Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 6 - Nov. / Dec. of 2007
Vol. 40 nº 6 - Nov. / Dec. of 2007
|
CASE REPORT
|
|
Prostatic rhabdomyosarcoma in an adult patient: a case report |
|
|
Autho(rs): Fábio Abílio Gomes de Almeida, Carlos Leite de Macêdo Filho, Ernesto Lima Araújo Melo, Luciana Mendes de Oliveira Cerri, Giovanni Guido Cerri |
|
|
Keywords: Rhabdomyosarcoma, Prostate, Adult |
|
|
Abstract:
IMDs, Residents in Radiology at Center of Imaging Diagnosis, Hospital Sírio-Libanês, São Paulo, SP, Brazil
INTRODUCTION Prostatic rhabdomyosarcoma is a malignant tumor originating from mesenchymal cells with sarcomatous differentiation(1,2). This disease progresses very fast and aggressively, and is predominantly found in children in whom it corresponds to the main tumor of the prostate(3,4). In adult individuals, this tumor is extremely rare, with only 30 cases described in the English-language literature(4-6). The major series described includes only nine cases(1), demonstrating the lack of accumulated experience on the disease in the worldwide literature. The present study is aimed at describing imaging findings of a case diagnosed in our institution, analyzing them in association with other studies already published in the literature.
CASE REPORT A 27-year-old male patient was admitted with recidivating episodes of pain in the left flank. The clinical hypothesis of urinary lithiasis was considered, and the patient was submitted to computed tomography (CT). The tomographic images (Figure 1) demonstrated a large, solid and heterogeneous prostatic mass, with a predominantly peripheral contrast-enhancement. The lesion extended posterosuperolaterally to the left, involving the left ureter and causing dilatation of the upper caliceal system. After CT examination, the patient was referred for being submitted to ultra-sonography (US)-guided transrectal biopsy, magnetic resonance imaging, and hybrid positron emission tomography/computed tomography (PET/CT) imaging for local and systemic staging.
At transrectal ultrasound (Figure 2) for puncture guidance, a solid, hypoechogenic mass was observed affecting the whole prostate, causing architectural distortion, interruption of the anatomic capsule and infiltration of adjacent planes. The seminal vesicle presented increased in volume because of the tumor infiltration. The anatomopathological and immunohistochemical study showed the presence of an embryonal rhabdomyosarcoma.
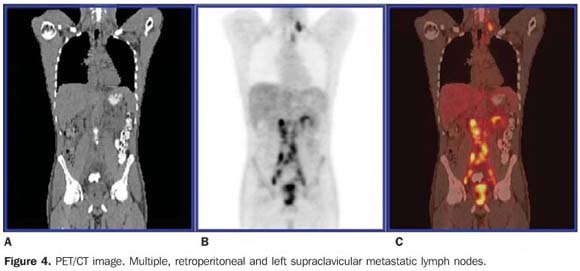
Endorectal coil magnetic resonance imaging (Figure 3) was performed for local staging, demonstrating an ill-defined mass with infiltrative aspect, intermediary signal on T1-, hypersignal on T2-weighted sequences, with intense and heterogeneous gadolinium-enhancement involving the left vasculonervous bundle, left seminal vesicle, and the medial portion of the right seminal vesicle. The lesion presented a contact surface with the vesical wall at the level of the trigone, with a probable involvement of the bladder. PET/CT study (Figure 4) also demonstrated hypermetabolic lesions in left, posterior cervical, left lower paratracheal, left supraclavicular fossa and retroperitoneal lymph nodes extending from the renal hila to the pelvic cavity. Lymph node metastases were confirmed by biopsy of supraclavicular lymph node.
DISCUSSION Malignant prostatic tumors of mesenchymal origin are rare, corresponding to 0.3% to 1.0% of all prostatic tumors. Thirty percent of these tumors are embryonal rhabdomyosarcomas(1). The majority of cases occurs in children, and is difficult to estimate the incidence in adult individuals. Assuming that about 10% of these cases occur in adults, the incidence of adenocarcinomas would be 3000 to 9000 times more frequently in this age range(1). Most of times, the other tumors of sarcomatous origin correspond to leiomyosarcomas, occurring particularly in a more advanced age range and with a much better prognosis(1,2,6,7). Usually, rhabdomyosarcomas presentation is extremely aggressive, being found simultaneously with distant metastases at the moment of the diagnosis in 25% of patients(4). Lungs are the most frequent site, followed by bones, lymph nodes, liver and serosas(1,3,8). Bone metastases are predominantly disseminated osteolytic, in contrast to adenocarcinomas that typically present osteoblastic metastases concentrating especially in the axial skeleton(1). Locally, rhabdomyosarcomas present periuretral, perivesical and perirectal infiltration, displacing the bladder and the rectum(1-3). Histologically, these tumors can be divided into embryonal, alveolar, a quite aggressive subtype predominantly occurring in soft tissues of children; and pleomorphous, a rare and aggressive subtype found in adult individuals(2,9). The embryonal pattern is found in about two thirds of all cases of rhabdomyosarcomas(2), and can be divided into botryoid type, with vegetative growth, most frequently affecting bladder and vaginal cupula; spinous cells and conventional type, with a better prognosis in the first two cases(2,3). Differential histologic diagnosis includes lymphoma and small-cell carcinoma of the prostate and may be resolved by means of an appropriate panel of immunohistochemical stains(4). The most frequent clinical presentation is associated with obstructive urinary symptoms resulting from a significant increase in the prostatic volume. Additionally, hematuria and incontinence may occur. Pelvic pain is a frequent finding, and usually requires rigorous analgesia. Perirectal planes compression or invasion may result in a significant intestinal obstipation(1,3,4,8). Imaging studies are quite scarce, and there is no pattern defining the diagnosis that is confirmed by means of US-guided transrectal biopsy(4,7). However, some findings may suggest the diagnosis, such as the presence of a large mass on the prostatic bed, infiltrating adjacent planes in a young patient who has not presented any increase in the levels of tumor markers or prostate-specific antigen (PSA)(1,7). At ultrasound, the lesion may present predominantly hyper or hypoechogenic, with sonolucent areas corresponding to hemorrhage or necrosis sites(3). The authors could not find any previous report on dopplervelocimetric profile characteristic of the lesion. Reports describe hyperemia and high diastolic flow velocity in paratesticular rhabdomyosarcomas of children(3). In the case presently described, US has also allowed the diagnosis of the tumor extension to the left seminal vesicle, proved by anatomopathological study. CT demonstrates an infiltrative, many times ill-defined mass with heterogeneous attenuation, whose prostatic of vesical site of origin cannot be identified(3,10). At MRI, the primary tumor shows non-specific low signal intensity on T1-weighted sequences, and high sinal intensity on T2-weighted sequences. Heterogeneous signal intensity representing hemorrhagic foci may be identified(3). MRI allows a more accurate evaluation of the local tumor extent and involvement of adjacent planes as compared with US and CT(3,5,11); this could be observed in the present study. The utilization of PET/CT for rhabdomyosarcoma staging in adult individuals is still to be consolidated in the literature, however, reports on cases involving children have demonstrated the relevance of this method in the detection of the primary focus in metastatic disease, obscure metastases and in unusual sites(12). In the present case, PET/CT was extremely useful in the detection of distant lymph node metastases. The treatment of this disease is performed with chemotherapy in association, or not, with surgical resection and/or radiation therapy. The prognosis is poor, with a five-year survival rate of 30%-35% for all rhabdomyosarcomas in adult individuals(6,13); this rate is probably lower in cases of primary tumor on the prostatic bed (1).
CONCLUSION Prostatic rhabdomyosarcoma is much more aggressive, rare, and presents a worst prognosis in adults as compared with its presentation in children. New technologies in imaging diagnosis may aid in the correct diagnosis and also provide an accurate staging of the disease, allowing a better therapeutic planning.
REFERENCES 1. Waring PM, Newland RC. Prostatic embryonal rhabdomyosarcoma in adults. A clinicopathologic review. Cancer 1992;69:755–762. [ ] 2. Nigro KG, MacLennan GT. Rhabdomyosarcoma of the bladder and prostate. J Urol 2005;173:1365. [ ] 3. Agrons GA, Wagner BJ, Lonergan GJ, Dickey GE, Kaufman MS. From the archives of the AFIP. Genitourinary rhabdomyosarcoma in children: radiologic-pathologic correlation. RadioGraphics 1997;17:919–937. [ ] 4. Logani S, Cabrera RA, Amin MB. Embryonal rhabdomyosarcoma of the adult prostate: differential diagnostic considerations. Path Cas Rev 2003;8:82–87. [ ] 5. Hawkins WG, Hoos A, Antonescu CR, et al. Clinicopathologic analysis of patients with adult rhabdomyosarcoma. Cancer 2001;91:794–803. [ ] 6. Ferrari A, Dileo P, Casanova M, et al. Rhabdomyosarcoma in adults. A retrospective analysis of 171 patients treated at a single institution. Cancer 2003;98:571–580. [ ] 7. Sexton WJ, Lance RE, Reyes AO, Pisters PW, Tu SM, Pisters LL. Adult prostate sarcoma: the M.D. Anderson Cancer Center Experience. J Urol 2001;166:521–525. [ ] 8. Bos SD, Slaa ET. An adult man with a rhabdo myosarcoma of the prostate. A case report. Scand J Urol Nephrol 1991;25:329–330. [ ] 9. Miettinen M. Rhabdomyosarcoma in patients older than 40 years of age. Cancer 1988;62:2060–2065. [ ] 10. Baker ME, Silverman PM, Korobkin M. Computed tomography of prostatic and bladder rhabdomyosarcomas. J Comput Assist Tomogr 1985; 9:780–783. [ ] 11. Bartolozzi C, Selli C, Olmastroni M, Menchi I, Di Candio G. Rhabdomyosarcoma of the prostate: MR findings. AJR Am J Roentgenol 1988;150: 1333–1334. [ ] 12. McCarville MB, Christie R, Daw NC, Spunt SL, Kaste SC. PET/CT in the evaluation of childhood sarcomas. AJR Am J Roentgenol 2005;184: 1293–1304. [ ] 13. Little DJ, Ballo MT, Zagars GK, et al. Adult rhabdomyosarcoma: outcome following multimodality treatment. Cancer 2002;95:377–388. [ ]
Received April 11, 2006. Accepted after revision, May 17, 2006.
* Study developed at the Center of Imaging Diagnosis, Hospital Sírio-Libanês, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554