Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 4 - July / Aug. of 2007
Vol. 40 nº 4 - July / Aug. of 2007
|
ICONOGRAPHIC ESSAY
|
|
Iliopsoas compartment lesions: a radiological evaluation |
|
|
Autho(rs): Alberto Ribeiro de Souza Leão, Raquel Portugal Guimarães Amaral, Thiago Giansante Abud, Guilherme Tadeu Sauaia Demarchi, Edison de Oliveira Freire Filho, Paulo Rogério Novack, Flavio do Amaral Campos, José Eduardo Mourão Santos, David Carlos Shigueoka, Artur da Rocha Corrêa Fernandes, Jacob Szejnfeld, Giuseppe D'Ippolito |
|
|
Keywords: Iliopsoas muscle, Psoas muscle, Computed tomography, Abscesses, Neoplasms |
|
|
Abstract:
IPost-graduate Students, Departamento de Diagnóstico por Imagem da Universidade Federal de São Paulo-Escola Paulista de Medicina (Unifesp-EPM), São Paulo, SP, Brazil
INTRODUCTION In the present study, the iliopsoas compartment anatomy aswell as main forms of its involvement will be reviewed toidentify useful signs for potential differential diagnoses. Thespectrum of symptoms in patients with involvement of theiliopsoas compartment is wide and non-specific, resulting indelayed diagnosis in a reasonable number ofcases(1,2). Historically, radiologists havebeen utilized planigraphy, excretory urography, nuclear medicineand ultrasound for detection of diseases affecting the iliopsoascompartment; however, the arrival of computed tomography (CT) wasa landmark in the differentiation of lesions in thissite(3,4). It is important to note that,despite several attempts to define specific signs for determiningthe etiology of lesions in the psoas muscle, the majority ofauthors have identified overlapping features, difficulting thediagnosis in a significant number of cases. However, the presentstudy will try to validate the sensitivity and specificity ofsome radiological findings in an attempt to aid in theetiological differentiation of the lesions to be evaluated. Inthis context, this study presents typical findings of the mostfrequent diseases affecting the iliopsoas compartment,highlighting the signs that could lead to a more specificdiagnosis. The present study includes retrospectively selected imagingstudies performed at Hospital São Paulo at UniversidadeFederal de São Paulo-Escola Paulista de Medicina, inpatients with iliopsoas compartment lesions, whose diagnoses wereconfirmed by means of anatomopathological study or clinicalfollow-up.
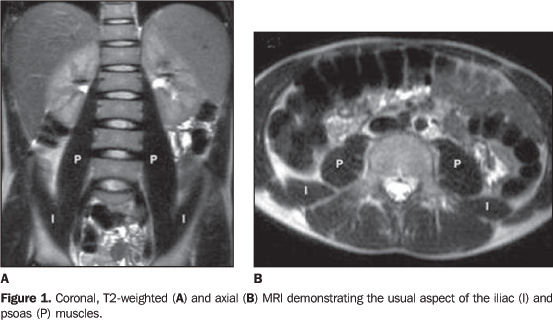
DISCUSSION Anatomy The iliopsoas compartment may be affected by several diseases,including infections, tumors and hemorrhages. The spectrum ofsymptoms in these patients is wide and non-specific, resulting indelayed diagnosis in a significant number ofcases(1). The iliopsoas compartment contains the greater psoas, the smaller psoas, and iliac muscles (Figure 1). The iliac muscle arises from the iliac wing. The greater psoas muscle originates from the transverse process of T12, merging with the iliac muscle at the L5-S2 level to form the iliopsoas muscle. The iliopsoas muscle inserts into the lesser trochanter of the femur. The smaller psoas muscle is located anteriorly to the greater psoas muscle, originating from the T12-L1 vertebral bodies, and inserting into the iliopectineal eminence. All of these muscles are involved by the iliopsoas fascia(1,2). Anteriorly, the iliopsoas fascia is formed by the transversalis fascia, which represents the posterior limit of the retroperitoneum, so defining the iliopsoas compartment, externally and posteriorly located in relation to the retroperitoneum(3,4).
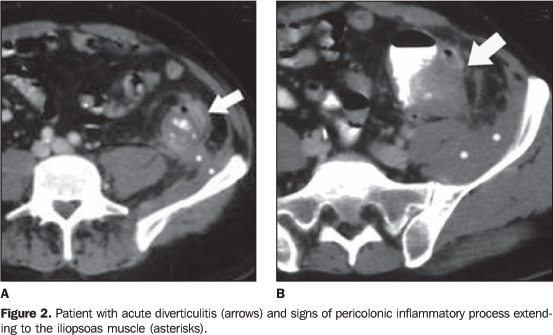
Infection The iliopsoas compartment infectious involvement may be primary or secondary. Primary iliopsoas abscesses are rare and usually idiopathic. Most frequently, Staphylococcus aureus and Gram-negative microorganisms are involved. Immunocompromised patients, and particularly those under corticotherapy, chemotherapy, and those HIV-positive present higher predisposition to infection(1,3). The secondary iliopsoas compartment involvement is even more frequent and usually results from the dissemination of infectious processes from kidneys (perinephric abscesses), bones (osteomyelitis and tuberculosis), and from intestinal loops (appendicitis, diverticulitis, Crohn's disease, perforated colon carcinoma) (Figure 2)(1).
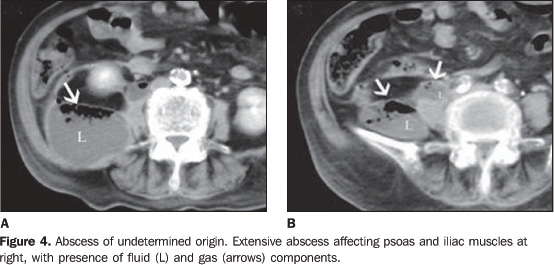
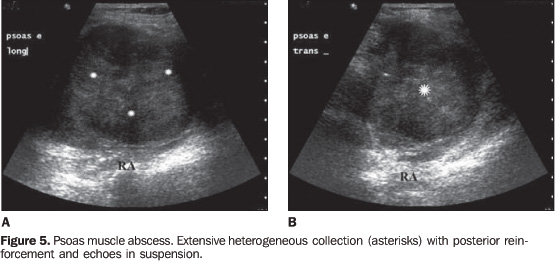
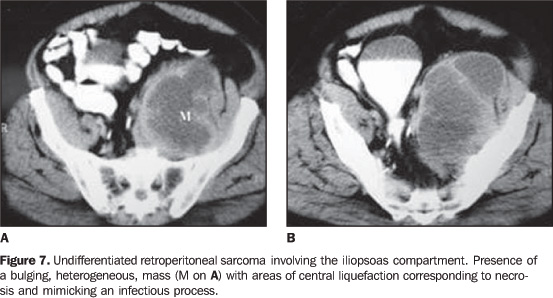
At CT, pyogenic abscesses manifest as lesions of low attenuation, this sign being the most frequent, although non-specific, since it also may be found in neoplasias with significant necrosis and chronic hematomas (Figures 3, 7 and 8)(1). Although the finding of gas bubbles is quite specific of this type of lesion, it is present in only 50% of cases(1–3). In these cases, CT is the most sensitive method for detecting the presence of gas inside the lesion (Figure 4)(1,2). Pyogenic abscesses also present a typical, marginal enhancement after contrast agent injection, observed both on CT and magnetic resonance imaging (MRI) (Figure 3). Obliteration of adjacent fat planes and varied degrees of bone destruction may be found in some cases(2). At ultrasound, these lesions present a poorly specific aspect, as a mass with a heterogeneous contents and fluid/fluid level, highlighting echoes in suspension and debris (Figure 5)(2).
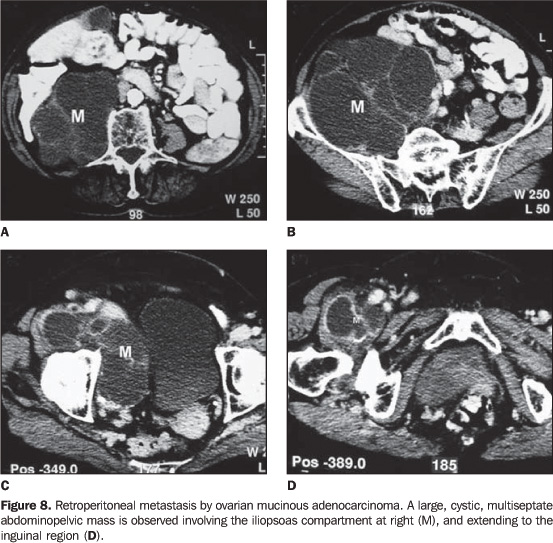
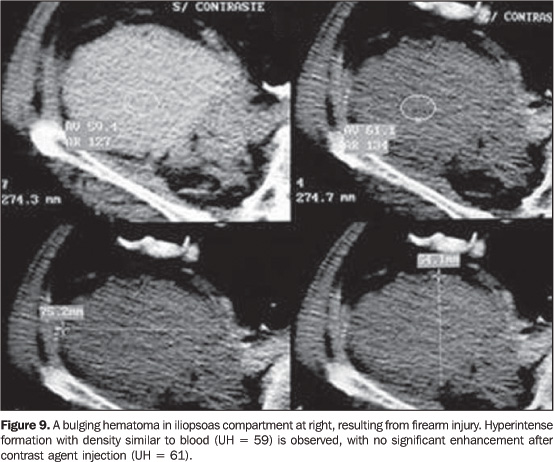
Among infectious processes, tuberculosis was, in the past, the most frequent cause of abscesses involving the spine, paraspinal region and iliopsoas compartment. With the better control of the disease, the pyogenic etiology has become prevalent. However, with the HIV dissemination, there has been a resurgence in tuberculous paraspinal infections, characterized by bone destruction, fluid collections and capsular calcifications (Figure 6)(2). Tumors In most of cases, tumor-like involvement of the iliopsoas is secondary to the direct extension of primary retroperitoneal, abdominal, pelvic, neurogenic, bone tumors, and direct invasion from adjacent lymph nodes(1). In contrast to the inflammatory/infectious involvement, the retroperitoneal fascial planes do not represent any barrier to tumor dissemination, with direct and random invasion(3). On CT and MRI, homogeneous or heterogeneous lesions are observed as a result of the presence of necrosis, hemorrhage and changes in the cellular structure (Figure 7)(3). The most significant findings for differentiation of tumors, abscesses and hematomas, would be the presence of adenopathy, bone destruction and discontinuity of fascial planes(4). Primary iliopsoas tumors are rare, with liposarcoma, fibrosarcoma, leiomyosarcoma and hemangiopericytoma being the typical histological variants found (Figure 7)(1,2). Metastasis to the iliopsoas compartment also is rare, and, most frequently result from hematogenic dissemination from lymphomas, melanomas and uterine cervix, ovary, lung and breast carcinomas (Figure 8)(1,2). The aspect of these lesions is quite overlapping, except for liposarcomas because of the presence of fat component detected at CT or MRI. Hematomas Iliopsoas compartment hematomas may be spontaneous orsecondary to hemorrhagic diathesis, anticoagulant therapy,trauma, tumor, recent surgery or biopsy, or resulting fromextension of bleeding in adjacent organs orvessels(1,2). By correlation between causalfactor and patient's age, it has been possible to observe acloser association with coagulopathies and trauma in a youngerage range (fourth decade of life), and aortic aneurysm ruptureand anticoagulant therapy for arteriosclerotic disease andthromboembolism in an older age range (seventh decade oflife)(3). On CT, acute hemorrhage presents with muscular enlargement and hyperdense contents (usually > 40 UH), unenhanced after contrast agent injection (Figure 9), except in the presence of active bleeding(1,2). In these cases, the involvement tends to be diffuse, fulfilling the whole muscular compartment, this sign being significant for differentiation between processes of infectious and neoplastic origin(4). Fluid/fluid level may be present in subacute and late phases of the disease (Figure 10). Chronic hematomas may be undistinguishable from abscesses and necrotic tumors; and percutaneous aspiration may be necessary for their differentiation (Figure 10)(1,2). On MRI, the hemorrhage aspect depends on the evolutive phase of the disease. In the acute phase, T1-weighted images show a signal intensity similar or slightly lower than that of the muscle; on T2-weighted images, acute hematoma is slightly hyper or hypoattenuating. Subacute hematomas may present up to three different levels of signal intensity on T1-weighted sequences: a low-intensity capsular sign, high-intensity in the peripheral zone, and central isosignal. As the hematoma develops, the central and peripheral signal intensity tend to decrease, on both T1- and T2-weighted sequences(1,2). Chronic hematomas may present with hypointense collections on T1-weighted images and hyperintense on T2-weighted images (Figure 10), simulating other types of collections.
Miscellaneous Retroperitoneal fibrosis, atrophy secondary to paralysis or muscle disease, calcifications secondary to trauma, rhabdomyolysis or foreign body (Figure 11) are other conditions that may involve the iliopsoas muscle(2). In a significant number of cases, radiological findings alonedo not allow to define the etiology of iliopsoas compartmentdiseases. However, their diagnostic accuracy increasessignificantly when evaluated in association with clinical data.Imaging methods also are useful for guiding biopsies and drainageprocedures. The present study was aimed at illustrating imaging findingsof different iliopsoas compartment lesions, to familiarizeradiologists, improving their diagnostic effectiveness and levelof confidence in the evaluation of this muscle compartment.
REFERENCES 1. Muttarak M, Peh WCG. CT of unusual iliopsoas compartment lesions. RadioGraphics 2000;20 (Spec No):S53–66. [ ] 2. Torres GM, Cernigliaro JG, Abbitt PL, et al. Iliopsoas compartment: normal anatomy and pathologic processes. RadioGraphics 1995;15:1285–1297. [ ] 3. Feldberg MA, Koehler PR, van Waes PF. Psoas compartment disease studied by computed tomography. Analysis of 50 cases and subject review. Radiology 1983;148:505–512. [ ] 4. Lenchik L, Dovgan DJ, Kier R. CT of the iliopsoas compartment: value in differentiating tumor, abscess, and hematoma. AJR Am J Roentgenol 1994;162:83–86. [ ]
Received January 17, 2006. Accepted after revision November 16, 2006.
* Study developed in the Departamento de Diagnóstico por Imagem da Universidade Federal de São Paulo-Escola Paulista de Medicina (Unifesp-EPM), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554