INTRODUCTION
Magnetic resonance imaging (MRI) is the imaging method of choice for the assessment of meniscal lesions. The development of new sequences, improvements in image quality and more powerful magnets in association with excellent contrast resolution and multiplanar capability allow the diagnosis of meniscal lesions with high accuracy. However, an appropriate understanding of the meniscal anatomy and parameniscal structures, particularly the ligaments, is essential for a correct diagnosis, avoiding a number of possible errors caused by pseudo-lesions and anatomical variations.
The present study reviews the anatomic variations of the menisci as well as the anatomy and variations of the perimeniscal ligamentous structures, with emphasis on MRI.
VARIATIONS OF THE MENISCAL MORPHOLOGY
Discoid meniscus
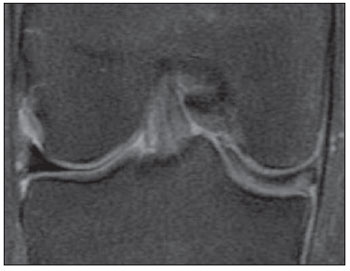
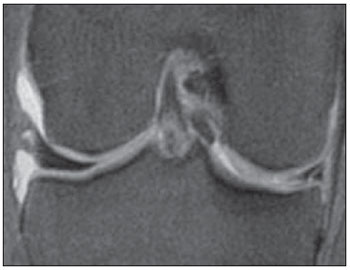
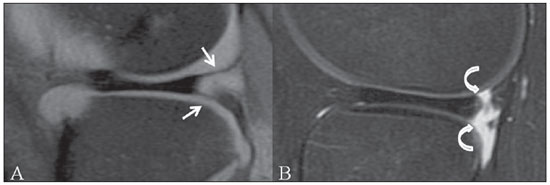
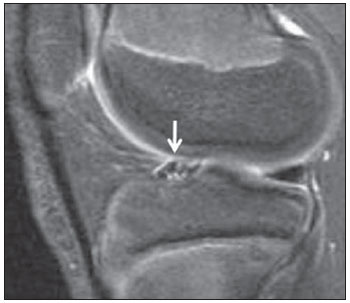
Discoid meniscus is a morphological alteration, probably of embryonal etiology, in which the meniscus presents a disc-like shape, instead of the habitual crescent shape. Its incidence is much greater in the lateral than in the medial meniscus, being REVIEW ARTICLE found in 0.7% to 5.2% of the Western countries population and in up to 15.3% of patients submitted to arthroscopy in Eastern countries(1,2), although anatomical studies in neonate cadavers demonstrate a much greater incidence (77%) in the lateral meniscus( 3), which corroborates the theory of a variation of embryonal nature. The clinical presentation is variable and depends on the type of meniscus and presence or absence of lesion, and may be asymptomatic or be associated with symptoms such as pain, knee clicking and decreased extension capacity, particularly in children and young adults(4,5). The most utilized classification is the one developed by Watanabe( 6) describing three patterns: type I or completely discoid, with the meniscus covering the entire tibial plateau (Figure 1); type II or incomplete, with a semilunar appearance, partially covering the tibial plateau (Figure 2); and type III or Wrisberg type, the rarest variant, resulting from the absence of the coronary and posterior meniscocapsular ligaments (Figure 3). The Wrisberg variant may occur in the discoid meniscus or in those with the habitual morphology, resulting in a hypermobile meniscus, and is more likely to become symptomatic at earlier ages(7). At MRI, discoid meniscus is > 14 mm in width in the coronal plane in the section corresponding to the middle segment of the body(8), and in the sagittal plane, the appearance of a bow tie, with a continuity between the anterior and posterior horns, remaining on more than two images(9), and possibly varying according to the slice thickness. Other criteria include a difference of > 2mm in the height of the horns of the medial and lateral menisci(2), meniscus-tibia ratio
> 20% and percentage of meniscus coverage
> 75%(10).
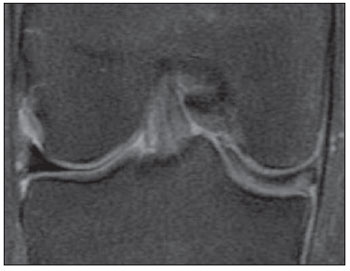
Figure 1. Coronal proton-density FS image depicting complete discoid-type medial meniscus occupying the whole extent of the tibial plateau, with a trace of horizontal tear.
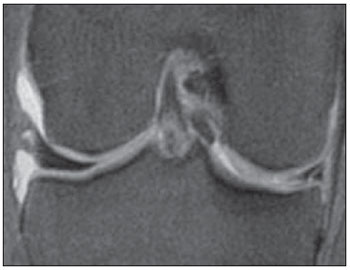
Figure 2. Coronal proton-density FS image at the level of the body depicting lateral meniscus partially covering the tibial plateau, corresponding to partial discoid meniscus (type II). Notice a lesion in the medial meniscus.
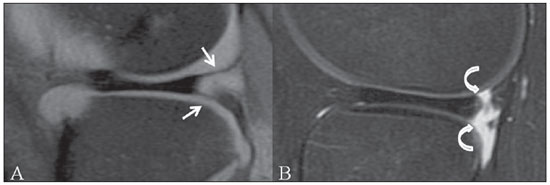
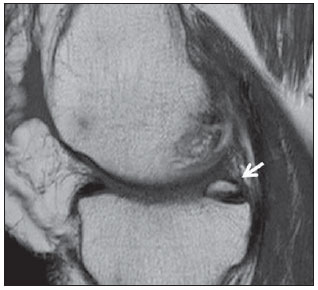
Figure 3. Sagittal proton-density FS image depicting upper and lower meniscocapsular fascicles (white arrows) adjacent to the posterior horn of the lateral meniscus (A) and discoid lateral meniscus with absence of fascicles (curved arrows), corresponding to Wrisberg variant (B).
A high signal band inside the discoid menisci may be observed in up to 85% of the cases, possibly corresponding either to early degenerative changes or to persistence of vascularization in children(11). The most frequent meniscal tear in patients with discoid lateral meniscus continues to be the isolated tear of the medial meniscus, at a rate similar to that in patients without discoid meniscus. However, the incidence of tears in discoid lateral meniscus is much higher than that observed in morphologically normal menisci(2,9). The lesion pattern may be related to the type of discoid lateral meniscus, with horizontal tears being more prevalent in the type I or complete, and the radial, degenerative and complex tears, in the incomplete type(1). Other lesion pattern in discoid meniscus is the central perforation, whose appearance is very similar to the bucket-handle tear pattern(12), and the differential diagnosis at MRI may be quite complicated in the lateral meniscus, because of characteristics overlapping. In such cases, the correlation with the clinical trauma history is essential.
In young patients with a history of pain, snapping knee or extension block with discoid meniscus and absence of meniscocapsular fascicles and coronary ligaments, the MRI diagnosis of the Wrisberg variant should be considered. Normally, the fascicles of the lateral meniscus can be clearly visualized at MRI, while the coronary ligaments are generally not identifiable, even in individuals with normal menisci; therefore they should not be included in the criteria for the diagnosis of Wrisberg variant at MRI(13).
Other less frequent anatomic meniscal variations
With the exception of discoid meniscus, other meniscal malformations are much less frequent, with an incidence of 0.3%(14). Such variations are more prevalent in the population of Asian countries, in the lateral meniscus and are frequently asymptomatic( 15). Such variations include ring-shaped meniscus, both partial or complete meniscal hypoplasias, double-layer meniscus and meniscal insertion abnormalities(14,16–20).
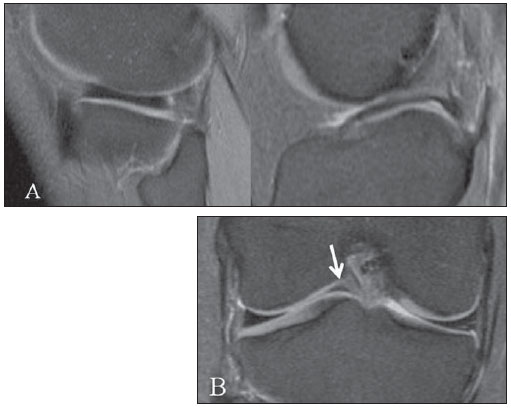
The ring-shaped meniscus is circular shaped, with the appearance of the external portion of the ring being similar to that of a normal meniscus – well defined and angular –, and does not present mobility of the internal segment adjacent to the intercondylar incisure (Figure 4). Such absence of mobility in the innermost portion is not defined by image criteria at MRI, but by means of tests with a probe during arthroscopy. Such considerations in association with the patients’ age and clinical history are fundamental for the differential diagnosis with central perforation of a discoid meniscus or a “bucket handle” tear(17). In the central perforation of a discoid meniscus, the internal margins of the meniscus are degenerated and irregular and there are other associated degenerative changes, such as osteophytes and chondral lesions(12,17).
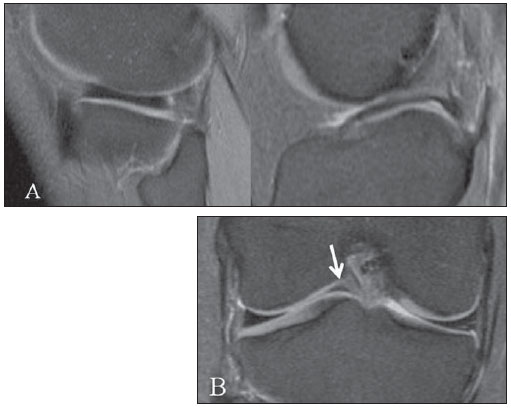
Figure 4. Sagittal proton-density FS image (A) and coronal proton-density FS image (B) depicting lateral meniscus with preserved morphology and signal, in continuity with a low signal band (white arrow) positioned at the middle line, corresponding to a “ringshaped” meniscus.
An anomalous meniscus band is usually smaller than the original meniscus, and is free and mobile, except for the insertion, normally at the posterior horn. The double layer meniscus presents a second layer parallel to the normal meniscus and peripherally attached to the capsule(15).
The anomalous insertion of the anterior horn of the medial meniscus into the anterior cruciate ligament is an infrequent variation, with a variable incidence reported in literature (never > 2.2%(16,21). At MRI, such abnormality is seen as a bandshaped structure with low signal intensity, extending from the anterior horn of the medial meniscus to the anterior cruciate ligament, in an almost parallel pathway, with a variable thickness, sometimes too thin to be individualized at MRI. Its appearance is very similar to that of the infrapatellar fold, however it runs towards the fat pad of Hoffa or sometimes to the lower patellar pole, instead of inserting into the meniscus(16,22). The anomalous insertion may also occur between the posterior horn and the anterior cruciate ligament(20).
Meniscal ossicle
It is an uncommon change that normally occurs in the posterior horn of the medial meniscus, and is defined by the presence of cortical and trabecular bone with bone marrow surrounded by meniscal fibrocartilage (Figure 5). It is associated with a greater incidence of pain and lesions, probably because of interference in the meniscal mobility and the mass effect. The identification of lesions at MRI is difficult on account of the presence of the ossicle(23). The diagnosis by means of conventional radiography may be difficult, and differentiation should be made with osteochondral loose bodies. At MRI, the ossicle is usually well defined and presents high-signal intensity on T1- and T2-weighted sequences, with signal loss on sequences with fat suppression, while loose bodies usually present low signal intensity on T1-weighted sequences( 15).
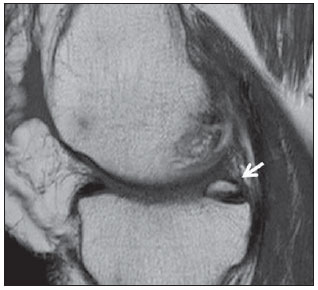
Figure 5. Sagittal T1-weighted image depicting posterior horn of the medial meniscus (white arrow) with high signal intensity on T1 with the same pattern as the bone marrow’s, in a case of meniscal ossicle.
Meniscocapsular ligaments
Meniscocapsular ligaments comprise the meniscofemoral and meniscotibial or coronary components that attach the meniscus to the posterior portion of the femur and tibia, respectively. Meniscotibial ligaments are short, and contribute in the maintenance of appropriate positioning of the meniscus in relation to the tibial plateau and aid in the formation of deep portion of the capsule, laterally. In the medial portion, both the meniscofemoral and meniscotibial ligaments contribute in the deep portion of the capsule(24) and no cleavage plane is defined between them(25). A lesion in this region may involve the meniscocapsular ligaments or the peripheral portion of the meniscus, known as meniscocapsular separation, and causes meniscus hypermobility. Such diagnosis is difficult at MRI and must be considered in the presence of perimeniscal fluid and if the external contour of the meniscus is irregular. It is potentially healable lesion, either with or without meniscal suture(25,26).
Intermeniscal ligaments
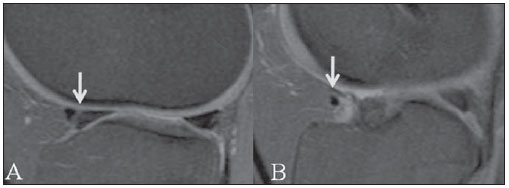
Intermeniscal ligaments comprise the anterior and posterior transverse ligaments as well as the medial and lateral oblique ligaments(27). The anterior transverse ligament is present in 53% to 94% of cases, with variable appearance and insertions(27,28), with a cord-like or flattened appearance and insertions into the anterior horns of the meniscus or capsular(29). At MRI, it can be identified at the lower portion of the fat pad of Hoffa at any plane, however it is more easily identified on the sagittal plane, with an appearance of a small nodular image with low signal intensity, which may simulate a lesion in the anterior horns of the meniscus (Figure 6), and is more common in the lateral one(30). The diagnosis of pseudotear can be avoided by following the course of the ligament on several consecutive images. The posterior transverse ligament consists of a fibrous band that connects the posterior horns of the menisci, passing in front of the posterior cruciate ligament, and is present in approximately 2% of the knees(27). No description of its appearance at MRI was found in the literature. The correlation with the appearance of the other ligaments and respective anatomic description suggests that it is seen as a low-signal-intensity band crossing the middle line, anteriorly to the posterior cruciate ligament(31).
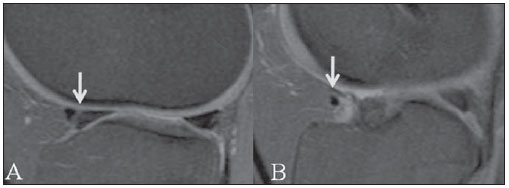
Figure 6. Sagittal proton-density FS image depicting transverse ligament (white arrows) causing pseudotear in the anterior horn of lateral meniscus (A), but easily identifiable in its course in the lower portion of the infrapatellar fat pad (B).
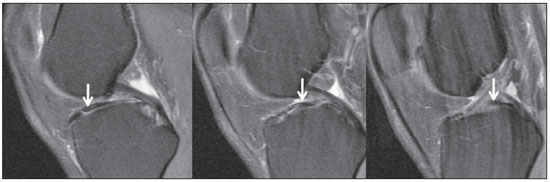
The oblique intermeniscal ligaments connect the anterior horn of a meniscus to the posterior horn of the other, being called as medial or lateral, according to the anterior insertion. They are present in 1% to 4% of the knees(32) and its presence is related to the presence of the transverse ligament( 27). At MRI it is seen as a structure with low signal intensity on any sequence, crossing the intercondylar incisure intermingled with the cruciate ligaments, with the appearance similar to that of a displaced meniscal fragment in the middle line or a double posterior cruciate, sometimes simulating a “bucket handle” tear (Figure 7). The identification of the ligament course and the presence of a meniscus with the habitual appearance, with preservation of the two “bow-tie” images and the typical triangular appearance in the coronal plane, are useful to rule out the possibility of a “bucket handle” lesion (33).
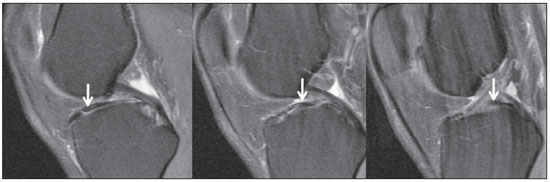
Figure 7. Sagittal proton-density FS image depicting oblique medial intermeniscal ligament (white arrows) extending from the anterior horn of the medial meniscus to the posterior horn of the lateral meniscus, intermingled with cruciate ligaments, simulating fragment at the middle line.
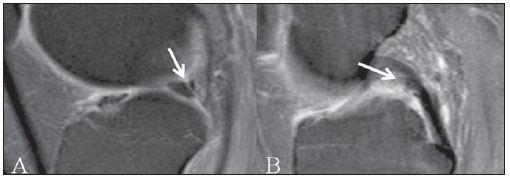
The meniscofemoral ligaments extend from the posterior horn of the lateral meniscus to the internal portion of the medial femoral condyle, and are denominated ligament of Humphrey, as it pass in front of the posterior cruciate ligament, and ligament of Wrisberg as it pass behind it. According to the literature, the incidence of such ligaments is between 50% and 93% with presence of only one of both of them, with possible variations in thickness and in the proximal and distal insertions(34).
The correct understanding of anatomy and orientation of these ligaments on MRI sequences is essential to avoid misinterpretation as meniscal lesions or loose bodies( 35). A pseudotear in the posterior horn of the lateral meniscus may be present in up to 63% of the cases (Figure 8), with a vertical or, most frequently, oblique orientation from anterosuperior to posteroinferior( 36). An apparent lateral extension of the meniscofemoral ligament insertion, on four or more images beyond the posterior cruciate ligament, should be considered as a suspicion of lesion in the posterior horn of the lateral meniscus, particularly in cases where there is an association with rupture of the anterior cruciate ligament(37).
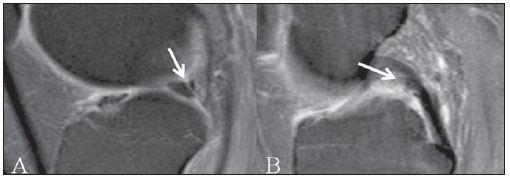
Figure 8. Sagittal proton-density FS image depicting meniscofemoral ligament of Humphrey (white arrows) inserting into the posterior horn of the lateral meniscus (A) and passing anteriorly to the posterior cruciate ligament (B).
The extension of the fibers of the anterior cruciate ligament to the anterior horn of the lateral meniscus may cause a speckled or dotted appearance seen on the two most central images of the meniscus (Figure 9) simulating a lesion (38,39). The presence of an intra-articular and extrasynovial band between the posterior horn of the lateral meniscus and the anterior cruciate ligament, functioning as an extension of the meniscal insertion, is a frequent finding at arthroscopies performed on cadavers(40), but never described at MRI.
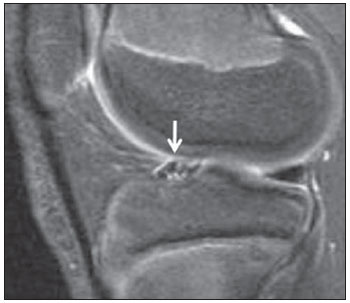
Figure 9. Sagittal T2-weighted FS image depicting a dotted appearance of the anterior horn of the lateral meniscus (white arrow), attributed to the insertion of the anterior cruciate ligament fibers
The detailed knowledge of the anatomy and variations of perimeniscal ligamentous structures, despite the fact that some of these variations are quite infrequent, is of fundamental relevance for the correct evaluation of meniscal lesions, thus avoiding a variety of possible diagnostic errors.
REFERENCES
1. Bin SI, Kim JC, Kim JM, et al. Correlation between type of discoid lateral menisci and tear pattern. Knee Surg Sports Traumatol Arthrosc. 2002;10:218–22.
2. Rohren EM, Kosarek FJ, Helms CA. Discoid lateral meniscus and the frequency of meniscal tears. Skeletal Radiol. 2001;30:316–20.
3. Kale A, Kopuz C, Edýzer M, et al. Anatomic variations of the shape of the menisci: a neonatal cadaver study. Knee Surg Sports Traumatol Arthrosc. 2006;14:975–81.
4. Good CR, Green DW, Griffith MH, et al. Arthroscopic treatment of symptomatic discoid meniscus in children: classification, technique, and results. Arthroscopy. 2007;23:157–63.
5. Jordan MR. Lateral meniscal variants: evaluation and treatment. J Am Acad Orthop Surg. 1996;4: 191–200.
6. Watanabe M, Takeda S, Ikeuchi H. Atlas of arthroscopy. Tokyo: Igaku-Shoin; 1978. p. 88.
7. Moser MW, Dugas J, Hartzell J, et al. A hypermobile Wrisberg variant lateral discoid meniscus seen on MRI. Clin Orthop Relat Res. 2007;456: 264–7.
8. Araki Y, Ashikaga R, Fujii K, et al. MR imaging of meniscal tears with discoid lateral meniscus. Eur J Radiol. 1998;27:153–60.
9. Silverman JM, Mink JH, Deutsch AL. Discoid menisci of the knee: MR imaging appearance. Radiology. 1989;173:351–4.
10. Samoto N, Kozuma M, Tokuhisa T, et al. Diagnosis of discoid lateral meniscus of the knee on MR imaging. Magn Reson Imaging. 2002;20:59– 64.
11. Stark JE, Siegel MJ, Weinberger E, et al. Discoid menisci in children. MR features. J Comput Assist Tomogr. 1995;19:608–11.
12. Choi JW, Chung HW, Ahn JH, et al. Central hole tear of the discoid meniscus of the knee in magnetic resonance imaging: mimicking the buckethandle tear. J Comput Assist Tomogr. 2009;33: 155–9.
13. Singh K, Helms CA, Jacobs MT, et al. MRI appearance of Wrisberg variant of discoid lateral meniscus. AJR Am J Roentgenol. 2006;187:384– 7.
14. Fujikawa A, Amma H, Ukegawa Y, et al. MR imaging of meniscal malformations of the knee mimicking displaced bucket-handle tear. Skeletal Radiol. 2002;31:292–5.
15. Tyler P, Datir A, Saifuddin A. Magnetic resonance imaging of anatomical variations in the knee. Part 2: miscellaneous. Skeletal Radiol. 2010;39:1175– 86.
16. Cha JG, Min KD, Han JK, et al. Anomalous insertion of the medial meniscus into the anterior cruciate ligament: the MR appearance. Br J Radiol. 2008;81:20–4.
17. Kim YG, Ihn JC, Park SK, et al. An arthroscopic analysis of lateral meniscal variants and a comparison with MRI findings. Knee Surg Sports Traumatol Arthrosc. 2006;14:20–6.
18. Ginés-Cespedosa A, Monllau JC. Symptomatic ring-shaped medial meniscus. Clin Anat. 2007; 20:994–5.
19. Atay OA, Aydingöz U, Doral MN, et al. Symptomatic ring-shaped lateral meniscus: magnetic resonance imaging and arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2002;10:280–3.
20. Bhargava A, Ferrari DA. Posterior medial meniscus- femoral insertion into the anterior cruciate ligament. A case report. Clin Orthop Relat Res. 1998;348:176–9.
21. Rainio P, Sarimo J, Rantanen J, et al. Observation of anomalous insertion of the medial meniscus on the anterior cruciate ligament. Arthroscopy. 2002; 18:E9.
22. Cothran RL, McGuire PM, Helms CA, et al. MR imaging of infrapatellar plica injury. AJR Am J Roentgenol. 2003;180:1443–7.
23. Tuite MJ, De Smet AA, Swan JS, et al. MR imaging of a meniscal ossicle. Skeletal Radiol. 1995; 24:543–5.
24. Bikkina RS, Tujo CA, Schraner AB, et al. The “floating” meniscus: MRI in knee trauma and implications for surgery. AJR Am J Roentgenol. 2005;184:200–4.
25. De Maeseneer M, Shahabpour M, Vanderdood K, et al. Medial meniscocapsular separation: MR imaging criteria and diagnostic pitfalls. Eur J Radiol. 2002;41:242–52.
26. De Maeseneer M, Lenchik L, Starok M, et al. Normal and abnormal medial meniscocapsular structures: MR imaging and sonography in cadavers. AJR Am J Roentgenol. 1998;171:969–76.
27. Zivanoviƒ S. Menisco-meniscal ligaments of the human knee. Anat Anz. 1974;135:35–42.
28. Aydingöz Ü, Kaya A, Atay OA, et al. MR imaging of the anterior intermeniscal ligament: classification according to insertion sites. Eur Radiol. 2002;12:824–9.
29. Nelson EW, LaPrade RF. The anterior intermeniscal ligament of the knee. An anatomic study. Am J Sports Med. 2000;28:74–6.
30. Herman LJ, Beltran J. Pitfalls in MR imaging of the knee. Radiology. 1988;167:775–81.
31. Simão MN, Gomes OH, Trad HS, et al. Ligamentos menisco-meniscais: revisão anatômica e causa de pseudolesões meniscais na RM. Rev Imagem. 2007;29(Supl 1):32, PA.4.17.
32. Sanders TG, Linares RC, Lawhorn KW, et al. Oblique meniscomeniscal ligament: another potential pitfall for a meniscal tear – anatomic description and appearance at MR imaging in three cases. Radiology. 1999;213:213–6.
33. Dorsay TA, Helms CA. Bucket-handle meniscal tears of the knee: sensitivity and specificity of MRI signs. Skeletal Radiol. 2003;32:266–72.
34. Cho JM, Suh JS, Na JB, et al. Variations in meniscofemoral ligaments at anatomical study and MR imaging. Skeletal Radiol. 1999;28:189–95.
35. Vahey TN, Bennett HT, Arrington LE, et al. MR imaging of the knee: pseudotear of the lateral meniscus caused by the meniscofemoral ligament. AJR Am J Roentgenol. 1990;154:1237–9.
36. Abreu MR, Chung CB, Trudell D, et al. Meniscofemoral ligaments: patterns of tears and pseudotears of the menisci using cadaveric and clinical material. Skeletal Radiol. 2007;36:729–35.
37. Park LS, Jacobson JA, Jamadar DA, et al. Posterior horn lateral meniscal tears simulating meniscofemoral ligament attachment in the setting of ACL tear: MRI findings. Skeletal Radiol. 2007; 36:399–403.
38. Muglia VF, Simão MN, Elias Jr E, et al. Erros comuns de interpretação de ressonância magnética de joelho: como reconhecê-los e evitá-los. Radiol Bras. 2001;34:161–6.
39. Shankman S, Beltran J, Melamed E, et al. Anterior horn of the lateral meniscus: another potential pitfall in MR imaging of the knee. Radiology. 1997;204:181–4.
40. Zemirline A, Gérard R, Uguen A, et al. Meniscoligamentous band between the posterior horn of the lateral meniscus and the anterior cruciate ligament: arthroscopic, anatomical and histological observations. Surg Radiol Anat. 2010;32:129–33.
1. PhD, MD, Radiologist at Central de Diagnóstico Ribeirão Preto (Cedirp), Radiologist Assistant at Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil.
2. PhD, MD, Radiologist, Professor of Radiology at Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil.
Mailing Address:
Dr. Marcelo Novelino Simão
Central de Diagnóstico Ribeirão Preto (Cedirp)
Avenida Nove de Julho, 1656, Jardim América
Ribeirão Preto, SP, Brazil, 14020-170
E-mail: marcelo_simao@hotmail.com
Received May 28, 2010.
Accepted after revision October 19, 2010.
Study developed at Centro de Ciências da Imagem e Física Médica (CCIFM) – Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRPUSP) and at Central de Diagnóstico Ribeirão Preto (Cedirp), Ribeirão Preto, SP, Brazil.
 Vol. 44 nº 2 - Mar. / Apr. of 2011
Vol. 44 nº 2 - Mar. / Apr. of 2011