INTRODUCTION
Biloma is defined as a bile collection, either encapsulated or not, outside the biliary tree, with intra- or extrahepatic location, generally of iatrogenic nature or resulting from abdominal trauma(1,2). The word "biloma" was first utilized by Gould & Patel, in 1979(3), but there are descriptions of such an entity since the century XIX(4). Spontaneous rupture of the biliary tree is rarely observed, sometimes being associated with choledocolythiasis(1,5). The detergent activity of bile acids provokes chronic inflammation that, on its turn, causes adhesions, leading to a possible loculated appearance of the collection(2). Clinically, abdominal pain, distention, peritonitis, jaundice and, in more severe cases, sepsis, may occur(1,2,5,6). The mean time between symptoms onset and the diagnosis is one to two weeks(2). Considering the rarity of such condition, the authors describe the present case and review this clinical entity.
CASE REPORT
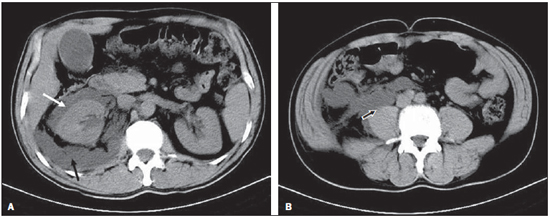
A male, 55-year-old, previously healthy patient has presented right hypochondrium pain, besides acholia and biliuria for 15 days. At clinical examination, the patient was icteric (3+/4+) and afebrile. Laboratory tests included: gamma-GT: 323 U/L, direct bilirubin levels: 7.08 mg/dl, and lipase levels: 195 U/L. Microbiological study presented negative results. Ultrasonography (US) demonstrated biliary dilation, choledocolythiasis and a right renal collection, which US-guided lumbar puncture revealed the presence of a thick, greenish material suggestive of bile. Computed tomography (CT) confirmed thickening of bile duct walls, biliary dilation and perirenal and retroperitoneal collections at right (Figure 1A). The patient was submitted to laparotomy, which confirmed the tomographic description of retroperitoneal collection with bile, dissecting from the posterior plane of the mesocolon to the pelvis (Figure 1B). Intraoperative cholangiography detected the presence of calculi, but did not demonstrate any fistula. After removal of calculi and biloma drainage, the patient progressed well and was discharged in 18 days.
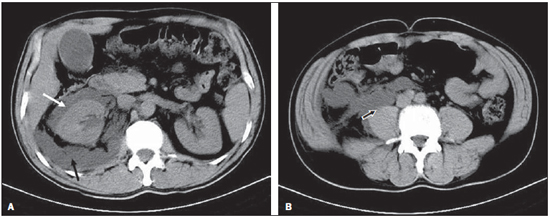
Figure 1. A: Computed tomography demonstrating the presence of isodense biliary dilation and collections in the perirenal (white arrow) and retroperitoneal (black arrow) spaces, both at right. B: Computed tomography demonstrating dissection of the retroperitoneal space, highlighting the pelvic extension in contact with the psoas muscle (arrow) at right.
Description and case reports about bilomas are not frequently found in the medical literature. In most of cases, bilomas involve the development of a bile collection outside the biliary tree after surgery complications or abdominal trauma(1,6,7). With the advent of the laparoscopic technique, the rate of occurrence of bilomas resulting from iatrogenic perforation increased from 0.1% to 0.3-1.5%(2).
Cases of spontaneous bilomas are even more rarely found. In such rare cases, bilomas are most commonly described either in children, as a result of congenital biliary malformations, or associated with choledocolythiasis in adult individuals(3,7), as described in the present report(7). According to the authors' review, this is the first report of spontaneous biloma in the Brazilian literature. Less common causes for bilomas include hepatic infarction, abscess, neoplasia and extrapulmonary tuberculosis(1,5).
There is no consensus on the mechanisms by which the bile reaches the retroperitoneum(1—4). One hypothesis would be the perforation of the inferior two-thirds of the choledoch (retroperitoneal segment), while another hypothesis would be the result from adhesion of the gallbladder to the posterior parietal peritoneum, with chronic inflammation and subsequent perforation(2,4,5). In the authors' opinion, the present case illustrates the second hypothesis.
Ultrasonography is generally the first imaging method that detects the presence of a biloma. However, CT demonstrates higher accuracy in determining the possible causes as well as the relationship between the collection and the adjacent structures(1,3).
Differential diagnoses include cysts, seromas, pseudocysts, hematomas, lymphoceles and hepatic abscess(1,5,6). In the present case, the presence of icteric syndrome and choledocolythiasis suggested the diagnosis of biloma. Radiologically guided percutaneous puncture, as performed in the present case with US, is useful for both the diagnosis and the treatment of bilomas(1—3,5,6). Biochemical and microbiological studies allow the differentiation among infectious causes of other etiologies(1,5,6).
The conservative treatment of bilomas includes intravenous hydration and antibiotic therapy (particularly in cases of sepsis)(1,2,5). In asymptomatic patients with small bile collections (< 4 cm), only follow-up is proposed, with no intervention(2). However, in most of cases, some therapeutic modality is required. For this purpose, percutaneous drainage has been proposed as a first option(1). If resolution is not achieved, retrograde endoscopic cholangiopancreatography and sphincterectomy may be performed, either with or without stent insertion(1—3,5,6).
REFERENCES
1. Bas G, Okan I, Sahin M, et al. Spontaneous biloma managed with endoscopic retrograde cholangiopancreatography and percutaneous drainage: a case report. J Med Case Reports. 2011;5:3.
2. Kannan U, Parshad R, Regmi SK. An unusual presentation of biloma five years following cholecystectomy: a case report. Cases J. 2009;2:8048.
3. Akhtar MA, Bandyopadhyay D, Montgomery HD, et al. Spontaneous idiopathic subcapsular biloma. J Hepatobiliary Pancreat Surg. 2007;14:579—81.
4. Kaushik R, Attri AK. Choleretroperitoneum — an unusual complication of cholelithiasis. Indian J Surg. 2004;66:358—60.
5. Lee JH, Suh JI. A case of infected biloma due to spontaneous intrahepatic biliary rupture. Korean J Intern Med. 2007;22:220—4.
6. Trivedi PJ, Gupta P, Phillips-Hughes J, et al. Biloma: an unusual complication in a patient with pancreatic cancer. World J Gastroenterol. 2009;15:5218—20.
7. Yaşar NF, Yaşar B, Kebapçi M. Spontaneous common bile duct perforation due to chronic pancreatitis, presenting as a huge cystic retroperitoneal mass: a case report. Cases J. 2009;2:6273.
1. MD, Radiologist, Unit of Radiology, Hospital Universitário de Santa Maria (HUSM), Santa Maria, RS, Brazil.
2. Graduate Students of Medicine, Monitors for the Discipline of Radiology, Universidade Federal de Santa Maria (UFSM), Santa Maria, RS, Brazil.
3. MDs, Residents, Hospital Universitário de Santa Maria (HUSM), Santa Maria, RS, Brazil.
4. MD, Radiologist, Hospital Universitário de Santa Maria (HUSM), Assistant Professor, Universidade Federal de Santa Maria (UFSM), Santa Maria, RS, Brazil.
Mailing Address:
Giordano Rafael Tronco Alves
Rua dos Andradas, 1985, ap. 201, Centro
Santa Maria, RS, Brazil, 97010-033
E-mail: grtalves@gmail.com
Received March 29, 2011.
Accepted after revision August 3, 2011.
Study developed at Hospital Universitário de Santa Maria (HUSM), Santa Maria, RS, Brazil.
 Vol. 45 nº 1 - Jan. /Feb. of 2012
Vol. 45 nº 1 - Jan. /Feb. of 2012