Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 5 - Sep. / Oct. of 2008
Vol. 41 nº 5 - Sep. / Oct. of 2008
|
ORIGINAL ARTICLE
|
|
The role of the unenhanced phase in the routine abdominal computed tomography |
|
|
Autho(rs): Ana Paula Klautau Leite, Leandro Accardo de Mattos, Gustavo Alfredo Duarte Henriques Pinto, Andrea Puchnick Scaciota, Rita Maria Aparecida Monteiro Moura Franco, Cássio Andreoni, Henrique Manoel Lederman, Giuseppe D'Ippolito |
|
|
Keywords: Computed tomography, Contrast media, Abdomen |
|
|
Abstract:
IMD, Resident, Department of Imaging Diagnosis, Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM), São Paulo, SP, Brazil
INTRODUCTION Because of the technological developments in the area of diagnostic methods, computed tomography (CT) has increasingly been utilized in the assessment of abdominal diseases. The advent of multislice technology resulted in an even higher increase in the utilization of this diagnostic tool(1,2). Currently, there is a wide range of specific protocols utilizing abdominal CT in the presence of determined clinical suspicions(3-9). On the other hand, there is a considerable group of patients submitted to abdominal CT scans without a clearly pre-established diagnostic hypothesis, such as those presenting with a clinical picture consisting only of fever of undetermined etiology or unexplained ponderal loss, among other specific clinical situations, and, when submitted to abdominal CT scan, are assessed by means of a generic protocol, like those undergoing tumors staging. It seems that there is a consensus in the literature (especially in the North-American one) that the unenhanced phase would be unnecessary in this group of patients(4,5). However, in our environment, these patients are routinely submitted to an unenhanced phase preceding the intravenous contrast-enhanced phases. The utilization of this protocol has implications related to radiation dose, images acquisition time, and x-ray tube power consumption, and it only would be justified if indispensable, supplementary information were added, affecting the management and prognosis of the patient. In some clinical circumstances, such as study of urolithiasis, hepatic steatosis, hemochromatosis/hemosiderosis or evaluation of renal or adrenal nodules and masses, the unenhanced phase has demonstrated an unquestionable usefulness(6,10-13). In other situations, the validity of this type of diagnostic approach is still to be evidenced. After an extensive literature review, we could not identify any study evaluating the value of the unenhanced phase preceding intravenous contrast-enhanced phases in abdominal CT scans for patients with an undefined clinical picture or undergoing tumors staging/restaging. For this reason, the authors have decided to evaluate the role of the unenhanced phase in abdominal CT scans for these patients.
MATERIALS AND METHODS In the period between March and June 2007, the authors developed a prospective, transversal, observational study aimed at evaluating the added value of the unenhanced phase in abdominal CT, with 100 patients (56 men and 44 women) with mean age of 55.23 ± 15.38 years. The present study encompassing two phases was approved by the Committee for Ethics in Research of Universidade Federal de São Paulo/Escola Paulista de Medicina, and developed in the Unit of Computed Tomography of the Department of Imaging Diagnosis at Hospital São Paulo. Phase 1 With the objective of establishing possible changes in the diagnosis as a result of findings at abdominal CT with and without the unenhanced phase, 100 consecutive patients were evaluated. The inclusion criterion was indication for unenhanced and contrast-enhanced CT according to the protocol adopted by the Unit. Patients with indication for unenhanced CT(6) (for example, urolithiasis study), contraindication to contrast agents, as well as patients undergoing investigation for adrenal(12) nodule/mass, renal(10) nod-ule/mass, hepatic steatosis(11), hemochromatosis and hemosiderosis(13) were excluded, considering the recognized necessity of the unenhanced phase for the diagnosis of these diseases. All the studies were performed in a helical Tomoscan AV CT equipment (Philips Medical Systems; Best, The Netherlands), following the study protocol included in the manual of routine procedures of the Unit of Computed Tomography at Hospital São Paulo - Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM), São Paulo, SP, Brazil. Contiguous, axial slices with 3-7 mm reconstruction interval, pitch ranging between 1 and 1.5, before and after intravenous injection of hydrosoluble iodinated contrast agent by means of an infusion pump in a dose ranging between 1.5 and 2.0 ml/kg at a rate of 3-4 ml/s. After the contrast injection, images were acquired in the arterial (corticomedullary), portal (or nephrographic) and equilibrium (or pyelographic) phases, depending on the clinical indication. Oral or rectal administration of contrast agents was performed as indicated. All the images were independently analyzed on an EasyVision workstation (Philips Medical System; Best, The Netherlands) by two radiologists with two-year experience in abdominal CT whose analyses were based on the clinical indication, initially only for the contrast-enhanced phase (first analysis), and subsequently combining the findings of both pre- and post-contrast phases (second analysis). Previously, the observers had access to the data included in the requests from the patients' doctors and, in the first and second analyses, classified the tomographic diagnoses into primary and secondary according to their priority and clinical significance for the patient. At the end of each evaluation, both observers determined if there was a change in primary and secondary diagnoses between the first and second analyses, i.e., if the interpretation based on the combined analysis of the unenhanced and contrast-enhanced phases had affected the diagnosis, as compared with the analysis only of the contrast-enhanced phase(s). In cases of disagreement, a third observer established if there was, or not, a change in the diagnosis between the first and second analyses. Phase 2 In this phase, only the cases with changes in the primary and secondary diagnoses between the first and second analyses were considered. Two experienced specialists, with over 10 years of practice, were selected according to the type of diagnosis (for example: gastroenterologist and urologist for indicating the approach to be adopted in cases of hepatic steatosis and urolithiasis), and invited to participate in the study for establishing if these changes would imply changes in the clinical approach to these patients. So, the specialists established an approach based on clinical/laboratory data and on the diagnosis originated in the first tomographic analysis, and subsequently based on the diagnosis modified (or supplemented) by the second tomographic analysis. Statistical analysis Data were tabulated on an Excel XP® (Microsoft) worksheet and the software SPSS 11.5 for Windows® (SPSS Inc.; Chicago, USA) was utilized in the data analysis. The frequency of changes in the primary and secondary diagnoses was evaluated in the phase 1 of the present study, upon comparison between the first and second analyses. In the second phase of the study, the authors measured the frequency of changes in the clinical approach established by the specialists based on the tomographic diagnosis resulting from the first and second analyses. The Chi-square test was utilized for statistical analysis, considering p < 0.05 as statistically significant.
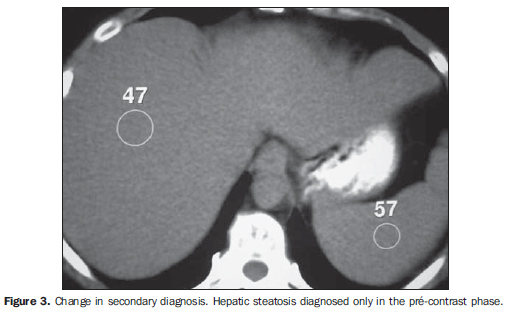
RESULTS Phase 1 Consensual primary diagnoses achieved by the radiologists were: acute abdomen (4%), abdominal neoplasm (65%), inflammatory-infectious process (8%), nephrolithiasis (2%), adrenal nodule (2%), hepatic nodule (3%) and others (16%). Only one (1%) of the 100 patients had the diagnosis changed after the reading of the unenhanced phase (second analysis) as compared with the reading of the contrast-enhanced phase (first analysis) and without statistical significance ( p = 1.000). This patient, with an operated colon neoplasm and undergoing tumor restaging, presented an adrenal nodule initially considered as indeterminate that, after the measurement of the unenhanced density (second analysis), was diagnosed as an adenoma (Figure 1). Eighteen (18%) of the 100 patients had their secondary diagnosis modified, although without statistical significance (p = 0.143), as follows: steatosis (7%), adrenal nodule (1%), nephrolithiasis (7%), renal cysts (2%) and hepatic calcifications without perfusional alterations (1%) (Figures 2, 3, 4 and 5).
Among the cases included in the present study, the diagnosis could be reached in the first analysis (i.e., without the necessity of the contrast-enhanced phase) in nine patients with steatosis, six with nephrolithiasis and one with adrenal adenoma (Figures 6, 7 and 8). Phase 2 Among the 19 patients who had their primary (one) or secondary (18) diagnoses modified in the second analysis, 11 presented urinary system alterations (for example, renal cysts, nephrolithiasis, adrenal adenomas), and eight alterations in the digestive system (for example, steatosis, hepatic calcification). For this reason, an urologist and a gastroenterologist were invited for analyzing these cases and defining the approach to be adopted. Five (62%) of the eight patients assessed by the gastroenterologist had their final therapeutic approach modified. In four patients diagnosed with steatosis only by the unenhanced phase, the specialist opted for investigating the cause for steatosis. In the case of a young patient undergoing tumor restaging without any tomographic sign of recidivation and with cholelithiasis identified only on the unenhanced phase (Figure 5), the specialist opted for indicating cholecystectomy. In the other three patients, the conduct was not modified because of their primary diagnosis and clinical progression. In two of the 11 patients evaluated by the urologist, the clinical approach remained unchanged. These two patients presented adrenal incidentalomas and would be submitted to laboratory tests, independently from the tomographic definition of the lesion nature. For the other nine patients (81.8%), seven of them with nephrolithiasis and two with renal cysts classified as Bosniak II and IIF according to the second analysis, the specialist proposed a treatment for those with renal calculi and evolutive follow-up for the two patients with renal cysts. The utilization of the unenhanced phase was statistically significant (p = 0.038) by the chi-square test applied to the cases where the conduct was changed.
DISCUSSION Technological developments incorporated into CT equipment in the last years, especially after the advent of the helical and, most recently, multislice technologies, have resulted not only in an increase in the utilization of this diagnostic method, but also in the complexity of some protocols for abdominal studies utilizing multiple contrastation phases(14,15). These multi-phase protocols reduce the tube lifetime and increase the amount of radiation absorbed by the patient(2). Numberless studies have been developed, with the most different strategies to reduce the radiation dose in abdominal CT studies(16-18). Among these strategies, the suppression of some of the study phases seems to be a practical and safe measure, provided the diagnostic reliability of the study is guaranteed(3). For this reason the present study was developed, considering that there is no evidence in the literature that, with the adoption of a protocol for abdominal CT without the utilization of the unenhanced phase, the same diagnostic efficiency is maintained for patients without a clear diagnosis hypothesis or those undergoing tumor staging or restaging. In the unit of CT of a university hospital where the present study was developed, there are several protocols specifically designed for determined diagnostic suspicions. Among these protocols, the authors adopted a generic one designed for cases where there is no defined clinical hypothesis (for example: fever of undetermined etiology or unexplained ponderal loss) or requiring tumor staging or restaging. In this generic protocol, the investigation is divided into three phases: a first, unenhanced phase, a second, performed 70 seconds after the contrast injection is initiated (portal phase), and a third phase acquired between three and five minutes after the contrast injection (equilibrium phase). The present study was aimed at establishing whether the unenhanced phase was really necessary in this group or could be suppressed, so reducing the radiation dose absorbed by the patient and increasing the x-ray tube lifetime. The evaluation of the necessity or not of the unenhanced phase was based on the frequency of changes in the primary and secondary diagnoses originated only by the contrast-enhanced phase (first analysis) and from the combined analysis of the unenhanced and contrast-enhanced phases (second analysis) performed by two independent observers. Primary diagnosis was that either directly related to the clinical condition or justifying the clinical picture of the patient. Secondary diagnosis was the one that had not met the criteria for primary diagnosis according to the subjective view of the observers. For the purposes of the present study, the sample included patients who did not present a defined clinical suspicion or diagnosis of diseases where the unenhanced phase was particularly useful, such as urolithiasis, hepatic steatosis, hemochromatosis, renal and adrenal nodules which were considered as exclusion criteria. The study was developed in two phases to measure not only the frequency of changes in diagnoses, but also their impact on the clinical approach to the patient from the point of view of the two observers. The primary diagnosis was changed in the second analysis in only one of the 100 cases, demonstrating that the unenhanced phase is not very useful in diagnostic terms. The patient in question underwent tomographic examination for a colon neoplasm staging. The initial diagnosis (after the first analysis) indicated only the presence of an indeterminate adrenal nodule (relative wash-out < 50%) (Figure 1) and that could be of secondary nature. The final diagnosis (after the second analysis) demonstrated the presence of an adenoma because of the low density observed in the unenhanced phase(12). The other findings were normal according to both observers and there was no evidence of metastatic dissemination to other organs. Despite the significance of this diagnostic change for the patient's prognosis, it is important to take some aspects into consideration. Metastases to the adrenal gland are common in cases of a variety of primary neoplasms, among them thyroid, renal, stomach, colon, pancreatic, esophageal neoplasms and melanomas. But, although frequent, many adrenal nodules in cancer patients are benign. Even among patients with lung carcinoma, 30% of adrenal nodules are not metastatic(19,20). Additionally, after a literature review, the authors have not found any case of patients with colon carcinoma and single metastasis to the adrenal. In these cases, the disease is generally disseminated to other organs, which has not been observed in the mentioned patient. Amongst the 100 cases evaluated, the 18 patients who had their secondary diagnoses modified presented steatosis, nephrolithiasis, adrenal nodules, renal cysts and hepatic calcifications without perfusional alterations. The seven cases of steatosis presented a mild form of fat infiltration, with density in the unenhanced phase measuring less than 10 Hounsfield units below the spleen density(21). It is interesting to observe that in nine patients with the most advanced stages of steatosis the diagnosis could be achieved in the contrast-enhanced phase (first analysis), and confirmed in the second analysis. Two patients presented renal cysts initially classified as simple (Bosniak I) and that the unenhanced phase evaluation demonstrated to be cysts without hyperdense contents or with septa, and reclassified as Bosniak II or IIF. Type II cysts do not require follow-up and therefore would not be responsible for changes in the clinical approach. On the contrary, cysts classified as IIF, because of their risk, although a low risk, of growth and malignization, undergo follow-up(22). One patient presented a hepatic punctiform calcification, with no associated perfusional alteration and identified only in the second analysis. It is important to note that this type of calcification has no pathological meaning and is frequently found in asymptomatic patients(23). One patient had an indeterminate adrenal nodule identified in the contrast-enhanced phase, and considered as compatible with adenoma because of the level of density observed in the unenhanced phase (second analysis). In these cases, when the contrast-enhanced phase does not allow an accurate diagnosis, it is recommended that the patient is recalled for a new evaluation by means of a unenhanced phase, therefore without any direct clinical impact, but just with a certain discomfort for the patient who must return to the unit of CT for undergoing a further CT scan(12). In seven patients, renal calculi were identified, six of them non-obstructive, and the majority with < 6 mm in diameter and found in asymptomatic patients(24,25). The absence of symptoms and the presence of small, non-obstructive calculi seem to represent favorable signs for indicating an expectative approach(26). Amongst the cases presented to the gastroenterologist, the changes in the diagnosis were associated to steatosis, cholelithiasis and hepatic calcifications without perfusional alterations. The specialist evaluated all the diagnoses of mild steatosis, indicating an investigation of the possible causes. Hepatic steatosis is frequently found in patients with chronic infection by hepatitis B and C viruses. Studies in the literature have demonstrated that steatosis is associated with a rapid progression of the hepatic fibrosis and a poor response to the antiviral therapy in hepatitis C patients(27,28). A precise measurement of the hepatic parenchyma attenuation coefficients is essential for determining a patient's eligibility for a living-donor transplant. In this group of patients, the unenhanced phase is indispensable for the acquisition of these measurements(21,29). These patients were not included in the present study, and in these cases the evaluation with only contrast-enhanced phase would not be indicated. In only one among the cases presented to the urologist there was no change in the clinical approach, because the diagnosis of adrenal nodule would indicate the necessity of hormonal evaluation independently from the nodule nature, considering the fact that it was diagnosed in a patient with no history of a known neoplasm. In cases of non-obstructive and asymptomatic nephrolithiasis, the urologist offered the patient the option for getting the calculus removed by means of flexible ureteroscopy or follow-up only, depending on the patient's personal characteristics and lifestyle(30). In the two patients with complex cysts, the specialist opted for following them up by means of magnetic resonance imaging (MRI). CT follow-up has shown to be an effective form of management of patients with moderately complex renal cysts(22), and CT and MRI demonstrate similar findings in the majority of renal cysts(31). However in some cases, MRI demonstrated additional findings such as parietal thickening or septa, determining a change in the Bosniak classification and for this reason this imaging method has been utilized in the follow-up of these patients(31). Radiation exposure represents a relevant factor to be taken into consideration in abdominal CT studies. Although there is no defined value for maximum radiation dose to which a patient could be exposed, and there is a consensus that this patient should receive the dose required for the diagnosis, it would be desirable that this dose was as lowest as possible(32). The dose utilized for each phase of multislice abdominal CT is about 12 to 20 mSv(33). This would be the mean radiation dose reduction obtained upon suppression of one of the tomographic phases. The present study has some limitations. The number of patients could be higher, and the authors are engaged in the development of a study with a larger sample for validating the findings of the present study. However, in the authors' opinion, remarkable changes should not be observed in these results. It was difficult to define the criteria for patients selection, considering that many presented with incomplete clinical histories or confused diagnosis hypotheses on their CT study requests. In a future study, it is the authors' intention to restrict the sample only to patients undergoing tumors staging or restaging. In the present study, the definition of the primary and secondary diagnoses was quite subjective, but the authors could not classify the tomographic findings in a more precise fashion. Finally, the authors could observe that the unenhanced phase has not provided significant changes in the primary diagnoses for patients in the clinical context approached by the present study. The secondary diagnoses altered by the reading of the unenhanced phase were also not quantitatively significant, but those initially considered as secondary were significantly valorized by the specialists in the respective diseases. From the author's point of view, it still remains unclear if the unenhanced phase should be abolished in routine computed tomography for patients without a definite diagnosis or undergoing tumor staging.
REFERENCES 1. Broder J, Warshauer DM. Increasing utilization of computed tomography in the adult emergency department, 2000-2005. Emerg Radiol. 2006;13:25-30. [ ] 2. Wiest PW, Locken JA, Heintz PH, et al. CT scanning: a major source of radiation exposure. Semin Ultrasound CT MR. 2002;23:402-10. [ ] 3. Iannaccone R, Laghi A, Catalano C, et al. Hepatocellular carcinoma: role of unenhanced and delayed phase multi-detector row helical CT in patients with cirrhosis. Radiology. 2005;234:460-7. [ ] 4. Zeman RK, Baron RL, Jeffrey RB Jr, et al. Helical body CT: evolution of scanning protocols. AJR Am J Roentgenol. 1998;170:1427-38. [ ] 5. Urban BA, Fishman EK. Tailored helical CT evaluation of acute abdomen. Radiographics. 2000;20:725-49. [ ] 6. Smith RC, Verga M, McCarthy S, et al. Diagnosis of acute flank pain: value of unenhanced helical CT. AJR Am J Roentgenol. 1996;166:97-101. [ ] 7. Galvão Filho MM, D'Ippolito G, Hartmann LG, et al. O valor da tomografia computadorizada helicoidal sem contraste na avaliação de pacientes com dor no flanco. Radiol Bras. 2001;34:129-34. [ ] 8. D'Ippolito G, Mello GGN, Szejnfeld J. The value of unenhanced CT in the diagnosis of acute appendicitis. São Paulo Med J. 1998;116:1838-45. [ ] 9. D'Ippolito G, Nunes Jr JAT, Wolosker AMB, et al. O valor da tomografia computadorizada sem contraste na avaliação da região cecoapendicular normal. Radiol Bras. 1996;29:247-51. [ ] 10. Bosniak MA. The current radiological approach to renal cysts. Radiology. 1986;158:1-10. [ ] 11. Limanond P, Raman SS, Lassman C, et al. Macrovesicular hepatic steatosis in living related liver donors: correlation between CT and histologic findings. Radiology. 2004;230:276-80. [ ] 12. Korobkin M, Brodeur FJ, Francis IR, et al. CT time-attenuation washout curves of adrenal adenomas and nonadenomas. AJR Am J Roentgenol. 1998;170:747-52. [ ] 13. Fritz GA, Schoellnast H, Deutschmann HA, et al. Density histogram analysis of unenhanced hepatic computed tomography in patients with diffuse liver diseases. J Comput Assist Tomogr. 2006;30:201-5. [ ] 14. Liu WY, Jin Y, Rong RH, et al. Multi-phase helical CT in diagnosis of early hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2003;2:73-6. [ ] 15. Huang QJ, Xu Q, Wang XN, et al. Spiral multi-phase CT in evaluating resectability of pancreatic carcinoma. Hepatobiliary Pancreat Dis Int. 2002;1:614-9. [ ] 16. Kim BS, Hwang IK, Choi YW, et al. Low-dose and standard-dose unenhanced helical computed tomography for the assessment of acute renal colic: prospective comparative study. Acta Radiol. 2005;46:756-63. [ ] 17. Funama Y, Awai K, Miyazaki O, et al. Improvement of low-contrast detectability in low-dose hepatic multidetector computed tomography using a novel adaptive filter: evaluation with a computer-simulated liver including tumors. Invest Radiol. 2006;41:1-7. [ ] 18. Meagher T, Sukumar VP, Collingwood J, et al. Low dose computed tomography in suspected acute renal colic. Clin Radiol. 2001;56:873-6. [ ] 19. Silverman SG, Mueller PR, Pinkney LP, et al. Predictive value of image-guided adrenal biopsy: analysis of results of 101 biopsies. Radiology. 1993;187:715-8. [ ] 20. Harisinghani MG, Maher MM, Hahn PF, et al. Predictive value of benign percutaneous adrenal biopsies in oncology patients. Clin Radiol. 2002;57:898-901. [ ] 21. Lee SW, Park SH, Kim KW, et al. Unenhanced CT for assessment of macrovesicular hepatic steatosis in living liver donors: comparison of visual grading with liver attenuation index. Radiology. 2007;244:479-85. [ ] 22. Israel GM, Bosniak MA. Follow-up CT of moderately complex cystic lesions of the kidney (Bosniak category IIF). AJR Am J Roentgenol. 2003;181:627-33. [ ] 23. Bezerra ASA, D'Ippolito G, Martelli P, et al. Calcificações hepáticas: freqüência e significado. Radiol Bras. 2003;36:199-205. [ ] 24. El-Nahas AR, El-Assmy AM, Madbouly K, et al. Predictors of clinical significance of residual fragments after extracorporeal shockwave lithotripsy for renal stones. J Endourol. 2006;20:870-4. [ ] 25. Nadler RB, Stern JA, Kimm S, et al. Coronal imaging to assess urinary tract stone size. J Urol. 2004;172:962-4. [ ] 26. Parsons JK, Lancini V, Shetye K, et al. Urinary stone size: comparison of abdominal plain radiography and noncontrast CT measurements. J Endourol. 2003;17:725-8. [ ] 27. Caturelli E, Castellano L, Fusilli S, et al. Coarse nodular US pattern in hepatic cirrhosis: risk for hepatocellular carcinoma. Radiology. 2003;226:691-7. [ ] 28. Colli A, Fraquelli M, Andreoletti M, et al. Severe liver fibrosis or cirrhosis: accuracy of US for detection - analysis of 300 cases. Radiology. 2003;227:89-94. [ ] 29. Brancatelli G. Science to practice: should biopsy be performed in potential liver donors when unenhanced CT shows an unacceptable degree of steatosis for transplantation? Radiology. 2006;239:1-2. [ ] 30. Elashry OM, Elbahnasy AM, Rao GS, et al. Flexible ureteroscopy: Washington University experience with the 9.3F and 7.5F flexible ureteroscopes. J Urol. 1997;157:2074-80. [ ] 31. Israel GM, Hindman N, Bosniak MA. Evaluation of cystic renal masses: comparison of CT and MR imaging by using the Bosniak classification system. Radiology. 2004;231:365-71. [ ] 32. D'Ippolito G, Medeiros RB. Exames radiológicos na gestação. Radiol Bras. 2005;38:447-50. [ ] 33. MacKersie AB, Lane MJ, Gerhardt RT, et al. Nontraumatic acute abdominal pain: unenhanced helical CT compared with three-view acute abdominal series. Radiology. 2005;237:114-22. [ ] Received September 4, 2007. Accepted after revision November 29, 2007. * Study developed in the Department of Imaging Diagnosis at Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554