Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 4 - July / Aug. of 2011
Vol. 44 nº 4 - July / Aug. of 2011
|
CASE REPORT
|
|
Spinal lipoma associated with congenital dermal sinus: a case report |
|
|
Autho(rs): Lívia Teresa Moreira Rios1; Ricardo Villar Barbosa de Oliveira2; Marília da Glória Martins3; Olga Maria Ribeiro Leitão4; Vanda Maria Ferreira Simões5; Janilson Moucherek Soares do Nascimento6 |
|
|
Keywords: Occult spinal dysraphism; Congenital dermal sinus; Intradural lipoma; Ultrasonography. |
|
|
Abstract: INTRODUCTION
Occult spinal dysraphisms constitute a group of dorsal conditions lying under an intact layer of dermis and epidermis. As the skin and nervous tissue originate from the ectoderm, abnormalities may simultaneously occur in both of them. Thus, association with a cutaneous stigma such as skin covered mass, hair tuft, cutaneous appendix, skin color disorder, cutaneous depression, is frequently observed(1—3). The spectrum of occult dysraphic lesions includes lipomas, dorsal dermal sinuses, myelocystoceles and diastematomyelia. Dorsal dermal sinus is usually associated with 60% of the cases of spinal lipoma(4). Spinal lipomas are less frequently found and may be located either outside or inside the spinal canal, or even in a combination of these locations(1—5). The present report describes a case of lipoma located inside the spinal canal (intradural lipoma), whose suspicion and detection were facilitated by the presence of a cutaneous stigmata of congenital dorsal dermal sinus type. CASE REPORT A male full-term neonate born by cesarean delivery, with antenatal ultrasonography studies with no abnormality. Clinical examination detected cutaneous stigma in the form of a cutaneous depression with a small paramedian ostium covered by a thin transparent membrane with elevated borders, immediately at left from the midline, above the intergluteal fold, compatible with dorsal dermal sinus. Also, a small solid mass covered by skin was observed in the lumbosacral region (Figure 1).  Figure 1. Dorsal dermal sinus. Image of the neonate with cutaneous stigmata (arrow) characterized by cutaneous depression covered by a thin membrane located above the intergluteal fold. Ultrasonography of the lumbosacral spine was requested at the third day of life, upon observation of the cutaneous stigmata indicating the presence of a possible occult spinal dysraphism. The images demonstrated a hypoechoic, elongated, solid mass within the spinal canal, extending from T12 to L4, measuring 3.2 × 0.7 cm, posteriorly located and attached do the spinal bone marrow, displacing it anterolaterally to the right and determining the presence of tethered spinal cord syndrome (Figures 2 and 3), with medullary cone at the level of the third and fourth lumbar vertebrae. 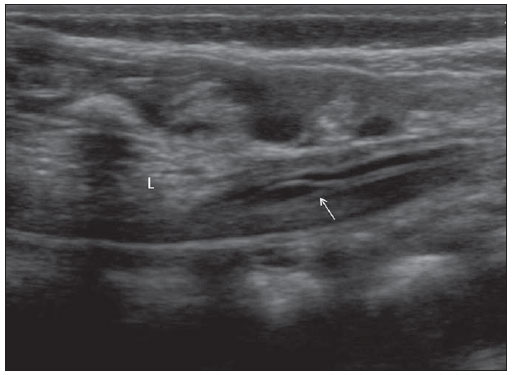 Figure 2. Tethered spinal cord syndrome. Midsagittal section at ultrasonography. The arrow indicates the medullary cone at the sacral level, as a function of the presence of the intradural lipoma (L). 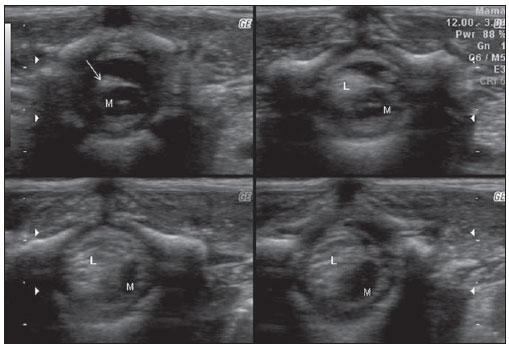 Figure 3. Cross-sectional section at ultrasonography performed with the patient in ventral decubitus, at different levels of the lumbosacral spine, demonstrating a hypoechoic, solid mass (arrow) (L), which fits into the medullary canal, attached to the bone marrow (M), displacing it anterolaterally to the right. Magnetic resonance imaging confirmed the sonographic findings of a mass within the spinal canal, accurately determined the lesion topography and demonstrated the opening of the dorsal dermal sinus, from the spinal canal to the skin surface (Figure 4). 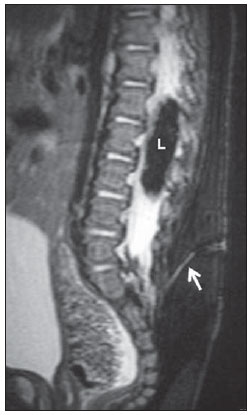 Figure 4. Mid-sagittal magnetic resonance imaging slice, T2-weighted image with fat-saturation, demonstrating intradural lipoma (L). The arrow indicates a dermal sinus connecting the fundus of the dural sac with the skin at S1–S2 plane. At his second month of life, the child was submitted to laminectomy with subtotal tumor resection. He remains under follow-up, with good clinical progression, and a subtle right lower limb motor deficit. DISCUSSION Occult spina bifida is frequently asymptomatic and may clinically manifest at any age. The defect occurs at the first two months of intrauterine life. Embryologically, the neural tube develops from ectodermal cells (neuroectoderm), while the mesoderm will originate the bones, meninges and muscles. The skin is separated from the neural tube by a mesoderm layer. An incomplete separation between the cutaneous ectoderm and the neural tube results in spine tethering, diastematomyelia or in dermal sinus. The premature separation between the cutaneous ectoderm and the underlying neuroectoderm leads to incorporation of mesenchymal elements between the neural tube and the skin, which may result in the development of lipomas(6). Spinal lipomas are divided into three main types as follows: lipomyelomeningocele, intradural lipoma and filum terminale fibrolipoma(1). Besides fat, about 80% of such tumors may contain neural tissue or meninges(5). Congenital dorsal dermal sinus is an epithelial connection between the skin and deepest tissues, resulting from a probable incomplete separation between the cutaneous ectoderm and the underlying neuroectoderm. Its estimated incidence in the general population is 1:2,500 live newborns. At clinical examination, it presents as a cutaneous depression or ostium, and is usually associated with 60% of spinal lipomas. The presence of such a condition should be considered as an alert sign for spinal lipoma screening by means of ultrasonography(5). The sonographic study assumes a relevant role as a screening method in neonates under suspicion of occult dysraphism without the presence of an apparent mass. Most of times, the presence of cutaneous stigmata is the sole indicator of the possible existence of occult spina bifida. Ultrasonography presents a good sensitivity and plays a significant role in the screening for fatty masses, characterization of the medullary cone topography and in the thorough analysis of the relation between the spinal bone marrow and the possible existence of a mass. Ultrasonography of a neonate’s spinal canal plays a relevant role as screening method, but as such, it presents limitations. Most of times, this method cannot identify the communication between the dermal sinus and the dural sac, which is important to rule out the risk for meningeal infection. The method can only infer the possibility of communication. Magnetic resonance imaging is the most specific imaging method to evaluate the spinal canal in neonates, allowing diagnostic confirmation and a more detailed analysis of dysraphism(3,7). REFERENCES 1. Wilson PE, Oleszek JL, Clayton GH. Pediatric spinal cord tumors and masses. J Spinal Cord Med. 2007;30Suppl1:S15-20. 2. Guggisberg D, Hadj-Rabia S, Viney C, et al. Skin markers of occult spinal dysraphism in children: a review of 54 cases. Arch Dermatol. 2004;140:1109-15. 3. Henriques JGB, Pianetti Filho G, Costa PR, et al. Uso da ultra-sonografia na triagem de disrafismos espinhais ocultos. Arq Neuropsiquiatr. 2004;62:701-6. 4. Ackerman LL, Menezes AH. Spinal congenital dermal sinuses: a 30-year experience. Pediatrics. 2003;112(3Pt1);641-7. 5. Lowe LH, Johanek AJ, Moore CW. Sonography of the neonatal spine: part 2, spinal disorders. AJR Am J Roentgenol. 2007;188:739-44. 6. Oskouian RJ Jr, Sansur CA, Shaffrey CI. Congenital abnormalities of the thoracic and lumbar spine. Neurosurg Clin N Am. 2007;18:479-98. 7. Robinson AJ, Russell S, Rimmer S. The value of ultrasonic examination of the lumbar spine in infants with specific reference to cutaneous markers of occult spinal dysraphism. Clin Radiol. 2005;60:72-7. 1. Master, MD, Imaging Clinic Coordinator, Obstetrics and Gynecology Unit of University Hospital in Federal University in Maranhão (HU-UFMA), São Luís, MA, Brazil. 2. Master, MD, Imaging Clinic, Obstetrics and Gynecology Unit of University Hospital in Federal University in Maranhão (HU-UFMA), São Luís, MA, Brazil. 3. PhD, Associate Professor II of Obstetrics, Obstetrics and Gynecology Unit Head, University Hospital in Federal University in Maranhão (HU-UFMA), São Luís, MA, Brazil. 4. MD, General Ultrasonography Specialist, Pediatric Ultrasonography Unit Physician, University Hospital in Federal University in Maranhão (HU-UFMA), São Luís, MA, Brazil. 5. PhD, Medical Residency General Coordinator, Neonatology Unit Head, University Hospital in Federal University in Maranhão (HU-UFMA), São Luís, MA, Brazil. 6. MD, General Ultrasonography Specialist, Imaging Clinic Physician, Obstetrics and Gynecology Unit, University Hospital in Federal University in Maranhão (HU-UFMA), São Luís, MA, Brazil. Mailing Address: Dra. Lívia Teresa Moreira Rios Avenida do Vale, L-10, Q-35, Ed. Costa Rica, ap. 801, Jardim Renascença São Luís, MA, Brazil, 65075-820 E-mail: ltlrios@terra.com.br Received March 24, 2010. Accepted after revision March 31, 2011. Study developed at the Imaging Clinic, Obstetrics and Gynecology Unit of University Hospital in Federal University in Maranhão (HU-UFMA), São Luís, MA, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554