Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 2 - Mar. / Apr. of 2007
Vol. 40 nº 2 - Mar. / Apr. of 2007
|
CASE REPORT
|
|
Pancreatic tuberculosis: a case report and literature review |
|
|
Autho(rs): Henrique Pereira Faria, José Torres Alves, Ovídio Carlos Carneiro Villela, Raul Moraes da França Filho, Milton Alves Romeiro |
|
|
Keywords: Tuberculosis, Pancreas, Computed tomography |
|
|
Abstract:
IMD, Trainee at Setor de Radiologia e Diagnóstico por Imagem do Hospital Márcio Cunha, Ipatinga, MG, and at Centro de Pesquisa e Pós-graduação da Faculdade de Ciências Médicas de Minas Gerais (CPG-FCMMG), Belo Horizonte, MG, Brazil
INTRODUCTION Tuberculosis is a common disease, but the pancreas involvementrarely occurs. The first cases were reported by Auerbach in1944(1). Pancreatic tuberculosis pathogenesis is still to be known. Ithas been suggested that bacilli reach the pancreas bylympho-hematogenic dissemination from primary or secondarytuberculosis. The primary lesion may be intestinal, withpancreatic involvement originating from retroperitoneal lymphnodes(2). Clinical features are quite variable,many times mimicking characteristics of a pancreaticadenocarcinoma(3). This paper presents a case of pancreatic tuberculosis in a39-year-old male patient manifesting pain in the superior abdomenand constitutional symptoms. The radiological workup and clinicalmanifestations are discussed.
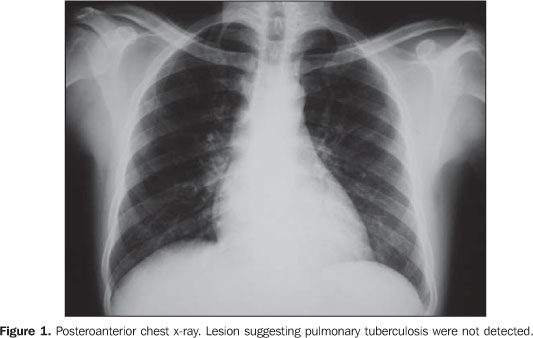
CASE REPORT Male, 39-year-old patient with previous history of alcoholism,reported intermittent epigastric pain for approximately thelatest 45 days, associated with nausea, vomiting and body weightloss. There was no history of pulmonary or gastrointestinaltuberculosis in the past. Clinical signs at physical examination were normal. Total leukocyte counting was 2,700/mm³, with the following differential counting: segmented 63%, rods 22%, lymphocytes 9% and monocytes 6%; hemoglobin de 9.3 g/dl. No alteration was found on upper digestive endoscopy. Normal chest x-ray (Figure 1). During the hospital stay, the patient progressed with febrile peaks predominantly at evening.
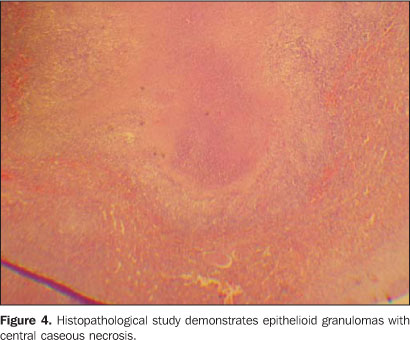
Computed tomography was requested and demonstrated hypodense lesions in the pancreatic tail and spleen (Figure 2A), with enhancement after venous contrast injection (Figure 2B). Exploratory laparotomy revealed multiple whitish nodules in the pancreas, spleen and omentum (Figure 3). The hypothesis of peritoneal carcinomatosis was raised, and omentectomy, splenectomy and hygienization of the peripancreatic area. The histopathological study of the spleen and omentum demonstrated several epithelioid granulomas with central caseous necrosis (Figure 4), associated with few Langhans-type and foreign-body-type giant multinucleated cells. The Ziehl-Nielsen staining for acid-fast bacilli was positive.
DISCUSSION The pancreas is rarely affected by tuberculosis. In 1944,Auerbach reported pancreatic involvement in 4.7% of biopsies incases of miliary tuberculosis(4). Between 1891and 1961, Paraf et al.(3) reported 11 cases ofpancreatic involvement in necropsies of miliary tuberculosis,with 2.1% incidence of involvement of this organ. Between 1980 and 1998, 14 cases were reported in theliterature(5), the majority in young adults(mean age 33 years), with constitutional symptoms and epigastricpain. In eight cases, only the pancreas was affected. Thediagnosis was made by means of laparotomy in seven cases. Fineneedle aspiration biopsy was performed in six cases, two of themunder computed tomography guidance. The cytology suggestedtuberculosis in four cases. Therefore, fine needle aspirationbiopsy is recommended in the suspicion of pancreatic tuberculosisand differential diagnosis with pancreatictumor(6,7). Of then cases with tuberculinictest, eight were positive. This is a simple and low-cost testthat may be useful as a support for the clinical rationale inthese cases. The diagnosis of pancreatic tuberculosis frequently may bedisregarded or postponed, unless there is an evidence ofpulmonary tuberculosis in another site. However, of the 14 casesin the literature(5), eight did not presentextrapancreatic lesions, and only three presented involvement ofthe lungs. Pancreatic tuberculosis may present several signs andsymptoms, including pain in the upper abdomen, obstructivejaundice mimicking a tumor in the pancreatic head, fever ofundetermined origin, and non-specific symptoms like body-weightloss. The majority of cases presented constitutional symptoms andpain in the upper abdomen(5).
CONCLUSION The diagnosis of pancreatic tuberculosis requires a high levelof suspicion and, although is a rare condition, should beconsidered as a differential diagnosis in patients withpancreatic lesions, particularly those with constitutionalsymptoms. The tuberculinic test may be of diagnostic value inthese cases. However, CT-guided fine needle aspiration emerges asa propedeutic method of choice because of its low-invasivenessand reasonable specificity.
REFERENCES 1. Watanapa P, Vathanopas V. Tuberculous pancreatic abscess: a rare condition mimicking carcinoma. HPB Surg 1992;5:209–213. [ ] 2. Lo SF, Ahchong AK, Tang CN, Yip AW. Pancreatic tuberculosis: case reports and review of the literature. J R Coll Surg Edinb 1998;43:65–68. [ ] 3. Paraf A, Menanger C, Texier J. La tuberculose du pancreas et la tuberculose des ganglions de l'etage superieur de l'abdomen. Rev Med Chir Mal Foie 1996;41:101–126. [ ] 4. Auerbach O. Acute generalized miliary tuberculosis. Am J Pathol 1944;20:121–136. [ ] 5. Ahmad Z, Bhargava R, Pandey DK, Sharma DK. Pancreatic tuberculosis – a case report. Ind J Tuberc 2003;50:221–223. [ ] 6. Ali RAR, Azfar M, Al-Jarallah M. Isolated pancreatic tuberculosis – a case report. Kuw Med J 2004;36:290–292. [ ] 7. Riaz AA, Singh A, Robshaw P, Isla AM. Tuberculosis of the pancreas diagnosed with needle aspiration. Scand J Infect Dis 2002;34:303–304. [ ]
Received April 25, 2005.
* Study developed in the Setor de Radiologia e Diagnóstico por Imagem do Hospital Márcio Cunha, Ipatinga, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554