INTRODUCTION
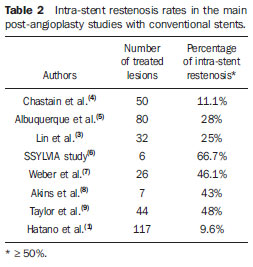
Approximately 25% of ischemic strokes involve the posterior circulation, with vertebral artery stenosis accounting for up to 20% of such events(1,2). In many patients, such ischemia is related to hemodynamic changes caused by proximal obstruction of the vertebral artery. In symptomatic patients unresponsive to dual antiplatelet therapy, balloon angioplasty has been reported as being beneficial. So far, the treatment of vertebral artery stenosis by means of the placement of stents has almost always been performed with conventional coronary prostheses(3,4) and has been associated with restenosis rates ranging from 9.6% to 66.7% (Table 1)(1,3,4—9). The rationale of utilizing drug-eluting stents involves coating the stent (platform) with cytotoxic drugs in order to inhibit the occurrence of vascular restenosis due to intimal hyperplasia. Clinical studies approaching the management of coronary arteries stenosis have demonstrated the superiority of drug-eluting stents over the conventional ones(8,10).

The present study reports the results in the treatment of 14 consecutive patients with vertebrobasilar territory ischemia caused by extracranial vertebral artery stenosis who underwent percutaneous transluminal angioplasty with paclitaxel-eluting stents.
MATERIALS AND METHODS
The present study involved the review of medical records and angiographic studies of 14 patients referred to the interventional neuroradiology team at the Hospital Universitário Clementino Fraga Filho — Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brazil, for treatment of vascular lesions involving vertebral arteries, who were submitted to endovascular treatment with the placement of paclitaxel-eluting stents, in the period from June 2008 to April 2011. The inclusion criteria were the following: a) patients with angiographic evidence of vertebral artery stenosis
> 50%; b) symptoms of vertebrobasilar ischemia refractory to drug therapy, characterized by vascular stroke or transient ischemic attack, during the use of antiplatelet drug and with risk factors under control; c) signing of a term of free and informed consent.
Initially, the patients were selected either by means of computed tomography angiography or magnetic resonance imaging angiography. Once selected, the patient was submitted to digital angiography was performed only at the moment of treatment, for confirmation of the findings and stenosis degree.
The patients included in the present study had symptoms related to posterior circulation ischemia refractory to clinical treatment, including the use of oral antiplatelet drugs. The angiographic images were re-evaluated for quantitative analysis of the lesions, by means of specific software integrated with the angiography system (Quantcor; Siemens Medical Solutions, Forchheim, Germany).
Catheter angiography was performed, including subclavian, vertebral and carotid arteries, also to determine the vascular disease extent and to evaluate the presence of collateral circulation through the posterior communicating arteries. The activated clotting time (ACT) was obtained before initiating the angiographic procedure. After arterial puncture, intravenous heparin bolus of 80 U/kg of body weight was made with the purpose of increasing by two and a half times the basal ACT value, or > 250 seconds. Subsequently, the patients were submitted to the procedure under conscious sedation. The vascular access was obtained by means of puncture of the femoral artery with a 6 or 7 Fr sheath. A guiding catheter Guider Soft Tip 6 or 7 Fr (Boston Scientific; Natick, MA, USA) was then carefully positioned proximally to the lesion to be treated. The lesion was then overcome with a Transend EX 0.014 guide-wire (Boston Scientific; Irvine, CA, USA), sometimes in combination with a 1.7 Fr SL10 microcatheter (Boston Scientific; Irvine, CA, USA). Whenever necessary, a Transend Platinum 300 cm exchange length guidewire (Boston Scientific; Irvine, CA, USA) was utilized for stent insertion. In the cases of severe stenosis (> 80%) balloon angioplasty was utilized for predilation to allow the later stent passage. The therapeutic procedures were performed in all the patients, utilizing Taxus Express Monorail coronary stents (Boston Scientific; Irvine, CA, USA), with paclitaxel-eluting platform. Cerebral protection filter devices were not utilized. An angiographic acquisition was performed following the stent insertion and before its release, in order to determine the exact location of the stent in the lesion. In the cases of ostial lesions, the stent was placed in such a manner so that a short 2 mm segment exceeded the most inferior portion of the ostium in the vertebral artery to completely cover the atherosclerotic plaque. The stent was implanted by slow and controlled inflation of the angioplasty balloon. The administration of heparin was interrupted at the end of the procedure, without reversion. The patients were maintained under oral triclopidine (500 mg/day) or clopidogrel (75 mg/day) regimen for three months, and 200 mg/day aspirin intake for undetermined period of time. Additionally, the risk factors associated with each patient were controlled, with strict management of hypercholesterolemia and hyperglycemia, besides adjuvant treatment for smoking cessation adherent patients. The patients were followed-up with Doppler ultrasonography, digital angiography or computed tomography angiography for up to24 months following the stent implantation.
RESULTS
The present study included 14 patients, 5 of them women and 9 men, with a mean age of 67.2 years (ranging between 49 and 87 years). Among related comorbidities, 8 (57.1%) out the 14 patients had arterial hypertension, 4 (28.6%), hypercholesterolemia, 3 (21.4%), diabetes mellitus, 3 (21.4%), coronary disease, and 4 (28.6%) were smokers. Five out the 14 patients (35.7%) presented with cerebral infarction with acute or subacute progression in the posterior circulation territory, demonstrated either by computed tomography or by magnetic resonance imaging.
Characteristics of the lesions evaluated on angiographic images obtained immediately before the stents implantation demonstrated initial degree of stenosis ranging from 50% to 95% (mean, 78.8%). The length of the stenotic segment ranged from 1.4 to 25.7 mm (mean, 5.2 mm).
The diameter measurements, including at the site of the most severe stenosis, were directly obtained from angiographic images in the pre-angioplasty working position. As regards the lesions distribution in the vertebral artery, most of them (57.14%) were located in the artery ostium, 14.2% in the V2 segment, 7.1% in the V3 segment and 21.4%, in the V4 segment. Ostial atherosclerotic disease, in general, was caused by extension of an atherosclerotic plaque from the subclavian artery. Table 1 demonstrates the arterial stenosis degree before and immediately after the stent implantation, as well as at the 24-month follow-up, besides the stents diameter and length and evaluation of intra-stent restenosis.
The angioplasty and stent implant procedures were technically successful in all the patients. In all of the cases, Taxus Express Monorail paclitaxel eluting stents (Boston Scientific; Irvine, CA, USA) were utilized. Permanent complications related to the procedure were not observed. The residual stenosis degree measured on the angiographic images obtained immediately after the stent implantation ranged from 0% to 20% (mean, 5.7%), and no patient presented residual stenosis > 25% of the arterial lumen. Both the procedure-related permanent neurologic morbidity and mortality in a 30-day follow-up were 0%. Only one patient (7.1%) had a transient ischemic attack within 24 hours after the procedure (patient 11). No stroke related to the site treated during the procedure was observed (0%). In only one case angioplasty-related intimal dissection was observed (patient 4), which was treated by means of an additional stent implantation.
Immediately after the procedure, a neurological evaluation was performed, and then repeated at 15 and 30 days and at the end of the follow-up period (mean 24 months). Most of the patients (71.4%) were symptomatic before the procedure and presented symptom improvement related to the decreased cerebral blood flow. Also, new ischemic episodes were not detected after the procedure.
Long-term angiographic follow-up was performed in all the 14 patients. Before the stent implant, all the patients presented stenosis of at least 50%. Immediately after the procedure, no patient presented residual stenosis
> 50%. Mean residual stenosis immediately after the procedure was 5.7%. At the 24th month, the mean stenosis rate increased to 12.5%, but only one patient presented hemodynamically significant stenosis (> 50%). Such a significant restenosis incidence at the 24th month of follow-up was 7.1%, although such patient did not present recurrence of vertebrobasilar symptoms.
Illustrative cases
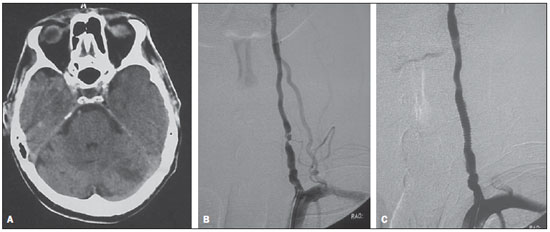
Patient 4 — A 63-year-old man with history of hypertension and hyperlipidemia and episodes of transient ischemic attacks manifested by deficiency in the visual field. The patient was conservatively treated with dual antiplatelet therapy, but two months later developed a stroke affecting the left cerebellar hemisphere and the left occipital lobe, which left the patient with residual quadrantanopia (Figure 1A). The patient was submitted to magnetic resonance angiography that revealed the presence of a lesion in the left vertebral artery. Pre-angioplasty digital angiography demonstrated an eccentric and irregular atheromatous plaque determining about 95% stenosis (Figure 1B). A 6F guide-catheter was inserted into the subclavian artery, and a 3.5 × 16 mm Taxus stent (Boston Scientific, Irvine, CA, USA) was implanted over the lesion. Angiography revealed marked improvement of the flow to the distal vertebral artery and towards the posterior circulation, without residual stenosis (Figure 1C). The patient was discharged, remaining under antiplatelet therapy and asymptomatic along the 26-month neurologic follow-up.
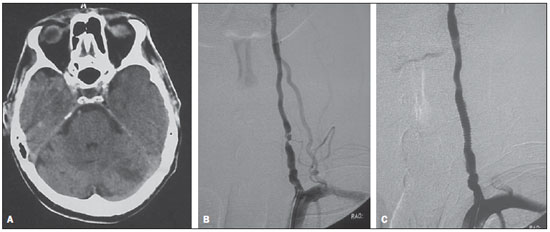
Figure 1. A: Cranial computed tomography demonstrating hypodense lesions in both cerebellar hemispheres, the largest lesion in the left hemisphere. B: Digital angiography of left vertebral artery demonstrating an atherosclerotic lesion at the V2 segment estimated at 95%. C: Post-angioplasty digital angiography of left vertebral artery, without residual stenosis.
A 54-year-old man with coronary artery disease presented to the emergency department hospital with vertiginous syndrome associated with vomiting. Cranial magnetic resonance imaging revealed punctate ischemic lesions in both cerebellar hemispheres, suggesting the embolic origin of the lesions (Figure 2A). Doppler ultrasonography study of the carotid and vertebral arteries suggested the presence of severe stenosis > 90% in the right vertebral artery. Pre-angioplasty digital angiography findings corroborated such diagnosis (Figure 2B), demonstrating an extensive atheromatous lesion determining 90% stenosis in the left vertebral artery ostium. Angioplasty was performed with a 3.0 × 16 mm Taxus stent (Boston Scientific, Irvine, CA, USA) implantation, with excellent angiographic outcome, and without evidence of post-angioplasty residual lesion (Figure 2C). At the 12th month, follow-up with computed tomography angiography demonstrated asymptomatic, minimum intra-stent stenosis, estimated to be 15%.

Figure 2. A: Diffusion-weighted magnetic resonance imaging demonstrating acute ischemic focus in the cerebellum. B: Pre-angioplasty digital angiography revealing lesions at the V1 and V2 segments of the right vertebral artery. C: Digital angiography demonstrating final angiographic appearance after angioplasty.
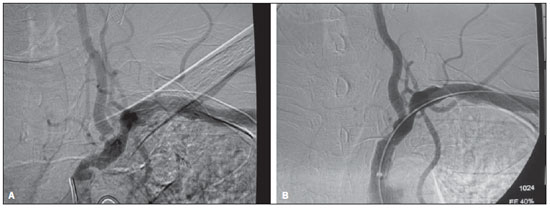
— A 62-year-old man, 50 pack year history of smoking, and history of systemic arterial hypertension, diabetes mellitus and peripheral vascular disease, presented with transient ischemic attacks with manifestation of vertiginous syndrome and diplopia. The patient was submitted to diagnostic digital angiography that demonstrated a lesion affecting 95% of the left vertebral artery ostium associated with 85% stenosis of the subclavian artery proximal to the origin of the vertebral artery (Figure 3A). The left vertebral artery was the dominant artery. Left subclavian artery catheterization was performed and a 4 × 16 mm Taxus stent (Boston Scientific, Irvine, CA, USA) was implanted in the ostium of the left vertebral artery (Figure 3B). Later, balloon angioplasty of the subclavian artery was performed [7 × 20 mm Powerflex balloon (Cordis; Warren, NJ, USA)] (Figure 3C). Post-angioplasty angiography revealed the resolution of the stenosis at the origin of the left subclavian vertebral artery, with excellent anterograde flow in this artery and residual stenosis in the subclavian artery (Figure 3D). The patient presented immediate improvement of symptoms after the procedure and remained asymptomatic over the 18-month follow-up, presenting minimum intra-stent stenosis, estimated to be 10%.
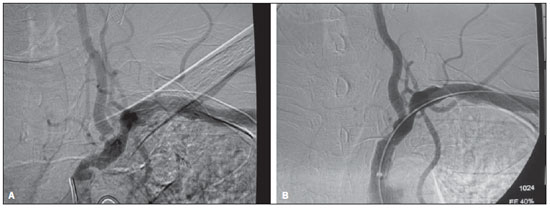
Figure 3. A: Digital angiography of left subclavian artery demonstrating ostial lesion estimated at 95% in the left vertebral artery associated with obstructive lesion of the subclavian artery. B: Final angiographic appearance after angioplasty of the ostium vertebral and subclavian arteries.
The analysis of the present study population identifies hypertension as the most common risk factor for severe atherosclerotic involvement of the vertebrobasilar system, followed by smoking and hypercholesterolemia.
The mechanism of vertebrobasilar ischemia may be embolic or hemodynamic. Embolic causes of vertebrobasilar ischemia are distal embolization of plaques or lesions of the subclavian, vertebral and/or basilar arteries(3,7,11). Hemodynamic symptoms onset depends on the presence of substantial disease in both vertebral arteries; and an incomplete Willis polygon. Although such mechanism is not completely understood, analysis of microemboli present in the posterior circulation demonstrates that the majority of microemboli result from coexistent heart disease, with no correlation with vertebrobasilar system system(2). Additionally, most of the causes related to posterior circulation ischemia are associated with hemodynamic compromise, in contrast with carotid artery disease, where the emboli represent the main source of stroke in the anterior circulation. Alternatively, hemodynamic ischemia with stenosis of the proximal subclavian artery may occur, leading to a subclavian steal syndrome. Some studies question the benefits of endovascular treatment of vertebral artery stenosis as compared with drug therapy(12). In the clinical practice, vascular reconstruction either by surgical or endovascular means has already been considered as a reasonable option to improve blood supply in patients with vertebrobasilar insufficiency. However, currently there is no good reason to refuse the minimally invasive procedure for patients with symptomatic vertebral stenosis refractory to drug treatment.
The present study demonstrates that the use of drug-eluting stents in patients with vertebral artery stenosis is feasible and beneficial to prevent recurrent vertebrobasilar ischemia and vascular restenosis. The assessment of the clinical value of angioplasty with stent placement in the management of vertebral artery stenosis would require a comparison with drug therapy in a larger randomized and controlled study. The current experience with angioplasty and stent placement in the management of vertebral stenosis is almost exclusively based on the utilization of conventional stents(1,3—9) (Table 2). Restenosis of the vessel in which the stent was placed, in the angiographic follow-up is generally defined as the degree of luminal narrowing of at least 50%(13).
A retrospective study developed by Gupta et al.(14) reported the use of drug-eluting stents in the endovascular treatment of 27 vertebral artery lesions. Two types of stents were utilized: Cypher
®(Cordis; Miami, FL, USA) and Taxus Express
®(Boston Scientific; Ca, USA). After four-month follow-up, 7% of the lesions presented restenosis of at least 50%(14). In the present study, the significant restenosis rate was 7.1% at the 24th month of clinical and angiographic follow-up. Apparently, such results were significantly superior to results that would have been obtained in case conventional stents had been utilized.
Undoubtedly, drug-eluting stents are considered as a significant progress for the clinical practice. The drug released by such stents reduces the risk for restenosis, inhibiting macrophage accumulation and proliferation of smooth muscle cells around the stent. However, as such actions also inhibit the reendothelialization on the stent surface(15,16), it was feared that such effects would increase the risk for late thrombosis of the stent, but it seems that the treatment with antiplatelet drug plays a relevant role in the reduction of the risk for such thrombosis(17,18). Additionally, studies on long term clinical outcomes in patients have contributed to confirm the benefits for the survival of drug-eluting coronary stents as compared with conventional stents in up to five years of follow-up, and have not demonstrated any difference in the risk for late thrombosis of the stent(17-20).
It is known that morphological factors related to vertebral artery lesions may affect the result from the therapy with angioplasty and stent placement. For example, the lesion extent affects the restenosis rate(3,21) and excessive vascular tortuosity may hinder the stent implant. In the present study, any lesion length was included and vascular tortuosity was not considered as an exclusion criterion.
The present study presents some limitations, particularly regarding the small number of included patients, but it is sufficient as a feasibility study. A higher rate of late restenosis was observed, particularly in cases where residual stenosis was detected at the end of the procedure. Thus, the presence of residual stenosis immediately after stent implantation in vertebral artery stenosis seems to be a predictor of restenosis at the follow-up, although the relevance of such finding in the clinical outcome is still to be determined.
Even though the dose of the drug released in the circulation is small with no evidences of paclitaxel-induced neurotoxicity, the potential neurotoxicity risk resulting from the implantation of a paclitaxel-eluting stent in a neurovascular territory still remains a concern that must be carefully evaluated(22—24).
Extracranial vertebral artery disease is difficult to diagnose and follow-up by means of non-invasive methods such as Doppler ultrasonography, and its management is not so well defined as the treatment for carotid vascular disease. For initial evaluation, therefore, computed tomography angiography or magnetic resonance imaging was utilized for screening, before the performance of digital angiography, in order to avoid the unnecessary costs and exposure of the patients to angiography risks. However, the use of computed tomography angiography would not be susceptible of resulting in a patient selection bias, as such method tends to exaggerate the degree of vascular stenosis(25). Although the utilization of clopidogrel for a whole year has been recommended for patients with coronary disease following drug-eluting stent implantation, it has been a common practice in the author´s institution to administer aspirin and clopidogrel for six months, and after that, aspirin alone continuously for patients who received stents in the vertebral carotid artery or in intracranial location.
The surgical correction of lesions at the origin of the vertebral artery and subclavian artery by means of ostial vertebral endarterectomy, subclavian endarterectomy, or vertebral artery or carotid artery reimplantation in the subclavian artery is technically difficult. In a series of 325 surgically treated lesions in 290 patients, Thevenet et al.(26) have reported a low mortality rate (0.6%), but a relatively high rate (28%) of post-operative Horner's syndrome, a complication that is not observed in cases of percutaneous therapy. Although good long term outcomes have been reported, they are associated with a relatively high rate of perioperative morbidity(3,26).
CONCLUSIONS
The results of the present retrospective clinical series suggest that angioplasty with placement of paclitaxel-eluting stents in symptomatic patients with vertebral artery stenosis is feasible and promising in terms of safety potential and effectiveness for preventing recurrent ischemia and restenosis. Although a long-term clinical and angiographic follow-up is required to evaluate the durability of the stent permeability, the clinical progression in this group of patients suggests a continuous benefit from the process. A larger randomized and controlled study would be required for such purpose.
REFERENCES
1. Hatano T, Tsukahara T, Miyakoshi A, et al. Stent placement for atherosclerotic stenosis of the vertebral artery ostium: angiographic and clinical outcomes in 117 consecutive patients. Neurosurgery. 2011;68:108—16.
2. Caplan LR, Amarenco P, Rosengart A, et al. Embolism from vertebral artery origin occlusive disease. Neurology. 1992;42:1505—12.
3. Lin YH, Juang JM, Jeng JS, et al. Symptomatic ostial vertebral artery stenosis treated with tubular coronary stents: clinical results and restenosis analysis. J Endovasc Ther. 2004;11:719—26.
4. Chastain HD 2nd, Campbell MS, Iyer S, et al. Extracranial vertebral artery stent placement: in-hospital and follow-up results. J Neurosurg. 1999;91:547—52.
5. Albuquerque FC, Fiorella D, Han P, et al. A reappraisal of angioplasty and stenting for the treatment of vertebral origin stenosis. Neurosurgery. 2003;53:607—16.
6. SSYLVIA Study Investigators. Stenting of Symptomatic Atherosclerotic Lesions in the Vertebral or Intracranial Arteries (SSYLVIA): study results. Stroke. 2004;35:1388—92.
7. Weber W, Mayer TE, Henkes H, et al. Efficacy of stent angioplasty for symptomatic stenoses of the proximal vertebral artery. Eur J Radiol. 2005;56:240—7.
8. Akins PT, Kerber CW, Pakbaz RS. Stenting of vertebral artery origin atherosclerosis in high-risk patients: bare or coated? A single-center consecutive case series. J Invasive Cardiol. 2008;20:14—20.
9. Taylor RA, Siddiq F, Suri MF, et al. Risk factors for in-stent restenosis after vertebral ostium stenting. J Endovasc Ther. 2008;15:203—12.
10. Virmani R, Guagliumi G, Farb A, et al. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation. 2004;109:701—5.
11. Burnay J, Pietri J. Vertebral and subclavian reimplantation into the common carotid artery with widening angioplasty on the vertebral ostium. Presse Med. 1986;15:580.
12. Wehman JC, Hanel RA, Guidot CA, et al. Atherosclerotic occlusive extracranial vertebral artery disease: indications for intervention, endovascular techniques, short-term and long-term results. J Interv Cardiol. 2004;17:219—32.
13. Biria M, Tadros P, Gupta K. Subclavian-vertebral artery bifurcation stenting using drug-eluting stents: a report of two cases using different techniques. J Invasive Cardiol. 2007;19:E156—9.
14. Gupta R, Al-Ali F, Thomas AJ, et al. Safety, feasibility, and short-term follow-up of drug-eluting stent placement in the intracranial and extracranial circulation. Stroke. 2006;37:2562—6.
15. Vajda Z, Miloslavski E, Güthe T, et al. Treatment of stenoses of vertebral artery origin using short drug-eluting coronary stents: improved follow-up results. AJNR Am J Neuroradiol. 2009;30:1653—6.
16. Yu SC, Leung TW, Lam JS, et al. Symptomatic ostial vertebral artery stenosis: treatment with drug-eluting stents–clinical and angiographic results at 1-year follow-up. Radiology. 2009;251:224—32.
17. Regar E, Serruys PW. The Ravel trial. Zero percent restenosis: a cardiologists dream comes true! Rev Esp Cardiol. 2002;55:459—62.
18. Dabus G, Gerstle RJ, Derdeyn CP, et al. Endovascular treatment of the vertebral artery origin in patients with symptoms of vertebrobasilar ischemia. Neuroradiology. 2006;48:917—23.
19. Du B, Wong EH, Jiang WJ. Long-term outcome of tandem stenting for stenoses of the intracranial vertebrobasilar artery and vertebral ostium. AJNR Am J Neuroradiol. 2009;30:840—4.
20. Morice MC, Serruys PW, Barragan P, et al. Long-term clinical outcomes with sirolimus-eluting coronary stents: five-year results of the RAVEL trial. J Am Coll Cardiol. 2007;50:1299—304.
21. Zhou Z, Yin Q, Xu G, et al. Influence of vessel size and tortuosity on in-stent restenosis after stent implantation in the vertebral artery ostium. Cardiovasc Intervent Radiol. 2011;34:481—7.
22. Pace A, Bove L, Aloe A, et al. Paclitaxel neurotoxicity: clinical and neurophysiological study of 23 patients. Ital J Neurol Sci. 1997;18:73—9.
23. Pace A, Nisticò C, Cuppone F, et al. Peripheral neurotoxicity of weekly paclitaxel chemotherapy: a schedule or a dose issue? Clin Breast Cancer. 2007;7:550—4.
24. van Gerven JM, Moll JW, van den Bent MJ, et al. Paclitaxel (Taxol) induces cumulative mild neurotoxicity. Eur J Cancer. 1994;30A:1074—7.
25. Yoo WJ, Lim YS, Ahn KJ, et al. Assessment of vertebral artery stents using 16-slice multi-detector row CT angiography in vivo evaluation: comparison of a medium-smooth kernel and a sharp kernel. Eur J Radiol. 2009;70:362—8.
26. Thevenet A, Ruotolo C. Surgical repair of vertebral artery stenoses. J Cardiovasc Surg (Torino). 1984;25:101—10.
1. Master, MD, Neuroradiologist at Hospital Universitário Clementino Fraga Filho da Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil.
2. Master, MD, Neuroradiologist at Hospital Universitário Antônio Pedro da Universidade Federal Fluminense (UFF), Niterói, RJ, Brazil.
3. PhD, Assistant Professor at Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRPUSP), Ribeirão Preto, SP, Brazil.
Mailing Address:
Dr. Eduardo Wajnberg
Rua Nina Rodrigues, 72/102, Jardim Botânico
Rio de Janeiro, RJ, Brazil, 22461-100
E-mail: eduardowj@gmail.com
Received August 1st, 2011.
Accepted after revision October 10, 2011.
* Study developed at Hospital Universitário Clementino Fraga Filho da Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil.
 Vol. 44 nº 6 - Nov. / Dec. of 2011
Vol. 44 nº 6 - Nov. / Dec. of 2011