Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 5 - Sep. / Oct. of 2010
Vol. 43 nº 5 - Sep. / Oct. of 2010
|
CASE REPORT
|
|
Morel-Lavallée lesion in the knee: a case report |
|
|
Autho(rs): Eduardo Hennemann Pitrez1; Roberto Campos Pellanda2; Mariana Eltz Silva3; Gustavo Garcia Holz3; Felipe Teixeira Hertz3; João Rubião Hoefel Filho4 |
|
|
Keywords: Knee trauma; Bursitis. |
|
|
Abstract: INTRODUCTION
Shear “degloving” Morell-Lavallée lesions represent a traumatic separation caused by the rapid and violent avulsion of the skin over the underlying fascia, leading the skin to separate from the subcutaneous cellular tissue of the underlying muscular fascia. Such separation implies the rupture of small perforating vessels in this region, resulting in the formation of a cavity that may be filled with blood, lymph and fat foci, the latter being sometimes necrotic(1,2). Morel-Lavallée lesion was originally described in the lateral aspect of the proximal thigh, which is the most common site of this lesion, however other anatomic sites such as periscapular, lumbar and gluteal regions, ankles and knees have been described in the literature(3,4). In the present article, the authors describe a case of Morel-Lavallée lesion affecting the knee of a young patient, evaluated by magnetic resonance imaging (MRI). CASE REPORT A male, 21-year-old patient, victim of a car accident who developed pain and swelling in right knee after the accident. Approximately 40 days after the accident, he was admitted at the university hospital to undergo a MRI study. The MRI study demonstrated a lesion in the deep subcutaneous cellular tissue of the prepatellar region. The lesion was fusiform and encapsulated, with an expansile effect between the subcutaneous tissue and the underlying fascia. The lesion presented with a pseudocapsule, besides some small fat foci inside. High signal intensity in T1- weighted sequences was identified inside the lesion, because of the presence of hematic content (Figure 1). 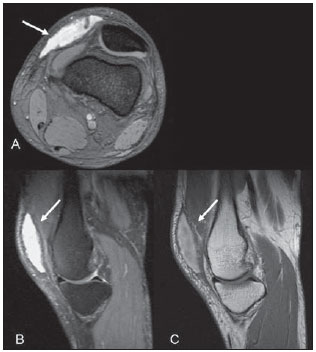 Figure 1. Morel-Lavallée lesion. MRI, axial T2-weighted sequence with fat sat (A) and sagittal T2-weighted sequences with fat sat (B) and T1-weighted sequence (C) demonstrating an encapsulated, fusiform, expansile lesion in the prepatellar region between the subcutaneous cellular tissue and the underlying fascia (arrows). On the T1-weighted image (C), observe the high signal related to hematic content. DISCUSSION This lesion was described by Morel-Lavallée in 1853 and it is a hemolymphatic mass located in the deep subcutaneous cellular tissue, as a consequence of a shearing lesion caused by trauma. Originally described at the external aspect of the thigh, in the last few years it has been recognized and described in other anatomic regions such as the lumbar region and the scapula(1,4). Shearing “degloving” lesions result from a traumatic separation caused by a violent and rapid avulsion of the skin over the fascia, which causes a discontinuity of the deep layer of the conjunctive tissue of the underlying muscular fascia. Such separation causes the disruption of small perforating vessels in this region, resulting in a cavity that may be filled with blood, lymph and sometimes necrotic fat foci(1,2) that may eventually be colonized by infectious agents(5). The development of granulation tissue is observed, and it may organize into a pseudocapsule, leading to the persistence of collections(4). The lesion can be either painful or asymptomatic and up to one third of the patients do not recall any significant trauma(4). Delay in the diagnosis results in the development of collections with bulging and deformity of the subcutaneous cellular tissue(5). Diagnostic delays of up to 34 years have already been described(1,3). These collections may develop rapidly when the arterial bed is involved, or otherwise slowly, in cases of injury to lymphatic vessels(1). Considering that Morel-Lavallée lesions may remain undiagnosed for long periods, it is important for the radiologist to know the characteristics of acute and chronic lesions, as well as their therapeutic implications. The appearance of the lesions depends on the amount of present blood, lymph and fat, as well as the time elapsed from the trauma(4). In the acute phase, blood clots and debris may be found in a hyperintense collection on T2-weighted sequences. With the organization of the hematoma, resulting from the conversion of deoxyhemoglobin into metahemoglobin, such lesions are seen as iso- to hyperintense on T1-weighted images. The lesion periphery becomes hypointense on T1- and T2-weighted images in the course of time, because of the presence of hemosiderin. In the course of time, the collection becomes a T2 hyperintense seroma with a T1 and T2 hypointense pseudocapsule(4). Most frequently, the lesions compromise the lateral aspect of the thigh (Figure 2), involving the great trochanter(6), although lesions in other sites, such as the gluteal, lumbar and scapular regions, the ankles and the knees have already been described(3,4,6). 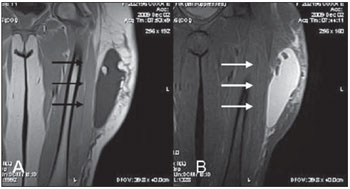 Figure 2. Morel-Lavallée lesion located in its most common site, in a patient with increase of soft tissues on the lateral aspect of the thigh developed after a car accident. MRI, T1-weighted sequence (A) and STIR sequence (B) demonstrating a fluid collection with fat foci within the lesion (arrows). Although Morel-Lavallée lesions occur with a relatively high frequency in the knees, the radiological literature scarcely presents reports on such cases(5,7,8). Tejwani et al. have studied 27 Morel- Lavalée lesions in the knees of 24 athletes over a 13-year period, demonstrating that the main mechanism leading to this lesion was a direct shearing force on the point of collection, and that the most relevant functional deficit was the restriction to flexion, affecting 41% of the patients. The authors have also demonstrated that such athletes returned to their activities even without the complete collections resolution(5). For a long time, the classical treatment comprised surgical drainage with debridement and second-intention healing but, recently, the therapeutic alternatives have tended towards less aggressive treatments(5). Small lesions may be resolved by means of a small incision and drainage, while major lesions may develop a pseudocapsule, becoming refractory to conservative treatment(1). The lesions may also be treated either with elastic compression or liposuction. In cases of failure, sclerosis with the administration of doxycycline is an option(5). The most important differential diagnosis of Morel-Lavallée knee lesions is done with prepatellar bursitis (“housemaid’s knee”). The prepatellar bursa often consists of a trilaminar bursa whose dimensions may extend a little beyond the edges of the patella measuring on average 39 × 40.5 × 3.2 mm in diameter, in the craniocaudal, latero-medial and anteroposterior planes(5). However, in Morel-Lavallée lesions, the collections dimensions and limits often exceed the expected proportions for the prepatellar bursa, this sign being the most reliable in the differentiation between the two entities. Collections extending above the suprapatellar region are virtually diagnostic of Morel-Lavallée, as the bursa should not extend to this point(4,7). Borrero et al. have studied four Morel- Lavallée collections, demonstrating in all the cases a unilocular collection whose limits extended beyond the prepatellar bursa, No blood or fat foci were identified within the collections(4). Tejwani et al. have demonstrated that Morel-Lavallée collections exceeded the expected dimensions of the prepatellar bursa and reported that many of the 27 cases of Morel-Lavallée knee lesions could only be identified by clinical examination; none of these lesions were submitted to biopsy, which maintains the criterion based on dimensions still under argument in the differential diagnosis(4). CONCLUSION Morel-Lavallée collections have been increasingly diagnosed in the knee region, and the radiologist’s knowledge on the characteristics of the lesion at MRI can help in the diagnosis of this disease that is not always recognized, and sometimes difficult to treat. The presence of a trauma history associated with a periarticular collection in the knee should indicate the possibility of a Morel-Lavallée lesion in the differential diagnosis, together with prepatellar bursitis. REFERENCES 1. Gilbert BC, Bui-Mansfield LT, Dejong S. MRI of a Morel-Lavallée lesion. AJR Am J Roentgenol. 2004;182:1347–8. 2. Hak DJ, Olson SA, Matta JM. Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: the Morel-Lavallée lesion. J Trauma. 1997;42:1046–51. 3. Mellado JM, Bencardino JT. Morel-Lavallée lesion: review with emphasis on MR imaging. Magn Reson Imaging Clin N Am. 2005;13:775–82. 4. Borrero CG, Maxwell N, Kavanagh E. MRI findings of prepatellar Morel-Lavallée effusions. Skeletal Radiol. 2008;37:451–5. 5. Tejwani SG, Cohen SB, Bradley JP. Management of Morel-Lavallee lesion of the knee: twentyseven cases in the national football league. Am J Sports Med. 2007;35:1162–7. 6. Moriarty JM, Borrero CG, Kavanagh EC. A rare cause of calf swelling: the Morel-Lavallee lesion. Ir J Med Sci. 2009 Jul 18. [Epub ahead of print]. 7. Ciaschini M, Sundaram M. Radiologic case study. Prepatellar Morel-Lavallée lesion. Orthopedics. 2008;31:626,719–21. 8. Aguiar RO, Viegas FC, Fernandez RY, et al. The prepatellar bursa: cadaveric investigation of regional anatomy with MRI after sonographically guided bursography. AJR Am J Roentgenol. 2007;188:W355–8. 1. PhD, Radiologist at Clínica Radiológica Osório Lopes and at Hospital de Clínicas de Porto Alegre (HCPA), Porto Alegre, RS, Brazil. 2. MD, Radiologist at Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS) and at Hospital de Clínicas de Porto Alegre (HCPA), Porto Alegre, RS, Brazil. 3. MDs., Residents in Radiology at Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil. 4. MD, Radiologist, Head of the Center of Imaging Diagnosis, Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil. Mailing address: Dr. Eduardo Hennemann Pitrez Rua Antenor Lemos, 33, Menino Deus Porto Alegre, RS, Brazil, 90850-100 E-mail: epitrez@terra.com.br Received March 13, 2010 Accepted after revision July 13, 2010 Study developed at Clínica Radiológica Osório Lopes, Porto Alegre, RS, Brazil |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554