Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 6 - Nov. / Dec. of 2010
Vol. 43 nº 6 - Nov. / Dec. of 2010
|
ORIGINAL ARTICLE
|
|
Brachial artery flow-mediated dilatation and intima-media thickness of carotid and brachial arteries: evaluation of individuals with and without risk factors for atherosclerosis* |
|
|
Autho(rs): Cristiane Martins Soares1; Hilton Augusto Koch2; Carlos Antônio Barbosa Montenegro3; Jorge Fonte de Rezende Filho4; Sandra Pereira Leite5; Antônio Rodrigues Braga Neto6; Carlos Eduardo Ferreira Novaes7 |
|
|
Keywords: Atherosclerosis; Endothelial dysfunction; Brachial artery flow-mediated dilatation; Intima-media complex of the carotid and brachial arteries. |
|
|
Abstract: INTRODUCTION
Atherosclerosis is a degenerative disease of multicausal etiology. Different (genetic and acquired) risk factors together may determine the occurrence of such disease in more than 50% of the adult population worldwide. Several conditions may affect carotid arteries of both men and women from their birth to the oldness. Among the main arteries affected by this condition, carotid arteries are the most studied ones, and among all the lesions of carotid arteries responsible for cerebrovascular disease of extracranial origin, 90% occur as a result of atherosclerosis. Other conditions are represented by non-atherosclerotic diseases such as kinking, Takayasu’s arteritis, fibromuscular dysplasia, extrinsic compressions, intimal dissection, aneurysm and trauma(1). Cerebrovascular accident (CVA) is one of the major causes of death worldwide, and the leading cause of disability in the population with > 50 years of age, being responsible for 10% of total deaths, 32.6% of deaths due to vascular causes, and 40% of early retirements in Brazil that is among the top ten countries with highest mortality rates for CVA(2). Cardiovascular disease is the first cause of death in developed countries, with high socioeconomic costs(3). In 2003, 69% of deaths with defined causes in Brazil were caused by non-transmissible chronic diseases, 32% of them of cardiovascular nature. In 2005, of five billion reais spent with the payment of authorizations for hospital admissions (except for labors), chronic diseases represented 58% of total expenditures, with 22% corresponding to the leading expenditures for cardiovascular diseases. Additionally, such chronic diseases may worsen the patients’ quality of life, affecting familial budgets in the poorest populations most frequently affected by these diseases and respective complications(4). The silent onset of vascular disease in the arterial wall progresses through the already known mechanisms including endothelial dysfunction, inflammation, plaque formation and vascular remodeling, later atherosclerotic plaque rupture and thrombosis(5). Endothelial dysfunction is a relevant step in the development of cardiovascular diseases(6) participating in the atheroma rupture responsible for 70% of acute myocardial infarctions in asymptomatic patients(7). The endothelial profile can be evaluated by the measurement of brachial artery flow-mediated dilatation (BAFMD), that is based on the capacity of production of nitric oxide released by the endothelium(8), which will promote arterial dilatation. Such measurement is achieved by means of ultrasonography, a noninvasive, low-cost method that allows the detection of preplaque endothelial dysfunction and provision of prophylactic treatment to avoid the worsening of the condition resulting from such alterations. Another aspect of carotid disease to be observed is its relationship with intima-media thickening (IMT), that is considered as a cardiovascular risk factor and can be a good marker for the development and prediction of future systemic vascular accidents(9). In healthy individuals, the maximum intima-media thickness of the common carotid artery at the prebifurcation site is 0.8 mm. Values between 0.9 and 1.4 mm are considered as thickening. In cases where the thickness is > 1.4 mm, atheromatous plaque is characterized(10). The present study was aimed at observing the vascular profile of both men and women with risk factors for atherosclerosis, utilizing BAFMD and IMT of carotid and brachial arteries. MATERIALS AND METHODS In the period from March to August 2004, 112 patients of the general and specialty infirmaries of Santa Casa da Misericórdia do Rio de Janeiro, RJ, Brazil, were invited to participate in the study. Such patients were divided into groups as follows: women with risk factors (n = 49), female control group (n = 24), men with risk factors (n = 21) and male control group (n = 18). All the patients included in the control groups were normotensive, non-smokers, non-diabetic, with no familial history of vascular diseases, cholesterol levels < 200 mg/dl and age range between 19 and 50 years. All the women were in the menacme. The following risk factors for atherosclerosis were considered: obesity, diabetes mellitus, dyslipidemia, atherosclerosis, systemic arterial hypertension, metabolic syndrome, smoking, osteoporosis and thyroid hormone disorders. After approval of the study by the Committee for Ethics in Research of the institution, and signature of a term of free and informed consent, all the patients were submitted to ultrasonography for evaluation of BAFMD and IMT of carotid and brachial arteries. BAFMD was applied according to the technique described by Celemajer et al. in 1992(11) and modified by Montenegro in 2004(12), by a single observer in all the situations, with the patients in dorsal decubitus, at rest, in a calm environment and under controlled room temperature. There was no food/drug restriction, since the objective of the study was to evaluate the patients’ conditions in their daily habits. The right brachial artery was identified with the aid of a Toshiba Nemio 2D color and spectral Doppler US unit (Toshiba Medical Systems, Tokyo, Japan), equipped with a linear, 14 MHz, high-resolution, B-mode transducer, placed between 2 and 5 cm above the cubital fold. The measurement limited by the intima-lumen interface (D1) at diastole was standardized for measuring the brachial artery diameter. Ischemia was provoked with the sphygmomanometer cuff previously positioned on the patient’s right arm, with 200 mmHg pressure for all the patients during five minutes. A new measurement was performed between 60 and 90 seconds following the compression interruption (D2), at diastole, with the aid of pulsatile Doppler US. The brachial artery flow-mediated dilatation was calculated with the formula (D2 – D1)/D1 Χ 100, and the results were expressed in percentages (Figure 1). The value established by Regattieri et al. (10%) was utilized as a normality parameter(13). 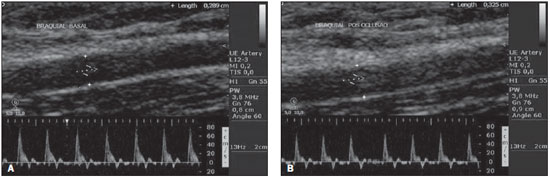 Figure 1. Longitudinal echographic image of brachial artery of a patient with no risk for atherosclerosis, with measurement of the initial diameter of the brachial artery (pre-occlusion) corresponding to 0.8 cm and final to 0.9 mm, with BAFMD value calculated in 12.5%. IMT is defined as the distance between the leading edge of the first echogenic line and the leading edge of the second echogenic line(14). The carotid IMT measurement was performed according to the description proposed by Salonen(15), where the first line represents the intima lumen interface, and the second line represents the carotid media-adventitia interface. In the present study, the evaluation was performed with the transducer placed on the most distal wall of the distal common carotid artery, at 1-2 cm proximal to the carotid bifurcation (Figure 2). The same technique was utilized in the approach of brachial arteries. 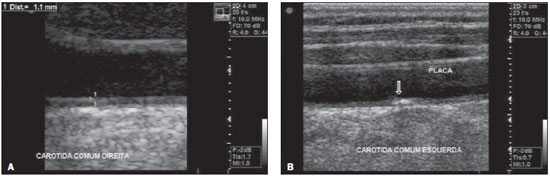 Figure 2. Longitudinal echographic image of right and left common carotid arteries of patients presenting risk for development of atherosclerosis, where thickening (A) and atheromatous plaque (B) could be visualized. The statistical significance threshold was set at p < 0.05, and the Mann-Whitney test of the SPSS package 16.02 for Windows (SPSS Inc.; Chicago, IL, USA) was utilized for statistical processing and analysis of results. Such test is proposed for independent samples, in cases where there is a rupture of parametric assumptions, particularly those regarding normality and homoscedasticity (assumption of constant variance across subsets of data). The results were expressed in mean ± standard deviation. RESULTS The BAFMD was significantly compromised in the group with risk factors as compared with the control group, regardless of sex. In the women with risk factors, BAFMD was 15.2% (± 8.1%) and in the female control group, 25.3% (± 5.4%); p < 0.01. In the men with risk factors BAFMD was 11.8% (± 7.2%), and in the male control group, 16.8% (± 4.2%); p < 0.02. The values observed in the statistical analysis of IMT in both risk and control groups, respectively were the following: for the brachial artery – women, 0.3% (± 0.1%) Χ 0.3% (± 0.1%), p < 0.06; men, 0.36% (± 0.1%) Χ 0.23% (± 0.05%), p < 0.07; for the carotid artery – women, 0.6% (± 0.2%) Χ 0.4% (± 0.1%), p < 0.07; men, 0.85% (± 0.3%) Χ 0.38% (± 0.1%), p < 0.08%, demonstrating that both for the brachial and carotid arteries, the IMTs were not significant. No significant correlation was observed between BAFMD, carotid IMT and brachial IMT among the groups of the present study. DISCUSSION Cerebrovascular and cardiovascular diseases constitute one of the facets of generalized disorder of vascular function, a true “pan-arterial” process. The first phase corresponds to endothelial dysfunction leading to intima-media thickening, with eventual development of atheromatous plaque. A persistent endothelial dysfunction may determine surface instability, erosion of the fibrotic capsule of the plaque, rupture and vascular thrombosis. The identification of changes in the arterial walls of asymptomatic individuals allows a more rigorous management of cardiovascular risk factors in order to prevent a future coronary event. Population and hospital studies utilize noninvasive techniques such as IMT measurement, endothelial dysfunction test and coronary artery calcification study to evaluate premature alterations in the arterial wall structure and function(16). Chequer et al.(17) have reported a significant correlation between BAFMD and intimal-media thickening, that is also an early indicator of atherosclerosis. The present study indicates that patients with risk factors for atherosclerosis present endothelial dysfunction, which has been confirmed by altered BAFMD, and that IMT, both for carotid and brachial arteries were not significantly altered. The endothelial function is affected by chronic conditions such as obesity, diabetes, hypercholesterolemia, smoking and arterial hypertension, and so does, acutely, by sleep deprivation, mental stress, hormonal changes, physical exercises, menstrual cycle and feeding habits. Changes in the vascular reactivity triggered by such conditions can be observed by BAFMD, and also can affect the method reliability. Originally, the measurement of BAFMD was noninvasively performed by ultrasonography, with a cuff positioned on the patient’s arm and later blood flow occlusion that deflagrated reactive hyperemia. Currently, blood flow occlusion in the forearm or wrist has been most frequently utilized, as it seems to express a dilatation promoted exclusively by nitric oxide. With distal occlusion, BAFMD values are lower than those observed with proximal occlusion in the arm (6.8 ± 3.8% Χ 9.8 ± 5.7%, respectively). However, BAFMD reliability seems not to be affected by the site where the cuff is positioned(18). According to Doshi et al.(19), the finding that forearm occlusion results in hyperemia purely mediated by nitric oxide may not by itself justify the abandonment of the technique based on the arm occlusion, because the dilatation promoted by the cuff positioned on the forearm is poor, so the identification of endothelial dysfunction and alterations resulting from changes in feeding habits/physical exercises becomes difficult. A variable that may affect the measurement reliability is the transducer frequency. Herrington et al.(20) have compared the BAFMD stability measured at the line M (media-adventitia interface) and have observed significantly better results in measurements performed with 13 MHz transducers (mean coefficient of variation = 26.3%) than with 7.5 MHz transducers (mean coefficient of variation = 45.3%). Another aspect to be considered is the occlusion time. Leeson et al.(21) have demonstrated that maximal arterial responses can be achieved after 4- to 5-minute occlusion with no additional effect resulting from longer occlusion times. Bots et al.(22) have demonstrated that most studies (~ 51%) have utilized occlusion times > 4.5 minutes. Taking all the variables into consideration, in the present study the authors have opted to evaluate the BAFMD with occlusion of the right arm, utilizing a pressure of 200 mmHg during five minutes and with an US unit equipped with a 14 MHz transducer. The measurement of carotid artery IMT with high-resolution B-mode ultrasonography is a noninvasive method to evaluate the presence of atherosclerosis and disease progression over the years. A good correlation is observed between this measurement and the risk for cardiovascular events. Studies have shown that with an increase of 0.1 mm in carotid IMT, the risk for future myocardial infarction increases in about 10% to 15%, and for stroke in 13% to 18%(23). Isolatedly, the IMT measurement has the same relevance as other most common risk factors, and does not increase the predictive value for cardiovascular events if utilized exclusively for screening purposes(24). Maybe, the absence of significance of the results observed in IMT measurements has occurred because the intima-media thickening is more precociously detected in the subclavian artery than in the carotid arteries, the first one being a more precocious marker for detecting cardiovascular risk than the second one(25). Although the ideal method for diagnosing endothelial dysfunction is still to be established, there are evidences that BAFMD allows an appropriate evaluation of the endothelial behavior and reflects the coronary endothelial function and behavior(26). Training and accurate technique are required for the performance of this methods. The observer must be fully skilled and appropriate equipment is required. Brachial artery flow-mediated dilatation is another useful tool for identifying individuals with cardiovascular diseases and, with the technique standardization, BAFMD tends to become a worldwide accepted method for evaluating endothelial function. The study developed by Meirelles et al.(27) confirms that baseline and post-occlusion diameters and BAFMD measurement by means of manual US technique is highly reliable, allowing its use for endothelial function diagnosis and monitoring. According to Quyyumi(28), markers for systemic inflammation such as BAFMD, carotid IMT and pulsewave analysis have gained popularity as methods for evaluating the risk for atherosclerosis. This author recommends the inclusion of such methods, the biochemical ones included, in randomized studies for screening and diagnosis of cardiovascular risk. CONCLUSIONS BAFMD was an effective criterion to demonstrate endothelial involvement in a population at risk for atherosclerosis. However, this is not valid for IMT of carotid and brachial arteries. REFERENCES 1. Freitas P, Piccinato CE, Martins WP, et al. Aterosclerose carotídea avaliada pelo eco-Doppler: associação com fatores de risco e doenças arteriais sistêmicas. J Vasc Bras. 2008;7:298–307. 2. Brasil. Ministério da Saúde. Sistema de Informações Hospitalares do Sistema Único de Saúde (SIH/SUS). [acessado em 15 de julho de 2010]. Disponível em: http://www.comciencia.br/comciencia/index.php?section=8&edicao=47&id=587 3. Nicolau LGC, Martins WP, Ferreira AC, et al. Avaliação da dilatação máxima da artéria braquial em gestantes e não gestantes, fumantes e não fumantes. Radiol Bras. 2010;43:85–9. 4. Brasil. Ministério da Saúde. Departamento de Ciência e Tecnologia. Secretaria de Ciência, Tecnologia e Insumos Estratégicos. ELSA Brasil: maior estudo epidemiológico da América Latina. Rev Saúde Pública. 2009;43:1–2. 5. Cohn JN. Introduction to surrogate markers. Circulation. 2004;109(25 Suppl 1):iv, 20–1. 6. Bugiardini R, Manfrini O, Pizzi C, et al. Endothelial function predicts future development of coronary artery disease: a study of women with chest pain and normal coronary angiograms. Circulation. 2004;109:2518–23. 7. Naghavi M, Libby P, Falk E, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: Part I. Circulation. 2003;108:1664–72. 8. Castro PT, Montenegro CAB, Carvalho ACP, et al. Dilatação fluxo-mediada da artéria braquial em mulheres com artrite reumatóide. Radiol Bras. 2007;40:247–50. 9. Aminbakhsh A, Mancini GB. Carotid intima-media thickness measurements: what defines an abnormality? A systematic review. Clin Invest Med. 1999;22:149–57. 10. Lorenz MW, von Kegler S, Steinmetz H, et al. Carotid intima-media thickening indicates a higher vascular risk across a wide age range: prospective data from the Carotid Atherosclerosis Progression Study (CAPS). Stroke. 2006;37:87–92. 11. Celermajer DS, Sorensen KE, Gooch VM, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–5. 12. Garrido KU, Rezende Filho J, Leite SP, et al. Dilatação fluxo-mediada da artéria braquial: estudo da função endotelial em mulheres na menopausa. Rev Bras Ecocardiogr. 2008;21:22–6. 13. Regattieri NAT, Leite SP, Koch HA, et al. Dilatação fluxo-mediada da artéria braquial: desenvolvimento da técnica, estudo em pacientes de risco para aterosclerose e em um grupo controle. Rev Bras Ultrason. 2006;9:9–13. 14. Pignoli P, Tremoli E, Poli A, et al. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation. 1986;74:1399–406. 15. Salonen R, Salonen JT. Determinants of carotid intima-media thickness: a population-based ultrasonography study in eastern Finnish men. J Intern Med. 1991;229:225–31. 16. Bots ML, Dijk JM, Oren A, et al. Carotid intima-media thickness, arterial stiffness and risk of cardiovascular disease: current evidence. J Hypertens. 2002;20:2317–25. 17. Chequer G, Nascimento BR, Navarro TP, et al. Espessamento médio-intimal da carótida e função endotelial na doença coronariana. Arq Bras Cardiol. 2006;87:84–90. 18. Mannion TC, Vita JA, Keaney JF Jr, et al. Non-invasive assessment of brachial artery endothelial vasomotor function: the effect of cuff position on level of discomfort and vasomotor responses. Vasc Med. 1998;3:263–7. 19. Doshi SN, Naka KK, Payne N, et al. Flow-mediated dilatation following wrist and upper arm occlusion in humans: the contribution of nitric oxide. Clin Sci (Lond). 2001;101:629–35. 20. Herrington DM, Fan L, Drum M, et al. Brachial flow-mediated vasodilator responses in population-based research: methods, reproducibility and effects of age, gender and baseline diameter. J Cardiovasc Risk. 2001;8:319–28. 21. Leeson P, Thorne S, Donald A, et al. Non-invasive measurement of endothelial function: effect on brachial artery dilatation of graded endothelial dependent and independent stimuli. Heart. 1997;78:22–7. 22. Bots ML, Westerink J, Rabelink TJ, et al. Assessment of flow-mediated vasodilatation (FMD) of the brachial artery: effects of technical aspects of the FMD measurement on the FMD response. Eur Heart J. 2005;26:363–8. 23. Lorenz MW, Markus HS, Bots ML, et al. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–67. 24. Marques DEA, Barra DA, Martins WP, et al. Ultra-sonografia nas lesões ateroscleróticas da carótida. EURP. 2009;1:93–9. 25. Engelhorn CA, Engelhorn AL, Cassou MF, et al. Espessamento médio-intimal na origem da artéria subclávia direita como marcador precoce de risco cardiovascular. Arq Bras Cardiol. 2006;87:609–14. 26. Widlansky ME, Gokce N, Keaney JF Jr, et al. The clinical implications of endothelial dysfunction. J Am Coll Cardiol. 2003;42:1149–60. 27. Meirelles CM, Leite SP, Montenegro CAB, et al. Reliability of brachial artery flow-mediated dilatation measurement using ultrasound. Arq Bras Cardiol. 2007;89:160–7. 28. Quyyumi AA. Inflamed joints and stiff arteries: is rheumatoid arthritis a cardiovascular risk factor? Circulation. 2006;114:1137–9. 1. MD, 33rd Infirmary (Maternity Hospital) of Santa Casa da Misericórdia do Rio de Janeiro, Rio de Janeiro, RJ, Brazil. 2. Full Professor of Radiology at Universidade Federal do Rio de Janeiro (UFRJ), Head of the Unit of Radiology, Santa Casa da Misericórdia do Rio de Janeiro, Rio de Janeiro, RJ, Brazil. 3. Full Professor of Obstetrics at Universidade Federal do Rio de Janeiro (UFRJ), Titular Member of Academia Nacional de Medicina, Rio de Janeiro, RJ, Brazil. 4. Head of the 33rd Infirmary (Maternity Hospital) of Santa Casa da Misericórdia do Rio de Janeiro, Associate Professor of Obstetrics at Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. 5. MD, Vascular Sonographer at Serviço de Cardiologia DASA, Clínica de Ultrassonografia Botafogo and Rede Labs, Rio de Janeiro, RJ, Brazil. 6. MD, 33rd Infirmary (Maternity Hospital) of Santa Casa da Misericórdia do Rio de Janeiro, Associate Professor, Course of Medicine, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. 7. Head of the 33rd Infirmary (Maternity Hospital) of Santa Casa da Misericórdia do Rio de Janeiro, Assistant Professor of Obstetrics at Universidade Gama Filho (UGF), Rio de Janeiro, RJ, Brazil. Mailing Address: Dra. Cristiane Martins Soares 33ª Enfermaria (Maternidade) da Santa Casa da Misericórdia do Rio de Janeiro Rua Santa Luzia, 206, Castelo Rio de Janeiro, RJ, Brazil, 20020-022 E-mail: crismsmed@yahoo.com.br Received July 23, 2010. Accepted after revision September 21, 2010. * Study developed at the 33rd Infirmary (Maternity Hospital) of Santa Casa da Misericórdia do Rio de Janeiro, together with Clínica de Ultrassonografia Botafogo and Department of Radiology – Faculdade de Medicina da Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554