Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 1 - Jan. /Feb. of 2012
Vol. 45 nº 1 - Jan. /Feb. of 2012
|
CASE REPORT
|
|
Osmotic demyelination syndrome: report of a case with favorable outcome |
|
|
Autho(rs): Mauro Eduardo Jurno1; Marina Horta Azevedo de Castro2; Mariana de Assis Lage2; João Henrique Dupin3; Antonio José Fonseca de Paula4; Gustavo de Vasconcelos Bello5 |
|
|
Keywords: Osmotic demyelination syndrome; Osmotic myelinolysis; Central pontine and extrapontine myelinolysis. |
|
|
Abstract: INTRODUCTION
The present case report refers to a patient with favorable outcome after osmotic demyelination syndrome confirmed by magnetic resonance imaging (MRI). CASE REPORT A female, 60-year-old patient with leukoderma sought medical assistance complaining of heartburn, nausea and vomiting. The patient presented a history of major depressive disorder, undergoing home treatment with risperidone and nortriptyline. According to family members, the news of the patient's daughter pregnancy was the stressful event that triggered to such a condition. Upon admission the use of neuroleptic drugs was discontinued. Laboratory tests demonstrated severe hydroelectrolytic disorder: hyponatremia (sodium: 123 mEq/l; RV: 135 to 145 mEq/l) and hypokalemia (potassium: 2.6 mEq/l; RV: 3.5 to 5.2 mEq/l). Electrolytes replacement was initiated, and sodium concentration in blood was 147 mEq/l in the first 48 hours after admission. Adynamia and prostration were observed. After psychiatric evaluation, clonazepan and mirtazapine were administered, but the clinical picture worsened. The patient presented severe prostration, drowsiness, hyporesponsiveness, eyes opening only upon stimulation, nonspecific motor response (withdrawal reflex) and incomprehensive verbal response (Glasgow coma scale: 9), and then was transferred to the intensive care unit. At admission to such unit, physical evaluation demonstrated isochoric and photoresponsive pupils, absence of nuchal rigidity, right-sided Babinski sign and right upper limb paresis. The patient progressed to a spastic paralysis and mutism. Alterations were not observed at brain computed tomography. As the low level of consciousness of the patient persisted even after normalization of her potassium and sodium levels, MRI was requested, which demonstrated signal hyperintensity on T2-weighted sequences, compromising the pons, sparing the corticospinal tract, with subtle involvement of the basal nuclei and the lateral aspect of the thalami, with bilateral areas of necrosis areas at the globus pallidus (Figures 1, 2 and 3). No abnormal contrast medium uptake was observed, and the radiologist concluded that the images confirmed signs of osmotic demyelination, necrosis in the globus pallidus and signs of decrease in the infra-and supratentorial volumes. 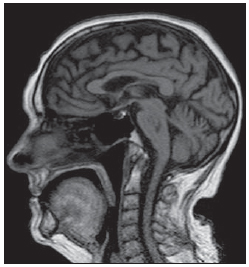 Figure 1. Magnetic resonance imaging, sagittal plane: image of the pontine region. 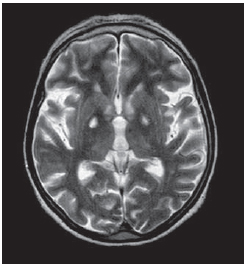 Figure 2. Magnetic resonance imaging, axial plane: extrapontine lesions. 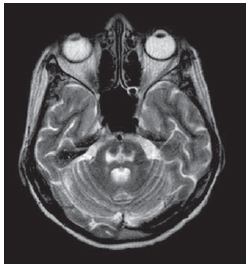 Figure 3. Magnetic resonance imaging, axial plane: pontine lesion image. The patient progressed with improvement in swallowing, allowing the progression from enteral to oral feeding. Improvement was also observed in limb spasticity, with a good response to the administration of introduction of a muscle relaxant drug. After one month, with progressive improvement of the clinical picture, the patient was able to communicate verbally (unable to raise the voice, still presenting dysarthria). MRI was repeated, with the same image pattern demonstrated by the previous study. Within two months, the patient had recovered from the previously described deficits. DISCUSSION Osmotic demyelination syndrome is a demyelinating disorder of the brain primarily affecting the pontine region, sometimes compromising extrapontine regions(1). In spite of the relevance of the association of this syndrome with metabolic disorders, particularly the rapid correction of hyponatremia, this entity may occur in patients with no sign of hydroelectrolyte imbalance(2). In such cases, the patients present other risk factors such as a history of alcohol or drug abuse, malnutrition, hepatic disorders, cancer and Addison's disease(3,4). Generally, mutism and dysarthria are the first symptoms of this syndrome. Alterations such as lethargy and affective disorders are also commonly observed and may be confused with psychiatric disorders. The progression of such patients is variable, ranging from complete recovery to death. In general, recovery is slow and gradual. The mortality rate associated with severe hyponatremia is between 40% and 50%(5,6). In the present case, hyponatremia may have resulted from the utilization of antidepressant drugs or from the previous vomiting episodes. It is important to prevent osmotic demyelination syndrome by means of an appropriate approach for patients with hyponatremia. Some authors consider it impossible to establish a totally risk free level of sodium correction; but in cases of symptomatic hyponatremia, sodium replacement must not exceed 10—12 mEq within 24 hours. The MRI report describes findings compatible with osmotic demyelination syndrome(7,8). REFERENCES 1. Grafton ST, Bahls FH, Bell KR. Acquired focal dystonia following recovery from central pontine myelinolysis. J Neurol Neurosurg Psychiatry. 1988;51:1354—5. 2. Pietrini V, Mozzani F, Crafa P, et al. Central pontine and extrapontine myelinolysis despite careful correction of hyponatremia: clinical and neuropathological findings of a case. Neurol Sci. 2010;31:227—30. 3. Sugimoto T, Murata T, Omori M, et al. Central pontine myelinolysis associated with hypokalaemia in anorexia nervosa. J Neurol Neurosurg Psychiatry. 2003;74:353—5. 4. Martin RJ. Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Neurosurg Psychiatry. 2004;75 Suppl 3:iii22—8. 5. Thompson PD, Miller D, Gledhill RF, et al. Magnetic resonance imaging in central pontine myelinolysis. J Neurol Neurosurg Psychiatry. 1989;52:675—7. 6. Germiniani FMB, Roriz M, Nabhan SK, et al. Mielinólise pontina central e extra-pontina em paciente alcoolista sem distúrbios hidro-eletrolíticos: relato de caso. Arq Neuropsiquiatr. 2002;60:1030—3. 7. Abbott R, Silber E, Felber J, et al. Osmotic demyelination syndrome. BMJ. 2005;331:829—30. 8. Howard SA, Barletta JA, Klufas RA, et al. Best cases from the AFIP: Osmotic demyelination syndrome. Radiographics. 2009;29:933—8. 1. PhD, Coordinator of the Medical Practice Residency Program at Hospital Regional de Barbacena – FHEMIG, Professor at Faculdade de Medicina de Barbacena, Barbacena, MG, Brazil. 2. MDs, Medical Practice Residents, Hospital Regional de Barbacena – FHEMIG, Barbacena, MG, Brazil. 3. MD, Resident of Psychiatry, Centro Hospitalar Psiquiátrico de Barbacena – FHEMIG, Barbacena, MG, Brazil. 4. MD, General Clinician and Oncologist, Preceptor of Medical Practice, Hospital Regional de Barbacena – FHEMIG, Barbacena, MG, Brazil. 5. MD, Radiologist, Titular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), Barbacena, MG, Brazil. Mailing Address: Dr. Mauro Eduardo Jurno Rua Fernando Laguardia, 45, Santa Tereza II (Geraldo Xavier) Barbacena, MG, Brazil, 36201-118 E-mail: jurno@uol.com.br Received January 17, 2011. Accepted after revision July 25, 2011. Study developed at Hospital Regional de Barbacena – FHEMIG, Barbacena, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554