INTRODUCTION
Mounier-Kuhn syndrome or tracheobronchomegaly (TBM) is a rare disease characterized by atrophy or absence of elastic fibers and thinning of the smooth muscles in the trachea, main bronchi and first- to fourth-order bronchi(1); consequently, the flaccid airways become widened during inspiration and collapse during expiration(1).
Although the findings have been recognized by Cyhlarz in autopsies since 1897, only in 1932 Mounier-Kuhn associated endoscopic and radiological findings of widened airways with recurrent infections of the respiratory tract(1,2).
The disease is clinically characterized by the presence of repetitive respiratory infections, secretion accumulation and ineffective cough(1,2). A subtle predominance of the disease is observed in men, at the third or fourth decades of life, but the exact prevalence is still to be determined, with very few cases reported in the literature( 1–3). It is thought that the conjunctive tissue weakness associated with inhalation of air pollutants and tobacco smoke play a key role in the development of such a syndrome(1).
The present study is aimed at describing the main clinical, radiographic and high resolution computed tomography (HRCT) findings in TBM, also known as Mounier- Kuhn syndrome. The study was approved by the Committee for Ethics in Research of the authors' institution under number 065/2010.
CASE REPORT
A male, 33-year-old painter, active smoker (two cigarette packs a day), with a previous history of treatment for pulmonary tuberculosis in 1979, presented fever, nocturnal sudoresis, productive cough, chest pain, dyspnea and chest wheezing for two months, was referred to the institution for pneumological evaluation. At clinical examination, the patient showed nail clubbing (Hippocratic fingers), lung auscultation with bilateral crepitus in the lower thirds. Spirometry demonstrated severe obstructive ventilatory disorder: FVC = 3.40 (75%), FEV
1 = 1.49 (40%), TI = 39.1%.
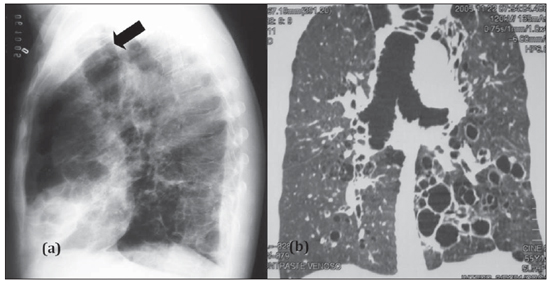
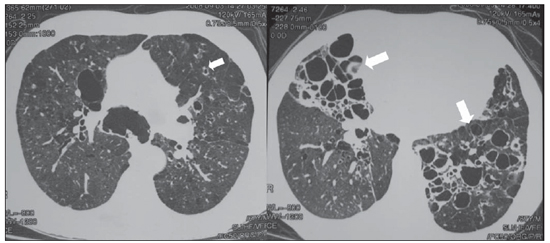
Chest radiography demonstrated increase in the lung volume and transparency, with signs of reticular interstitial infiltrate predominating in the central regions. The trachea presented increased caliber, with a maximum transverse diameter of 40.0 mm (Figure 1). High resolution CT demonstrated details of the parenchymal alterations particularly characterized by predominantly cystic bronchiectasis clustered in the central regions, diffuse perfusional alterations in the pulmonary parenchyma (mosaic pattern of attenuation), besides increased caliber of the trachea and of the main bronchi which also presented jagged contours corresponding to tracheobronchial diverticulosis (Figure 2).
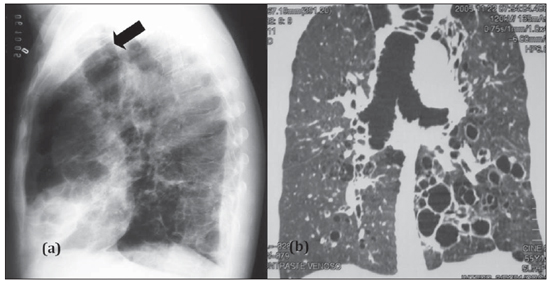
Figure 1. Lateral chest radiography (a) showing increased tracheal caliber (arrow). Multiplanar (MPR) reconstruction (b) demonstrates increase in the caliber of the trachea, main bronchi and bronchiectasis.
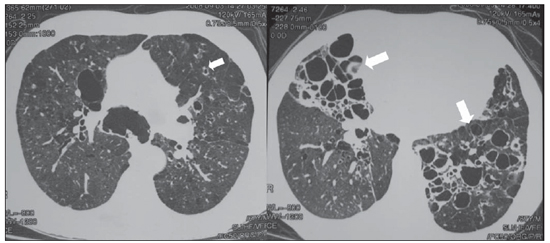
Figure 2. Axial chest HRCT showing increase in the caliber of main bronchi and diffuse bronchiectasis (arrows).
Over the years, the patient presented a progressive worsening of the dyspnea with chronic suppuration (sputum analysis demonstrated
Pseudomonas aeruginosa colonization) and several hospital admissions because of infective exacerbation. In 2009, the patient was admitted to the hospital, progressing to fatal respiratory failure.
DISCUSSION
The diagnosis of tracheobronchomegaly may be achieved when the diameters of the trachea and of the right and left main bronchi are > 3.0, 2.4 and 2.3 cm, respectively( 1,2). Frequently, TBM is associated with tracheal diverticulosis and bronchiectasis. The tracheal diverticulum may be originated from increased compliance of the tracheal wall and development of a redundant membranous tissue(4). The disease can be diagnosed by means of plain chest radiography in association with clinical findings, but the investigation with computed tomography allows a more accurate evaluation of abnormalities in the affected airways as well as of the disease extent(5). The diminished clearing of secretions observed in this syndrome causes its accumulation, leading to repetitive respiratory infections which results in the development of the mentioned anatomic alterations and consequential functional impairment, ranging from minimal functional damage to respiratory failure leading to death(1,3). Respiratory function testing demonstrate an obstructive pattern, increased residual volume and decreased CO
2 diffusion in the presence of parenchymal disease; in advanced cases, a predominance of a restrictive pattern secondary to fibrosis is observed.( 1). The treatment is generally supportive, by means of respiratory physiotherapy, appropriate antibiotic therapy for recurrent infections and tobacco use cessation. Success has been achieved in few cases with tracheal stenting to prevent expiratory collapse(6).
CONCLUSION
Suspicion of tracheobronchomegaly should be raised in patients with chronic pulmonary suppuration, repetitive respiratory infections and ineffective cough and whose chest radiography demonstrates increased tracheal caliber. High resolution computed tomography (HRCT) plays a relevant role in the accurate evaluation of abnormalities present in the lung parenchyma.
REFERENCES
1. Menon B, Aggarwal B, Iqbal A. Mounier-Kuhn syndrome: report of 8 cases of tracheobronchomegaly with associated complications. South Med J. 2008;101:83–7.
2. Nóbrega BB, Figueiredo SS, Cavalcante LP, et al. Traqueobroncomegalia (síndrome de Mounier- Kuhn): relato de caso e revisão da literatura. Radiol Bras. 2002;35:187–9.
3. Schwartz M, Rossoff L. Tracheobronchomegaly. Chest. 1994;106:1589–90.
4. Shin MS, Jackson RM, Ho KJ. Tracheobronchomegaly (Mounier-Kuhn syndrome): CT diagnosis. AJR Am J Roentgenol. 1988;150:777–9.
5. Sorenson SM, Moradzadeh E, Bakhda R. Repeated infections in a 68-year-old man. Chest. 2002;121:644–6.
6. Collard P, Freitag L, Reynaert MS, et al. Respiratory failure due to tracheobronchomalacia. Thorax. 1996;51:224–6.
1. Fellow PhD degree in Sciences of Health, Universidade Federal de Minas Gerais (UFMG), MD, Physician Assistant at Department of Imaging Diagnosis – Hospital Júlia Kubitschek – FHEMIG, Belo Horizonte, MG, Brazil.
2. Physician Assistant at Department of Pneumology – Hospital Júlia Kubitschek – FHEMIG, Belo Horizonte, MG, Brazil.
Mailing Address:
Dra. Andréa de Lima Bastos
Hospital Júlia Kubitschek – Fundação Hospitalar do Estado de Minas Gerais (FHEMIG), Unidade de Diagnóstico por Imagem
Rua Doutor Cristiano Rezende, 2745, Bairro Flávio Marques Lisboa (Barreiro)
Belo Horizonte, MG, Brazil, 30620-470
E-mail: andblima@yahoo.com.br
Received November 30, 2010.
Accepted after revision March 14, 2011.
Study developed at Hospital Júlia Kubitschek – FHEMIG, Belo Horizonte, MG, Brazil.
 Vol. 44 nº 3 - May / June of 2011
Vol. 44 nº 3 - May / June of 2011