Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 6 - Nov. / Dec. of 2009
Vol. 42 nº 6 - Nov. / Dec. of 2009
|
REVIEW ARTICLE
|
|
Pelvic ultrasonography in children and teenagers |
|
|
Autho(rs): Wellington de Paula Martins, Stael Porto Leite, Carolina Oliveira Nastri |
|
|
Keywords: Ultrasonography, Early puberty, Ovary |
|
|
Abstract:
IPhD, Associate Professor at Escola de Ultrassonografia de Ribeirão Preto (EURP), Assistant Physician at Department of Gynecology and Obstetrics of Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil
INTRODUCTION The knowledge on developmental changes that take place in the female pelvis during puberty is essential in the investigation of pelvic conditions in children and teenagers. Imaging methods can facilitate the achievement of a correct diagnosis, and ultrasonography is the method of choice in such cases(1). The prepubertal uterus is thin, with the uterine body similar in size to the cervix. Because of the hormone stimulation that takes place in the puberty, the uterus grows and the uterine body becomes prominent. The ovaries can be identified at ultrasonography at either age. Generally, the ovarian volume increases after the age of six years and small follicles can be normally seen during the whole childhood. In children and teenagers, ultrasonography is routinely performed through abdominal approach, utilizing the liquid within the bladder as a sonographic window. Considering that the presence of gas in the bowel hinders the propagation of sound waves, a full bladder moves the bowel loops up, allowing a better visualization of the pelvic organs. Color Doppler ultrasonography allows a rapid identification of abnormal vessels and vascular structures. In sexually active teenagers, the study may be complemented with the transvaginal approach. Additionally, as a better image resolution is required or in cases where the abdominal approach does not provide sufficient information, the rectal approach is a good alternative provided it is performed by an experienced sonographer. Main indications for pelvic ultrasonography in children and teenagers are the following: either early or late puberty, pelvic pain or tumor, ambiguous genitalia, vaginal bleeding in children, and primary amenorrhea. Prepubertal vaginal bleeding may indicate the presence of a foreign body, precocious puberty or vaginal rhabdomyosarcoma. The most common causes of primary amenorrhea in teenagers include: gonadal dysgenesis (Turner's syndrome) and Müllerian abnormalities (uterine/vaginal malformations). Pelvic pain or tumors in children and teenagers may be caused by ovarian torsion, hemorrhagic ovarian cyst, pelvic inflammatory disease or ectopic pregnancy.
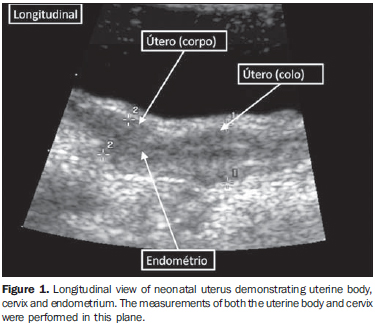
UTERUS AND OVARIES In female neonates, the uterus is increased due to the influence of maternal and placental hormones(2,3). The uterine body is larger than the uterine cervix, the uterine length is approximately 3.5 cm, and the maximum thickness is approximately 1.4 cm. Generally, the endometrium is visible and echogenic (Figure 1). A small amount of fluid may be present within the endometrial cavity in approximately 25% of neonatal uteri. In neonates, the ovarian volume is slightly larger than in the childhood (on average, 1 cm3 at the first year as compared with 0.6767 cm3 at the second year of life)(4). The presence of ovarian follicles (< 1 cm) is routinely detected in 84% of neonates up to the second year of life, and in 68% of children between two and six years of age(5).
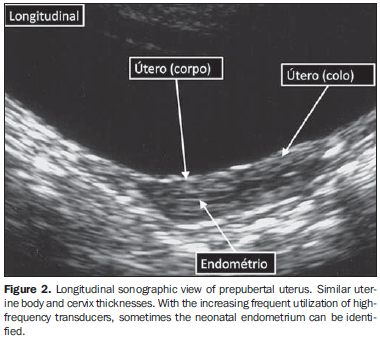
Before the puberty, in the age range between two and six years, the size and morphology of the uterus and ovaries remain relatively stable: the volume of each ovary is < 2 cm3, with follicles < 9 mm, the uterine length if < 4 cm, and the width and thickness of the uterine body and cervix generally are < 1 cm. The prepubertal uterus is a tubular structure (uterine cervix = uterine body), but sometimes the uterine cervix thickness may be larger than the uterine body(6,7). Typically the endometrium is not apparent, but in some cases it can by visualized with the utilization of high-frequency transducers (Figure 2). From the practical point of view, the following values may be adopted as parameters for prepubertal girls: maximum uterine length < 4.5 cm, uterine thickness < 1 cm and ovarian volume < 3 cm3(8).
A recent study evaluating the utilization of pelvic ultrasonography for differentiating children with precocious puberty from children with early pubarche, thelarche, or normal puberty also has shown that this is a good diagnostic method(9). The uterine length and volume, besides the ovarian volume, have played a relevant role in the differentiation of girls with precocious puberty from those with normal puberty. The uterine body/cervix ratio considered by many as a good method, has also presented a good performance although inferior to the performance of the first ones. However, this study has not evaluated separately the uterine thickness, probably the most reproducible one, considering the best limits definition(10). On the other hand, during the measurement of the uterine length, it may be difficult to differentiate the external uterine orifice from the vagina, while the width limits may be ill-defined due to the similarity between the uterine and tube/ligaments echogenicity. From the beginning of puberty, (around the age of six to nine years) there is a progressive growth of uterus and ovaries. The uterine body becomes wider and thicker than the uterine body, assuming the piriform shape observed in adult women, with an increase in the uterine body/cervix ratio from 1/2 to values between 2/1 and 3/1(8). Generally, the uterine length ranges between 5 and 8 cm, the width is about 3.5 cm, and the thickness, between 1.5 and 3 cm. The endometrium can be easily identified, with thickness and echographic appearance varying according to the phase of the menstrual cycle. The ovaries assume a more ovoid shape and volume > 4 cm3 as a response to the gonadotropins stimulus. The Doppler study of uterine arteries may be utilized as a complementary tool in the puberty follow-up(11). Such arteries may be evaluated on a cross-sectional view of the uterus near the uterine body. In prepubertal girls, the systolic flow is seen as a narrow spectral wave, there is no Doppler signal during the diastolic period, and high pulsatility index (PI): mean 6.27, ranging from 3.5 to 8. Typically, early in the puberty a non-continuous Doppler signal is observed at diastole with decreased PI: mean 3.7, ranging from 2.5 to 5. On the other hand, late in the puberty, the Doppler spectrum corresponds to a broader systolic wave with continuous Doppler signal at diastole and PI , 3: mean 2.06, ranging from 1.1 to 2.96. However, uterine and ovarian arterial flow measured by Doppler is less useful than uterine and ovarian volume to differentiate children with precocious puberty from those with normal puberty(12).
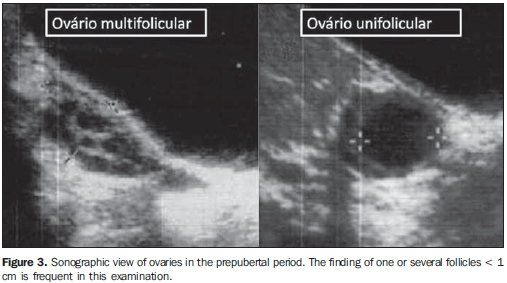
ECHOGRAPHIC EVALUATION OF HORMONAL INFLUENCE IN GIRLS Estrogen stimulation Echographic findings suggesting estrogen stimulation are the following: uterine thickness and volume, uterine body thickening (uterine body thicker than cervix or uterine body/cervix ratio > 1) and apparent endometrium. The ovary appearance is less useful because of a certain overlapping of measurements along the childhood between prepubertal and pubertal girls, besides the fact that the presence of follicles does not indicate precocious puberty, since follicles with < 1 cm in diameter may be observed in the prepubertal period (Figure 3)(6,13). Ultrasonography has been considered to be useful in the differentiation between premature thelarche and central precocious puberty, as an adjuvant to LH level measurement, according to a recent consensus on the use of GnRH antagonists in children(14). The main markers reported by such consensus were the following: apparent endometrium, that is highly specific (about 100% specificity), although with a not so good sensitivity (about 30-80%)(15); uterine length > 3.0-4.0 cm (depending on the age); and ovarian volume > 1.0 to 1.5 cm3, with sensitivity and specificity around 90%(9,10,16,17). Table 1 is a summary of the main cut-offs utilized in the diagnosis of precocious puberty according to the age.
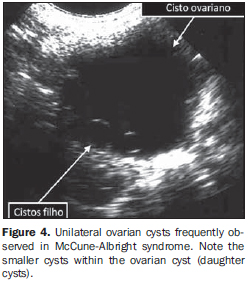
Precocious puberty is defined as complete sexual development (including menarche) before the age of eight years, and may be classified into central and peripheral. Central precocious puberty (true precocious puberty) is gonadotropins-dependent and, in about two thirds of cases is idiopathic. Some tumors of the central nervous system or increase in the intracranial pressure may lead to central precocious puberty. Uterine and ovarian growth may be demonstrated at ultrasonography before the changes in the LH and FSH secretary patterns as compared with GnRH tests can be observed(16). As the echographic follow-up is performed during the treatment with GnRH agonists, a decrease in the uterine and ovarian volume can be demonstrated up to values found in prepubertal children with the same age(18,19). Peripheral precocious puberty (pseudoprecocious puberty is not gonadotropin-dependent. McCune-Albright syndrome is characterized by café-au-lait spots, fibrous dysplasia and peripheral precocious puberty. Follicular cysts with autonomous production of estradiol represent the most frequent cause of peripheral precocious puberty, and the children present high estradiol serum levels and low FSH and LH levels. In such cases, the GnRH test result is negative. The most frequent echographic findings are: uterus characteristic of estrogenic stimulus and unilateral follicular ovarian cyst(20,21), that may present with smaller follicular cysts (daughter cysts) inside (Figure 4)(22). Spontaneous symptoms regression and disappearance of the ovarian cyst at echography may occur. Follicular ovarian cysts with autonomous estrogenic production are most frequently found than estrogenic ovarian tumors, such as granulose cell tumors or gonadoblastomas.
Isolated premature adrenarche and isolated premature thelarche These children present echographic findings of the pelvis (uterine body/cervix ratio, uterine length and thickness and ovarian volume) with values similar to the ones observed in prepubertal children with the same age.(13,16)
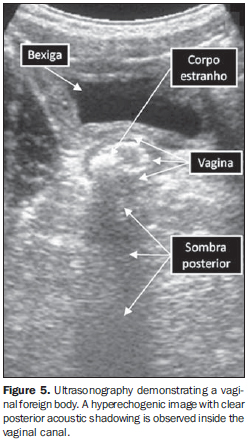
ECHOGRAPHIC EVALUATION OF VAGINAL BLEEDING IN PREPUBERTAL CHILDREN Vaginal bleeding in prepubertal children may occur because of the presence of a foreign body inside the vagina, precocious puberty or vaginal rhabdomyosarcoma. Hemangiomas and other vascular malformations also may cause vaginal bleeding in these children. Foreign body in the vagina Foreign bodies in the vagina are seen in 18% of children with vaginal bleeding and discharge and in 50% of children with vaginal bleeding and without discharge(8). A vaginal foreign body may be identified through echogenic imaging, the presence of posterior acoustic shadowing being frequently observed (Figure 5)(23).
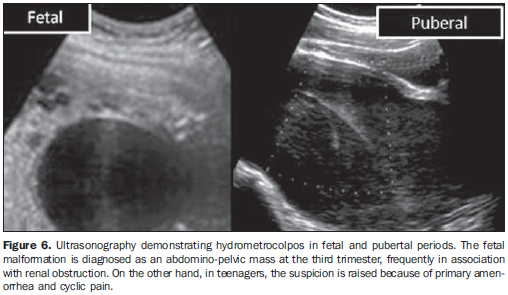
Vaginal rhabdomyosarcoma Vaginal rhabdomyosarcomas are almost exclusively found in very young children. The echographic aspect of these tumors corresponds to large solid, heterogeneous or hypoechoic nodules located posteriorly to the bladder. Five-year survival in cases of genital rhabdomyosarcomas without metastasis is of approximately 90%(24-26). Primary amenorrhea in teenagers Primary amenorrhea is defined in one of the following three situations: absence of menarche at 16 years of age, absence of thelarche or adrenarche at 14 years of age, absence of menarche within three years from adrenarche or thelarche. The presence or absence of secondary sexual characteristics at clinical examination and identification of the uterus at echography constitute the initial steps taken before starting an investigation by means of laboratory tests. Common causes of primary amenorrhea include ovarian failure (for example, Turner's syndrome - 48.5% of cases), uterine-vaginal malformations (Müllerian anomalies - 16.2% of cases), dysfunction of the hypothalamic-hypophyseal-ovarian axis (8.3% of cases), constitutional or familial delay (6% of cases). Other less common causes, such as malnutrition, psychiatric disorders, and infections are responsible for 21% of cases(27). Turner's syndrome Girls with 45 X0 karyotype (approximately 70% of cases) will present prepubertal uterus and ovaries unidentifiable at ultrasonography or inactive ovaries(28,29). In rare cases, particularly those where a mosaic-type karyotype is present, the ovaries may present a normal echographic appear-ance(30). Spontaneous puberty may occur in up to 20% of cases(31). Uterine-vaginal malformations (Müllerian anomalies) Paramesonephric ducts (Müllerian ducts) develop between the 5th and 6th gestational weeks. At about the 8th gestational week they fuse to form the uterovaginal canal. During this fusion, the uterovaginal canal reaches the urogenital sinus at the same time that the vaginal plate is formed at the lower end of the utero-vaginal canal. Thus, the vagina is formed both by the paramesonephric ducts (upper 2/3 or 4/5) and the urogenital sinus(32). Müllerian agenesis (Mayer-Rokitansky-Kuster-Hauser syndrome) is the second most common cause of primary female infertility (the first one is gonadal dysgenesis)(33). Echographically, this syndrome is characterized by vaginal atresia associated with either absence of the uterus or rudimentary uterus and normal ovaries. Renal malformations (agenesis, ectopia) occur in up to 50% of cases, and bone malformations in up 12% of cases. Among these women, 6-10% may present with immaturely formed uterus and functional endometrium, possibly with the development of hematometrium. Obstructive malformations In most of cases, congenital hydrometrocolpos is associated with malformation of the urogenital sinus. Utero-vaginal obstructions may be identified early during the fetal life, in the third trimester, as an abdomino-pelvic mass (Figure 6). Frequently, renal obstruction is associated. Teenagers with obstructive anomalies typically present primary amenorrhea and cyclic abdominal pain. In such cases, ultrasonography is useful for differentiating cases of hematometrocolpos secondary to imperforate hymen or transverse vaginal septum from hematometrium due to cervical agenesis(34). The differentiation between such cases plays a significant role in the definition of the prognosis, since hematometrocolpos is resolved after desobstruction, while, because of the cervical agenesis, hematometrium generally is managed by means of hysterectomy.
Approximately 45% of vaginal septa are found in the upper vaginal third, 40% in the middle third, and only 15% in the lower third(35). The presence of obstructed hemivagina with uterine duplication, Herlyn-Werner-Wunderlich syndrome, is almost always associated with ipsilateral renal agenesis(36). At clinical examination, cyclic abdominal pain caused by the obstruction is concomitantly present with regular menstrual cycles, which generally may delay a correct diagnosis. Complete vaginal obstruction must be urgently treated because of the risk for endometriosis and impairment of the reproductive capacity. Non-obstructive malformations The main non-obstructive malformations result from failure in the paramesonephric ducts fusion or resorption, leading to septate, bicornuate, unicornuate uteri and didelphia. Two-dimensional ultrasonography may suspect of the defect type, which can be better evaluated by three-dimensional ultrasonography(37).
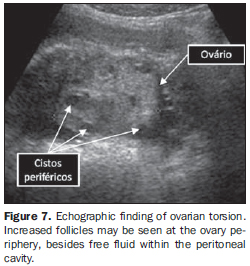
ULTRASONOGRAPHY: PELVIC MASS AND PAIN Ultrasonography is the initial modality in the evaluation of children and teenagers with pelvic pain. Ovarian torsion and tumors Ovarian torsion is most common in patients with predisposing factors such as ovarian cysts or masses(38). In children, ovarian torsion may be due to the fact of the uterine tube being relatively longer and the ovary more mobile. The main cause for a normal ovary torsion is the excessive ovarian mobility in the infant pelvis. The twisted ovary presents multiple, peripheral increased follicles (Figure 7)(39). Color Doppler is not a reliable method for evaluating ovarian torsion. The peripheral and/ or central arterial flow may be demonstrated at Doppler ultrasonography in cases of surgically proved ovarian torsion, which may be explained by the doubleness of the ovarian vascularization. Because of the late diagnosis, since pelvic pain is rarely investigated in children with the required rapidity, few twisted ovaries may be saved during surgery.
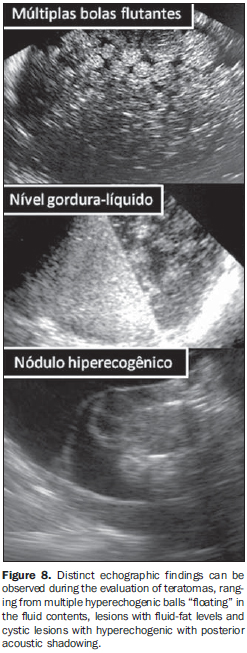
Ovarian tumors in children primarily occur because of the presence of functional cysts (follicular - 60%) and neoplasms (40%). Two thirds of neoplasms are benign (frequently teratomas), while one third is malignant. At ultrasonography, teratomas present different characteristics (Figure 8), so the diagnosis may be difficult. The histological analysis of malignant ovarian tumors reveals a prevalence of 60-75% of germ cell tumors, epithelial tumors in 10%20% of cases, and stromal tumors in 10%(38,40). In children and teenagers, ovarian teratomas may lead to torsion in about 30% of cases, and 10% are bilateral. Ultrasonography demonstrates wall nodules in 55% of cases and echogenic foci with posterior shadowing in 44% of cases. Some echographic findings such as ascites, peritoneal implants, lymphadenopathies or hepatic metastasis may suggest the presence of malignancy. The echographic characteristics of the lesion do not suggest malignancy, which makes the diagnosis more difficult.
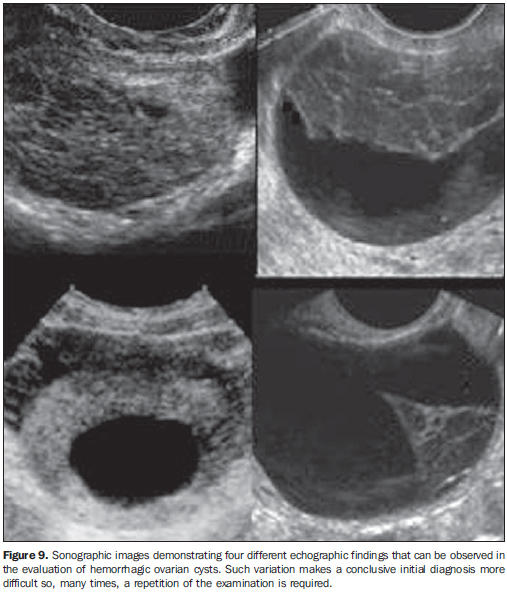
Hemorrhagic ovarian cysts Acute pelvic pain at the middle of the menstrual cycle is clinically suggestive of hemorrhage resulting from ovulation that occurs during the corpus luteum formation. Ultrasonography demonstrates a complex ovarian mass with posterior acoustic shadowing because of the liquid contents, frequently associated with the presence of free fluid in the vaginal pouch fundus. However, the echographic appearance of such cysts is quite variable (Figure 9). Along the echographic follow-up, such cysts become anechoic in most of cases(41).
Pelvic inflammatory disease Pelvic inflammatory disease or tube-ovarian abscess are found in sexually active teenagers and may be recognized through clinical findings (pelvic pain, fever, pain at cervical mobilization, adnexal rigidity). Ultrasonography is useful for detecting complications such as tubo-ovarian abscesses, hydrosalpinx and pyosalpynx. Ectopic pregnancy The incidence of ectopic pregnancy is very low among teenagers, but, in this age range it presents highest mortality rates(8). Like in adults, the diagnosis must be based on the presence of any adnexal mass associated with a positive pregnancy test.
FINAL CONSIDERATIONS Ultrasonography has demonstrated to be the modality of choice in the initial evaluation of the female pelvis in the childhood and adolescence, a situation where the clinical examination is very limited, since the vaginal approach is unfeasible and many times clinicians do not feel comfortable adopting the rectal approach. Such examination may provide valuable information on the patient's pelvis, allowing the definition and planning of clinical and surgical treatments. In these cases, a specific knowledge of the changes in the female pelvis during the childhood and puberty is essential to avoid inaccurate diagnosis.
REFERENCES 1. Ziereisen F, Guissard G, Damry N, et al. Sonographic imaging of the paediatric female pelvis. Eur Radiol. 2005;15:1296-309. [ ] 2. Nussbaum AR, Sanders RC, Jones MD. Neonatal uterine morphology as seen on real-time US. Radiology. 1986;160:641-3. [ ] 3. Hata K, Nishigaki A, Makihara K, et al. Ultrasonic evaluation of the normal uterus in the neonate. J Perinat Med. 1989;17:313-7. [ ] 4. Cohen HL, Shapiro MA, Mandel FS, et al. Normal ovaries in neonates and infants: a sonographic study of 77 patients 1 day to 24 months old. AJR Am J Roentgenol. 1993;160:583-6. [ ] 5. Cohen HL, Eisenberg P, Mandel F, et al. Ovarian cysts are common in premenarchal girls: a sonographic study of 101 children 2-12 years old. AJR Am J Roentgenol. 1992;159:89-91. [ ] 6. Holm K, Laursen EM, Brocks V, et al. Pubertal maturation of the internal genitalia: an ultrasound evaluation of 166 healthy girls. Ultrasound Obstet Gynecol. 1995;6:175-81. [ ] 7. Orbak Z, Sağsöz N, Alp H, et al. Pelvic ultrasound measurements in normal girls: relation to puberty and sex hormone concentration. J Pediatr Endocrinol Metab. 1998;11:525-30. [ ] 8. Garel L, Dubois J, Grignon A, et al. US of the pediatric female pelvis: a clinical perspective. Radiographics. 2001;21:1393-407. [ ] 9. Badouraki M, Christoforidis A, Economou I, et al. Evaluation of pelvic ultrasonography in the diagnosis and differentiation of various forms of sexual precocity in girls. Ultrasound Obstet Gynecol. 2008;32:819-27. [ ] 10. Martins WP, Nastri CO. Ultrasonographic measurement of ovarian volume in the diagnosis of central precocious puberty. Ultrasound Obstet Gynecol. 2009;34:484-5. [ ] 11. Ziereisen F, Heinrichs C, Dufour D, et al. The role of Doppler evaluation of the uterine artery in girls around puberty. Pediatr Radiol. 2001;31:712-9. [ ] 12. Golestani R, Sheikhvatan M, Behpour AM, et al. Relationship between uterine and ovarian arterial blood flow measured by Doppler sonography at different stages of puberty. Taiwan J Obstet Gynecol. 2008;47:62-5. [ ] 13. Buzi F, Pilotta A, Dordoni D, et al. Pelvic ultrasonography in normal girls and in girls with pubertal precocity. Acta Paediatr. 1998;87:1138-45. [ ] 14. Carel JC, Eugster EA, Rogol A, et al. Consensus statement on the use of gonadotropin-releasing hormone analogs in children. Pediatrics. 2009; 123:e752-62. [ ] 15. de Vries L, Horev G, Schwartz M, et al. Ultrasonographic and clinical parameters for early differentiation between precocious puberty and premature thelarche. Eur J Endocrinol. 2006;154:891-8. [ ] 16. Haber HP, Wollmann HA, Ranke MB. Pelvic ultrasonography: early differentiation between isolated premature thelarche and central precocious puberty. Eur J Pediatr. 1995;154:182-6. [ ] 17. Herter LD, Golendziner E, Flores JA, et al. Ovarian and uterine findings in pelvic sonography: comparison between prepubertal girls, girls with isolated thelarche, and girls with central precocious puberty. J Ultrasound Med. 2002;21:1237-46; quiz 1247-8. [ ] 18. Ambrosino MM, Hernanz-Schulman M, Genieser NB, et al. Monitoring of girls undergoing medical therapy for isosexual precocious puberty. J Ultrasound Med. 1994;13:501-8. [ ] 19. Jensen AM, Brocks V, Holm K, et al. Central precocious puberty in girls: internal genitalia before, during, and after treatment with long-acting gonadotropin-releasing hormone analogues. J Pediatr. 1998;132:105-8. [ ] 20. Rodriguez-Macias KA, Thibaud E, Houang M, et al. Follow up of precocious pseudopuberty associated with isolated ovarian follicular cysts. Arch Dis Child. 1999;81:53-6. [ ] 21. Fakhry J, Khoury A, Kotval PS, et al. Sonography of autonomous follicular ovarian cysts in precocious pseudopuberty. J Ultrasound Med. 1988;7:597-603. [ ] 22. Lee HJ, Woo SK, Kim JS, et al. "Daughter cyst" sign: a sonographic finding of ovarian cyst in neonates, infants, and young children. AJR Am J Roentgenol. 2000;174:1013-5. [ ] 23. Caspi B, Zalel Y, Katz Z, et al. The role of sonography in the detection of vaginal foreign bodies in young girls: the bladder indentation sign. Pediatr Radiol. 1995;25 Suppl 1:S60-1. [ ] 24. Martelli H, Oberlin O, Rey A, et al. Conservative treatment for girls with nonmetastatic rhabdomyosarcoma of the genital tract: a report from the Study Committee of the International Society of Pediatric Oncology. J Clin Oncol. 1999;17:2117-22. [ ] 25. Andrassy RJ, Wiener ES, Raney RB, et al. Progress in the surgical management of vaginal rhabdomyosarcoma: a 25-year review from the Intergroup Rhabdomyosarcoma Study Group. J Pediatr Surg. 1999;34:731-4; discussion 734-5. [ ] 26. Castellino SM, McLean TW. Pediatric genitourinary tumors. Curr Opin Oncol. 2007;19:248-53. [ ] 27. Timmreck LS, Reindollar RH. Contemporary issues in primary amenorrhea. Obstet Gynecol Clin North Am. 2003;30:287-302. [ ] 28. Morgan T. Turner syndrome: diagnosis and management. Am Fam Physician. 2007;76:405-10. [ ] 29. Haber HP, Ranke MB. Pelvic ultrasonography in Turner syndrome: standards for uterine and ovarian volume. J Ultrasound Med. 1999;18:271-6. [ ] 30. Mazzanti L, Nizzoli G, Tassinari D, et al. Spontaneous growth and pubertal development in Turner's syndrome with different karyotypes. Acta Paediatr. 1994;83:299-304. [ ] 31. Massa G, Heinrichs C, Verlinde S, et al. Late or delayed induced or spontaneous puberty in girls with Turner syndrome treated with growth hormone does not affect final height. J Clin Endocrinol Metab. 2003;88:4168-74. [ ] 32. Gell JS. Müllerian anomalies. Semin Reprod Med. 2003;21:375-88. [ ] 33. Chandiramani M, Gardiner CA, Padfield CJ, et al. Mayer-Rokitansky-Kuster-Hauser syndrome. J Obstet Gynaecol. 2006;26:603-6. [ ] 34. Blask AR, Sanders RC, Rock JA. Obstructed uterovaginal anomalies: demonstration with sonography. Part II. Teenagers. Radiology. 1991; 179:84-8. [ ] 35. Rackow BW, Arici A. Reproductive performance of women with müllerian anomalies. Curr Opin Obstet Gynecol. 2007;19:229-37. [ ] 36. Orazi C, Lucchetti MC, Schingo PM, et al. Herlyn-Werner-Wunderlich syndrome: uterus didelphys, blind hemivagina and ipsilateral renal agenesis. Sonographic and MR findings in 11 cases. Pediatr Radiol. 2007;37:657-65. [ ] 37. Ferreira AC, Mauad Filho F, Nicolau LG, et al. Ultra-sonografia tridimensional em ginecologia: malformações uterinas. Radiol Bras. 2007;40:131-6. [ ] 38. Schultz KA, Ness KK, Nagarajan R, et al. Adnexal masses in infancy and childhood. Clin Obstet Gynecol. 2006;49:464-79. [ ] 39. Breech LL, Hillard PJ. Adnexal torsion in pediatric and adolescent girls. Curr Opin Obstet Gynecol. 2005;17:483-9. [ ] 40. Gribbon M, Ein SH, Mancer K. Pediatric malignant ovarian tumors: a 43-year review. J Pediatr Surg. 1992;27:480-4. [ ] 41. Swire MN, Castro-Aragon I, Levine D. Various sonographic appearances of the hemorrhagic corpus luteum cyst. Ultrasound Q. 2004;20:45-58. [ ] Received June 13, 2009. * Study developed at Escola de Ultrassonografia de Ribeirão Preto (EURP) and at Department of Gynecology and Obstetrics of Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554