rate above 90%, and is associated with lower morbidity and mortality as compared with surgical treatment that should be reserved for those cases where embolization fails to succeed(5,6,8). Nowadays, there is a wide availability of embolic agents such as detachable balloons, coils, polyvinyl alcohol particles and n-butyl cyanoacrylate(3). Gelfoam is a non-expensive, easily available and absorbable gelatin powder. Coils allow a greater accuracy, but they make the procedure more expensive. Complications from arterial embolization include hepatic infarction, gallbladder necrosis, gastrointestinal bleeding, acute pancreatitis, and are related to the incorrect selection of embolic agents and inappropriate utilization of the superselective embolization technique(3). In conclusion, massive hemobilia is a surgical emergency. Arteriography with transcatheter embolization is one of the best available options for diagnosis and treatment. It is a safe, less invasive and effective method(3). REFERENCES 1. Cho CJ, Kim YG, Lee SG, et al. Inflammatory and noninflammatory vascular disease causing hemobilia. J Clin Rheumatol. 2011;17:138—41. 2. Demyttenaere SV, Hassanain M, Halwani Y, et al. Massive hemobilia. Can J Surg. 2009;52:E109—E110. 3. Xu ZB, Zhou XY, Peng ZY, et al. Evaluation of selective hepatic angiography and embolization in patients with massive hemobilia. Hepatobiliary Pancreat Dis Int. 2005;4:254—8. 4. Dobbins JM, Rao PM, Novelline RA. Posttraumatic hemobilia. Emergency Radiology. 1997;4:180—3. 5. Wani NA, Gojwari TA, Khan NA, et al. Hemobilia in a child due to right hepatic artery pseudoaneurysm: multidetector-row computed tomography demonstration. Saudi J Gastroenterol. 2011;17:152—4. 6. López AC, Villar JM, Álvarez-Arenas IB, et al. Hemobilia: una causa poco frecuente de hemorragia digestiva masiva. Cir Esp. 2007;82:368—72. 7. Forlee MV, Krige JEJ, Welman CJ, et al. Haemobilia after penetrating and blunt liver injury: treatment with selective hepatic artery embolisation. Injury. 2004;35:23—8. 8. Shapira Z, Lavy R, Altshuler A, et al. Hemobilia as a presenting sign of hepatic artery to portal vein fistula caused by percutaneous transhepatic biliary drainage. Isr Med Assoc J. 2011;13:64—5. 1. MD, Resident of Dermatology at Hospital Universitário Walter Cantídio – Universidade Federal do Ceará (UFC), Fortaleza, CE, Brazil. 2. Titular Member of Colégio Brasileiro de Cirurgiões, Surgeon-in-Chief at Serviço de Cirurgia do Hospital Geral de Fortaleza (HGF), Fortaleza, CE, Brazil. 3. General Surgeon, MD, Resident of Vascular Surgery at Hospital Geral de Fortaleza (HGF), Fortaleza, CE, Brazil. 4. Titular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), General Surgeon, Interventional Radiologist and Angioradiology, Hospital Geral de Fortaleza (HGF), Fortaleza, CE, Brazil. 5. General Surgeon, Resident of Vascular Surgery, Instituto Dante Pazzanese de Cardioloigia, São Paulo, SP, Brazil. 6. MD, Interventional Radiologist, Hospital Geral de Fortaleza (HGF), Fortaleza, CE, Brazil. Mailing Address: Dra. Hercilia Maria Carvalho Queiroz Rua Valdetário Mota, 1572, ap. 101, Bairro Cocó Fortaleza, CE, Brazil, 60192-300 E-mail: herciliaqueiroz@hotmail.com Received February 26, 2011. Accepted after revision June 29, 2011. Study developed at Hospital Geral de Fortaleza (HGF), Fortaleza, CE, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554