Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 6 - Nov. / Dec. of 2011
Vol. 44 nº 6 - Nov. / Dec. of 2011
|
ORIGINAL ARTICLE
|
|
Indications for breast magnetic resonance imaging in an oncology reference center |
|
|
Autho(rs): Elvira Ferreira Marques1; Maria Luiza Leite de Medeiros2; Juliana Alves de Souza1; Maira Coltrone Mendonça2; Almir Galvão Vieira Bitencourt3; Rubens Chojniak4 |
|
|
Keywords: Magnetic resonance imaging; Breast neoplasms; Early detection of cancer. |
|
|
Abstract: INTRODUCTION
Breast cancer is the leading cause of cancer deaths among women in Brazil(1). However, its prognosis may be considered as good, provided the disease is early diagnosed and treated. Mammography is the primary diagnostic method for evaluating breast cancer, with 60—90% sensitivity. This method is utilized in the screening among women above the age of 40 because of its high sensitivity, low cost and low level of radiation exposure. Programs aimed at early detection of tumors by means of periodic mammographic studies have reduced the breast cancer mortality in 25—32%(2). Ultrasonography (US) has also become a relevant evaluation tool in the management of breast cancer, since it can identify small nodules besides being useful in the elucidation of lesions otherwise inconclusive at mammography. However, the main disadvantage of this method is its significant operator dependence(3). Besides mammography and US, other diagnostic methods have been considered for early diagnosis of breast cancer. Magnetic resonance imaging (MRI) has been the most utilized, allowing the assessment of the lesions vascularization by means of intravenous administration of paramagnetic contrast agents(4). According published studies(5), MRI presents higher sensitivity (94—99%), but a highly variable specificity (37—86%). Such a variation in specificity involves several factors particularly related to the lack standardization in the imaging protocols and appropriate indications for this imaging modality(6,7). Considering that the use of MRI was just recently disseminated (in the 1990's), the method still lacks standardization, and the centers present different indications for patients with a single clinical/radiological profile(6). The main objective of the present study is to evaluate and discuss the indications for breast MRI in an oncology reference center. MATERIALS AND METHODS The present study was approved by the Committee for Ethics in Research of the institution and involved a retrospective analysis of clinical records and imaging reports of women who underwent breast MRI in the period from July 1st, 2008 to July 31, 2009. A standard form was filled in for all the patients included in the study, with demographic and clinical data, besides previous imaging studies results and indication for breast MRI. Previous mammographic results were categorized according to the Breast Imaging Reporting and Data System (BI-RADS&#reg;) lexicon(8). Statistical analyses were performed with the aid of the Statistical Package for Social Sciences, version 17.0 for Windows (SPSS Inc.; Chicago, IL, USA). The descriptive analysis included absolute and relative frequencies. Continuous variables were expressed as mean and standard deviation, assuming a normal distribution. RESULTS A total of 529 breast MRI studies were included in the present study. The mean patients' age was 49 years, ranging between 17 and 86 years. Two hundred and nineteen women (41.4%) had a personal history related to increased risk for breast cancer, including previous breast cancer (n = 125; 23.6%), ovarian cancer (n = 6; 1.2%), breast surgery (n = 201; 38.1 %), pre-malignant findings at percutaneous biopsy (n = 13; 2.5%) and history of thoracic irradiation (n = 30; 5.7%). Family history of breast and/or ovarian cancer was present in 162 patients (30.6%), 110 (20.7%) of them in first-degree relatives. Previous mammograms were available for 415 (78.4%) of the patients. The BI-RADS classification of mammographic findings is summarized on Table 1. 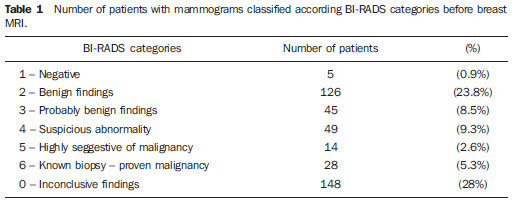 The most common indications for breast MRI were the following: inconclusive mammographic and/or US findings; evaluation of tumor recurrence/fibrotic scar tissue after breast surgery; and staging/surgical planning (Table 2). For 17 patients (3.2%) such information was not available. 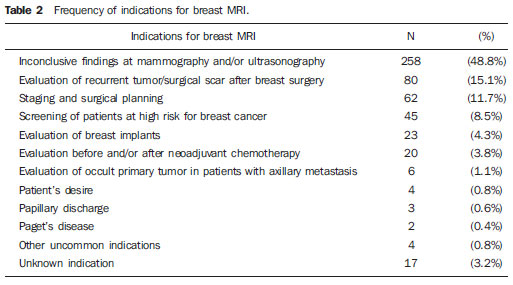 In the group of patients whose indication for breast MRI was based on inconclusive mammographic/US results, the most frequent findings were nodules in 114 out of 258 studies (44%), followed by architectural distortion in 59 (23%) and focal asymmetry also in 59 (23%). DISCUSSION Breast MRI is an expensive method, with potential false positive results and high frequency of incidental findings that may require further investigation. A thorough diagnostic evaluation with mammography and US must be undertaken before considering the necessity of MRI(9). According to the recommendations of the European Society of Breast Cancer Specialists, breast MRI should be performed in radiological centers specialized in conventional breast imaging (mammography and US), percutaneous biopsy and MRI-directed second-look US(10). The most relevant factors in the interpretation of breast MRI studies are correlation with clinical data and conventional imaging results, as well as the presence of precise indications directing the investigation. In a multicentric study developed in the United States of America in 2008 interviewing 754 radiologists specialized in breast imaging, most of them (84%) answered that never (46.5%) or rarely (37.6%) interpret breast MRI studies without correlating their findings with mammographic/US findings. In this same study, the most common indications for breast MRI were aimed at evaluating the disease extent (93.8%) and clarifying inconclusive findings of conventional imaging methods (72.2%)(11). The prevalence of personal and family antecedents related to breast cancer was high, which is expected in patients to be submitted to breast MRI, particularly in an oncology reference center. In the present study, the main indications for MRI are compatible with reports in the literature and international guidelines(6,12). For about half of the patients in the present study, the indication for MRI was aimed at clarifying inconclusive findings of conventional imaging methods, followed by differentiation between tumor recurrence and surgical scar in previously treated patients, staging and preoperative planning in patients with confirmed diagnosis of cancer, besides screening of high-risk patients. However, in spite of being the most common indication, there is no evidence in the literature justifying the utilization of breast MRI as a diagnostic tool in cases of inconclusive findings at conventional imaging studies, particularly those where percutaneous procedures can be performed(10,13). The negative predictive value of MRI is not enough to avoid biopsy for a suspicious clinical or radiological finding without correspondence at MRI(14). A careful selection of patients with inconclusive mammographic findings requiring further evaluation with MRI is important. Moy et al. have evaluated 115 MRI studies performed with such an indication and observed that in 87% of cases, the method did not demonstrate any corresponding abnormality, and in only 0.7% malignant lesions were observed(9). However, in selected cases, MRI may be utilized as a contribution to elucidate inconclusive mammographic/sonographic findings. Such cases include the differential diagnosis of cysts with echogenic contents at US, focal asymmetry or architectural distortion without calcifications at mammography, mammographic findings observed at a single view, multiple nodular lesions of undefined etiology at mammography and US, and suspected tumor recurrence on surgical scar(13). In the literature, breast evaluation in the postoperative period is the most grounded indication for MRI, since surgery and/or radiotherapy may cause skin thickening, edema, development of masses, scars and architectural distortion. Such findings are hardly elucidated by mammography and US, possibly leading to unnecessary procedures. In such cases, the patients may benefit from breast MRI due the typical paramagnetic contrast uptake by the different breast tissues(15). The presence of a non-contrast enhanced scar at MRI has a high negative predictive value for cancer recurrence. However, a normal increase in the vascularization may be observed in the surgical site up to 18 months following radiotherapy(16). Several authors have also described the relevance of breast MRI in the preoperative staging, considering that such method is more sensitive than conventional imaging methods to evaluate the tumor extent, even in cases of ductal carcinoma in situ and invasive lobular carcinoma(15). Additionally, MRI is highly sensitive in the detection of multifocal, multicentric and contralateral tumors(17). MRI can detect additional tumors in the same breast in 15—27% of patients, and in the contralateral breast in 3—10% of patients. The preoperative evaluation by MRI leads to change in the treatment in up to one third of breast cancer patients(18). For breast cancer screening, the American Cancer Society recommends annual MRI in association with mammography for patients with BRCA mutation or with first-degree relatives with such a mutation; patients under the risk = 20—25% of developing breast cancer based on risk evaluation tools; women with history of thoracic irradiation between 10 and 30 years; and patients with genetic disorders leading to increased risk for breast cancer, such as Li-Fraumeni, Cowden or Bannayan-Riley-Ruvulcaba syndromes(19). On the other hand, there is not sufficient evidence to recommend MRI for women under a risk of 15—20% for developing breast cancer during their lifetime; for women with lobular carcinoma in situ or atypical ductal/lobular hyperplasia; for women with heterogeneous or extremely dense breasts at mammography or those with breast cancer antecedents, including ductal carcinoma in situ(19). Other less common indications for breast MRI mentioned in the present study were the following: breast implants evaluation, patients submitted to neoadjuvant chemotherapy, and presence of primary occult tumor in patients with ganglional metastasis. In cases of breast implants evaluation, MRI should be indicated to confirm or rule out implant rupture only in symptomatic patients whose conventional imaging methods could not detect any abnormality(10). Neoadjuvant chemotherapy is routinely utilized in cases of advanced breast cancer to reduce the size of the tumor and, in some cases, to allow treatment with conservative surgery. MRI has demonstrated to be better than clinical examination, mammography and US to evaluate residual disease after neoadjuvant chemotherapy, contributing for a better surgical planning in such cases(20—22). Occult tumors at conventional imaging studies of women with isolated metastasis to axillary lymph nodes represent < 1% of cases of breast carcinoma. MRI can identify the primary tumor in 62—86% of such cases(13). Finally, it is important to be aware of the appropriate indication for breast MRI. Considering that such method presents high sensitivity and high rate of false positive results, it should be recommended only in cases where there is a specific question to be answered, avoiding unnecessary procedures such as biopsies and follow-up studies. If appropriately indicated, breast MRI can significantly contribute in the diagnostic process, constituting an essential tool in the imaging evaluation of the breast. REFERENCES 1. Brasil. Ministério da Saúde. Instituto Nacional de Câncer [Internet]. Estimativa 2010: incidência de câncer no Brasil. Rio de Janeiro, RJ: INCA; 2009. [acessado em 28 de junho de 2010]. Disponível em: http://www.inca.gov.br/estimativa/2010/estimativa20091201.pdf 2. Knutson D, Steiner E. Screening for breast cancer: current recommendations and future directions. Am Fam Physician. 2007;75:1660—6. 3. Yang W, Dempsey PJ. Diagnostic breast ultrasound: current status and future directions. Radiol Clin North Am. 2007;45:845—61. 4. Leopoldino DD, D'Ippolito G, Bezerra ASA, et al. Aspectos técnicos da ressonância magnética de mama com meio de contraste: revisão da literatura. Radiol Bras. 2005;38:287—94. 5. Orel SG, Schnall MD. MR imaging of the breast for the detection, diagnosis, and staging of breast cancer. Radiology. 2001;220:13—30. 6. Rausch DR, Hendrick RE. How to optimize clinical breast MR imaging practices and techniques on your 1.5 T system. Radiographics. 2006;26:1469—84. 7. Kuhl CK. The current status of breast MR imaging. Part 1. Choice of technique, image interpretation, diagnostic accuracy, and transfer to clinical practice. Radiology. 2007;244:356—78. 8. American College of Radiology. Breast Imaging Reporting and Data System: BI-RADS Atlas. 4th ed. Reston, VA: American College of Radiology; 2003. 9. Moy L, Elias K, Patel V, et al. Is breast MRI helpful in the evaluation of inconclusive mammographic findings? AJR Am J Roentgenol. 2009;193:986—93. 10. Sardanelli F, Boetes C, Borisch B, et al. Magnetic resonance imaging of the breast: recommendations from the EUSOMA working group. Eur J Cancer. 2010;46:1296—316. 11. Bassett LW, Dhaliwal SG, Eradat J, et al. National trends and practices in breast MRI. AJR Am J Roentgenol. 2008;191:332—9. 12. American College of Radiology. ACR practice guideline for the performance of magnetic resonance imaging (MRI) of the breast. In: Practice guideline and technical standards, 2005. Reston, VA: American College of Radiology; 2005. p. 341-6. 13. Kuhl CK. Current status of breast MR imaging. Part 2. Clinical applications. Radiology. 2007;244:673—91. 14. DeMartini W, Lehman C. A review of current evidence-based clinical applications for breast magnetic resonance imaging. Top Magn Reson Imaging. 2008;19:143—50. 15. Alvares BR, Michell M. O uso da ressonância magnética na investigação do câncer mamário. Radiol Bras. 2003;36:373—8. 16. Heywang-Köbrunner SH, Schlegel A, Beck R, et al. Contrast-enhanced MRI of the breast after limited surgery and radiation therapy. J Comput Assist Tomogr. 1993;17:891—900. 17. Berg WA, Gutierrez L, NessAiver MS, et al. Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology. 2004;233:830—49. 18. Teller P, Jefford VJ, Gabram SG, et al. The utility of breast MRI in the management of breast cancer. Breast J. 2010;16:394—403. 19. Saslow D, Boetes C, Burke W, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57:75—89. 20. Ojeda-Fournier H, Comstock CE. MRI of breast cancer: current indications. Indian J Radiol Imaging. 2009;19:161—9. 21. Thibault F, Nos C, Meunier M, et al. MRI for surgical planning in patients with breast cancer who undergo preoperative chemotherapy. AJR Am J Roentgenol. 2004;183:1159—68. 22. Partridge SC, Gibbs JE, Lu Y, et al. Accuracy of MR imaging for revealing residual breast cancer in patients who have undergone neoadjuvant chemotherapy. AJR Am J Roentgenol. 2002;179:1193—9. 1. MDs., Imaging Department, Hospital A. C. Camargo, São Paulo, SP, Brazil. 2. Graduate Students of Medicine, Students in the Programa Institucional de Bolsas de Iniciação Científica (PIBIC), Hospital A. C. Camargo, São Paulo, SP, Brazil. 3. MD, Resident at Hospital A. C. Camargo, São Paulo, SP, Brazil. 4. PhD, Titular Director, Imaging Department, Hospital A. C. Camargo, São Paulo, SP, Brazil. Mailing Address: Dr. Almir Galvão Vieira Bitencourt Hospital A. C. Camargo,Departamento de Imagem Rua Professor Antônio Prudente, 211, Liberdade São Paulo, SP, Brazil, 01509-010 E-mail: almirgvb@yahoo.com.br Received August 17, 2011. Accepted after revision October 27, 2011. * Study developed at Hospital A. C. Camargo, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554