INTRODUCTION
Snapping knee syndrome corresponds to the feeling of clicking, snapping or abrupt movement during flexion of the joint. The snapping or clicking may be produced by the friction of soft tissues over a bone prominence or by the abnormal and abrupt motion of intra-articular structures. Association with symptoms is necessary for the diagnosis of such a syndrome. Not always, crepitations that are audible or may be felt by the patient, or even a palpable snapping felt at clinical examination are symptomatic or pathological.
Snapping syndrome has been diagnosed and reported in the literature, involving major joints such as shoulders, elbows, hips, knees and ankles(1). Most frequently, the hip joint is affected(1-4). In general, the symptoms associated with snapping syndrome are most frequently related to pain complaints, however, neurological changes may eventually occur, as in the case of snapping of the ulnar nerve at the elbow(5).
In the knee, the most frequent causes of snapping syndrome are related to meniscal abnormalities, to the biceps femoris tendon and gracilis and semitendinosus tendons in the posteromedial corner(6-11).
The present study describes a case of snapping in the distal myotendinous junction of the sartorius muscle of a patient who also presented knee hyperextension. No description of this type of snapping was found in the literature.
CASE REPORT
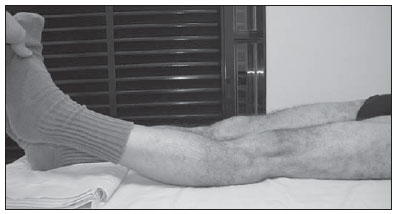
Male, 58-year-old white patient with a history revision arthroplasty of the left hip, with complaints of pain associated with the felling of clicking in the medial aspect of the left knee six months after surgery. At clinical examination, besides the confirmation of a palpable snapping during knee flexion and extension, a knee hyperextension was identified (Figure 1). A tendency towards genu recurvatum was observed in both knees, but most noticeable in the symptomatic knee. A 9 mm discrepancy was also identified in the length of the lower limbs, with shortening of the previously operated lower limb.
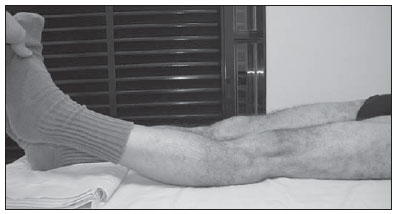
Figure 1. Male, 58-year-old patient. Clinical examination revealed knee hyperextension.
In the present case, the cervical-diaphyseal angle of the left hip prosthesis measured about 135 degrees, while the cervical-diaphyseal angle of the right femur measured about 130 degrees; and the ratio between the offset at the prosthesis side and the contralateral offset was approximately 95%.
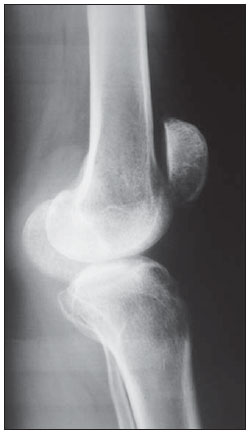
Plain radiography of the left knee confirmed the hyperextension and demonstrated minimum marginal osteophytes (Figure 2). Knee ultrasonography was requested for the evaluation of the snapping of one of the pes anserinus tendons, with suspicion of semitendinosus or gracilis snapping.
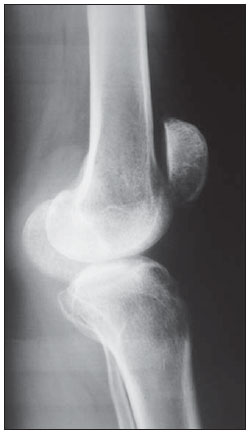
Figure 2. Plain radiography lateral view, confirming knee hyperextension, with a subtle genu recurvatum deformity.
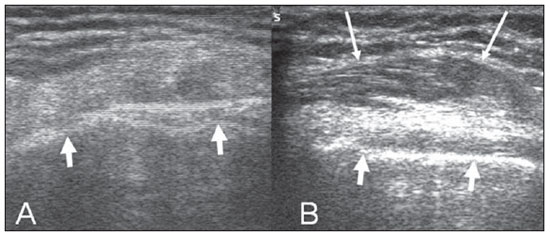
At ultrasonography, the components of pes anserinus were identified at the posteromedial corner. The patient was evaluated in dorsal decubitus with a slight rotation of the knee to allow the assessment of the region of interest. Subsequently, these tendons were dynamically evaluated during flexion and extension. Ultrasonography confirmed the snapping at the posteromedial corner, but such snapping was exclusively related to the abrupt movement of the sartorius in relation to the medial condyle of the femur (Figure 3).
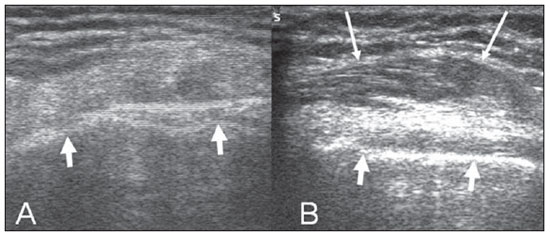
Figure 3. Axial sections at ultrasonography. In A, with the flexed knee, no structure with muscular pattern is observed between the subcutaneous layer and the bone surface (short arrows). On B, the image acquired with the knee in hyperextension, demonstrates the sartorius muscle (long arrows), superficially located over the bone contours (short arrows).
As the painful symptoms were relatively well tolerated by the patient, a conservative approach was adopted to treat the snapping, and after 18 months the patient presented stable complaints as compared with those presented at the onset of the symptoms. The treatment comprised physiotherapy for muscular strengthening and utilization of insoles to compensate for the discrepancy in the length of lower limbs.
DISCUSSION
It did not become clear for the authors whether the knee hyperextension, the total hip arthroplasty or a combination of both factors might be directly or indirectly related to the occurrence of snapping of the sartorius muscle in this case. The symptoms onset occurred approximately six months after arthroplasty and, for this reason, it is possible to hypothesize that some change in the mechanical axis of the lower limb may have occurred.
Patients submitted to total arthroplasty of the hip may develop changes in the alignment of the lower limbs after the procedure(12). A limitation in the present study was the fact that the pre- and postoperative panoramic radiographs of the lower limb were not available for evaluation. Total hip arthroscopy may induce a change in the mechanical axis, altering the spatial position of the femoral head center, with possible reduction of the femoral offset(13). Such reduction of femoral prosthesis offset, on its turn, may lead to a lateralization of the mechanical axis(12). In the case described in the present study the reduction of the femoral prosthesis offset in relation to the contralateral femur was approximately 5%.
In the knee, the snapping syndrome is more commonly associated with meniscal disorders(7-9). The lateral discoid meniscus may cause symptomatic snapping, particularly in the case of type III lateral discoid meniscus, a rare variant of discoid meniscus also known as Wrisberg variant where the posterior attachment between the meniscus and the tibia is absent, with significantly greater mobility of the meniscus(8,14). Cases of snapping at the posterolateral corner of the knee related to the biceps femoris tendon and to the popliteus tendon(6,15) have been reported. Most rarely, the snapping in the knee may be caused by intra-articular tumors(16). Cases of snapping in the posteromedial corner have been described, particularly those related to the semitendinosus tendon around the semimembranosus muscle(10,11).
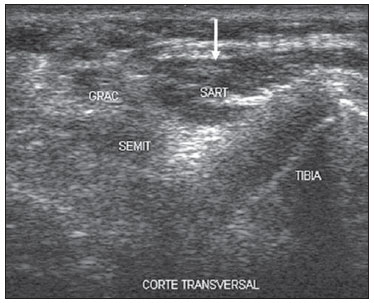
The study of snapping tendons can be made by clinical examination and by means of ultrasonography, which allows the dynamic study of the tendons(2,3,5,10,11). In the suspicion of intra-articular disorders, the literature emphasizes the utilization of magnetic resonance imaging(1,12). In the present case, ultrasonography was capable of characterizing the snapping sartorius muscle instead of snapping semitendinosus tendon, which is more prevalent at the posteromedial corner. At ultrasonography, the sartorius muscle was easily differentiated from other components of the pes anserinus, because of its more anterior position, greater cross-sectional area at the level of the femoral condyle, and because of its hypoechoic composition related to the muscular fibers. The gracilis and semitendinosus tendons present a fibrillar pattern, are more echogenic and present a smaller cross-sectional area (Figure 4). In the case of snapping of the posteromedial corner related to the semitendinosus and the gracilis tendons, the excision of such tendons with successful relief of symptoms has already been reported in the literature(10,11,17). No report on snapping knee related to the sartorius muscle was found by the authors in the literature written in Portuguese and English languages.
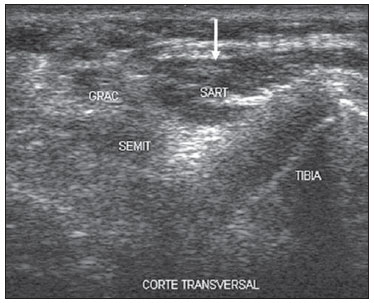
Figure 4. Axial oblique section at ultrasonography of the posteromedial corner region of the knee demonstrating the differentiation between the sartorius muscle (arrow) and the gracilis (GRAC) and semitendinosus (SEMIT) tendons.
Ultrasonography is an important method for the diagnosis of snapping in the posteromedial corner of the knee(10,11). In the present case, the relevance of ultrasonography was confirmed, and a different cause for posteromedial snapping in the knee was identified.
REFERENCES
1. Silva HR, Simão MN, Elias Jr J, et al. Diagnóstico por imagem nas síndromes do estalido ou do ressalto. Radiol Bras. 2009;42:49-55.
2. Pelsser V, Cardinal E, Hobden R, et al. Extraarticular snapping hip: sonographic findings. AJR Am J Roentgenol. 2001;176:67-73.
3. Deslandes M, Guillin R, Cardinal E, et al. The snapping iliopsoas tendon: new mechanisms using dynamic sonography. AJR Am J Roentgenol. 2008;190:576-81.
4. Costa FP, Canto RST. Quadril em ressalto. Rev Bras Ortop. 1990;25:369-72.
5. Jacobson JA, Jebson PJL, Jeffers AW, et al. Ulnar nerve dislocation and snapping triceps syndrome: diagnosis with dynamic sonography - report of three cases. Radiology. 2001;220:601-5.
6. Lokiec F, Velkes S, Schindler A, et al. The snapping biceps femoris syndrome. Clin Orthop Relat Res. 1992;(283):205-6.
7. Goldstein RC, Andrade Jr AM. Lesão cística de menisco: abordagem por via artroscópica. Rev Bras Ortop. 1998;33:371-6.
8. Kelly BT, Green DW. Discoid lateral meniscus in children. Curr Opin Pediatr. 2002;14:54-61.
9. Poey C, Couette P, Savorit L, et al. Hypermobile snapping medial meniscus: features on flexion-extension MRI. J Radiol. 2008;89(1Pt1):53-6.
10. Bollen SR, Arvinte D. Snapping pes syndrome: a report of four cases. J Bone Joint Surg Br. 2008;90:334-5.
11. Karataglis D, Papadopoulos P, Fotiadou A, et al. Snapping knee syndrome in an athlete caused by the semitendinosus and gracilis tendons. A case report. Knee. 2008;15:151-4.
12. Umeda N, Miki H, Nishii T, et al. Progression of osteoarthritis of the knee after unilateral total hip arthroplasty: minimum 10-year follow-up study. Arch Orthop Trauma Surg. 2009;129:149-54.
13. Bourne RB, Rorabeck CH, Patterson JJ, et al. Tapered titanium cementless total hip replacements: a 10- to 13-year follow up study. Clin Orthop Relat Res. 2001;(393):112-20.
14. Singh K, Helms CA, Jacobs MT, et al. MRI appearance of Wrisberg variant of discoid lateral meniscus. AJR Am J Roentgenol. 2006;187:384-7.
15. Cooper DE. Snapping popliteus tendon syndrome. A cause of mechanical knee popping in athletes. Am J Sports Med. 1999;27:671-4.
16. Mine T, Ihara K, Taguchi T, et al. Snapping knee caused by intra-articular tumors. Arthroscopy. 2003;19:E21.
17. Geeslin AG, LaPrade RF. Surgical treatment of snapping medial harmstring tendons. Knee Surg Sports Traumatol Arthrosc. 2010;18:1294-6.
1. PhD, Professor, Division of Radiology, Centro de Ciências das Imagens e Física Médica (CCIFM) – Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil.
2. PhD, Teacher at the Service of Medical Residency in Orthopedics & Traumatology of Santa Casa de Ribeirão Preto, Ribeirão Preto, SP, Brazil.
Mailing Address:
Dr. Marcello Henrique Nogueira-Barbosa
Divisão de Radiologia, CCIFM, FMRP-USP
Avenida Bandeirantes, 3900, Campus Universitário, Monte Alegre
Ribeirão Preto, SP, Brazil, 14048-900
E-mail: marcello@fmrp.usp.br
Received October 11, 2010.
Accepted after revision February 1, 2011.
Study developed at Centro de Ciências das Imagens e Física Médica (CCIFM) – Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil.
 Vol. 44 nº 3 - May / June of 2011
Vol. 44 nº 3 - May / June of 2011