Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 6 - Nov. / Dec. of 2009
Vol. 42 nº 6 - Nov. / Dec. of 2009
|
ORIGINAL ARTICLE
|
|
Subungual glomus tumors: imaging findings |
|
|
Autho(rs): Cristiano Montandon, Juliana da Cunha Costa, Lorena Andrade Dias, Fernando Henrique Abrão Alves da Costa, Ana Carolina Mendes da Costa, Renato Tavares Daher, Marcelo Eustáquio Montandon Jr |
|
|
Keywords: Subungual glomus tumors, Magnetic resonance imaging, Ultrasonography |
|
|
Abstract:
IMDs, Radiologists, Clínica da Imagem and Clínica Multimagem Diagnósticos, Titular Members of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR) and Sociedade Goiana de Radiologia, Goiânia, GO, Brazil
INTRODUCTION Glomus bodies are highly specialized arteriovenous anastomoses responsible for the thermoregulation by regulating the skin blood flow. These bodies can be found in the reticular layer of the dermis throughout the body although they are most numerous in digits, hand palms and feet soles(1). Glomus tumors are rare benign lesions(2,3), first described by Wood in 1812(3,4), characterized by hamartomatous proliferation originated in the neuromyoarterial glomus bodies(2). This type of tumor, also denominated glomangioma, represents approximately 2% of all the primary soft tissue tumors(5,6) and 1% to 4.5% of hand neoplasms(3,5). Usually, these tumors present like a small, reddish blue nodule measuring 3 to 10 millimeters in diameter(2). Their typical location is the subungual region of the distal phalanges, but they may be found throughout the body(1,7). Multiple lesions are extremely rare (2.3%), being most frequently found in children(1). Clinically, these lesions are characterized by intense, pulsatile, debilitating pain and sensitivity to pressure and temperature(8,9). Ungual alterations are frequently observed in cases of larger lesions and these tumors are rarely palpable. However, the clinical signs are not always obvious and, considering the small dimensions of these lesions, imaging studies are required to elucidate the diagnosis and, above all, to aid in the therapeutic/surgical planning(10,11) . The present study is aimed at analyzing the main imaging findings of subungual glomus tumors.
MATERIALS AND METHODS Eight cases of subungual glomus tumor from the archives of Clínica Multimagem Diagnósticos and Clínica da Imagem, Goiânia, GO, Brazil, were retrospectively evaluated (Table 1).
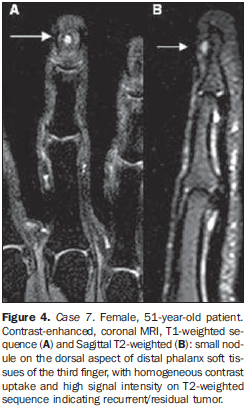
Anteroposterior and lateral radiographic images were obtained in five cases. Doppler ultrasonography (US) was performed in six patients, and non-contrast- and contrast-enhanced magnetic resonance imaging (MRI) in five cases. The diagnostic criterion adopted for subungual glomus tumor was the direct visualization of the tumor by Doppler US or MRI. Echogenicity and vascularization were evaluated at color Doppler US. Signal intensity on T1- and T2-weighted images, besides contrast (gadolinium) enhancement pattern were analyzed at MRI. Additionally, at radiography, the authors utilized an indirect criterion characterized by bone remodeling in the dorsal aspect of the distal phalanx as a positive sign of the presence of a glomus tumor. The subungual tumors were also classified according to their location, the affected digit as well as the tumor situation on the axial plane, either midline or laterally in the nail bed. All the patients had not received any treatment, except for the patient number 7 who had already been submitted to surgery five years ago, for resection of a glomus tumor in the middle finger, presenting with tumor recurrence at the time of the present study. All the cases were histopathologically confirmed after the surgical resection. Prognosis evaluation and/or patients' follow-up were not approached by the authors of the present study.
RESULTS Mean age of the patients with glomus tumors evaluated in the present study was 39 years (26 to 51 years), with a female predominance (7:1). Location of the tumors was the following: three (37%) in the index finger; two (25%) in the middle finger; two (25%) in the little finger; and one (12.5%) in the thumb. As regards axial plane location, most of the tumors were in the midline (six cases - 75%) and only two (25%) were laterally located in the nail bed. Plain radiography was positive in three among the five cases evaluated by this method (60%), demonstrating bone remodeling (pressure erosion) on the dorsal aspect of the distal phalanx (Figure 1). Doppler US was positive in five among the six patients evaluated (83%), all of them with a well-defined, solid, hypoechoic and hypervascularized subungual nodule (Figures 1 and 2). MRI was positive in the five cases evaluated, demonstrating well-defined, solid nodules with hypointense signal on T1-weighted images and signal hyperintensity on T2-weighted images with homogeneous intravenous contrast-enhancement (Figures 3 and 4).
DISCUSSION Glomus tumors are benign lesions, generally located in the hands, especially in the distal fingertips and particularly in the subungual area since glomus bodies are most numerous in these regions(8). These are rare but debilitating lesions and represent 1% to 4.5% of all hand tumors(5). Like other reports in the literature(6,8,10), the present study has demonstrated a higher female prevalence (7:1) and mean age of 39 years at the moment of the diagnosis. Usually, the diagnosis of glomus tumor is clinical, being confirmed in 50% to 78% of cases(12), but many times it is lately achieved, on average four to seven years after symptoms onset(8,13,14). The evaluation of patients' clinical data was not considered by the authors of the present study. Plain radiography, US and MRI are the imaging methods most frequently utilized in the suspicion of glomus tumor. Such methods contribute for the early diagnosis, reducing the time span between the symptoms onset and the treatment. Additionally, these methods are useful for the therapeutic planning, particularly in the definition of the surgical approach, reducing the rates of the main postoperative complication, i.e. nail dystrophia(2). Signs of bone remodeling in the dorsal aspect of the distal phalanx (pressure erosion) were observed at conventional radiography. However, this finding is present in only 14% to 60% of cases(5,15-18) (60% in the present study). Increased distance between the dorsal aspect of the distal phalanx and underside of the nail is also described as a sign of the presence of this type o tumor. However, this finding is rarely observed (25%)(2) and was seen in only one case of the present study. The low sensitivity of this method is probably related to the small size of the lesions in most of cases. Images magnification and comparison with the contralateral side are useful in the evaluation of these lesions(2). At Doppler US, a solid, well-delimited, hypoechoic nodule is observed with prominent vascularization. The limitations of this method are related to operator dependence and difficulty in the sonographic analysis of the subungual region(6). Thus, a negative study should not rule out the presence of a small-sized tumor, and investigation should proceed with surgical exploration in the setting of a well-established clinical suspicion(1). In the present study, US was positive in 83.3% of cases. At MRI, a solid, well defined nodular lesion is observed with low signal intensity in relation to the dermis of the nail bed on T1-weighted images, and high signal intensity on T2-weighted images, with homogeneous contrast-enhancement(2,7,19). Such findings were observed in all the patients of the present study evaluated with this imaging method. Additionally, MRI also depicts hyperintense lesions on T1weighted images, probably as a result of a hemorrhagic component, besides lesions with a hypointense halo and capsular aspect which have not been observed in the present study(2). MRI has also the advantage of being 3.5 times more sensitive than plain radiography in the detection of bone erosion(2). Presently, it is the most sensitive imaging method available for detecting glomus tumors, and no false negative case was observed in the present series with this method. Additionally, this method provides satisfactory information on the tumor location, aiding in the surgical planning(1). Complete surgical resection is the treatment of choice for these lesions(1). The postoperative incidence of symptoms recurrence ranges between 12-24% of cases(2). In cases where symptoms recurrence is observed within less than one year postoperatively, many authors attribute the recurrence to incomplete resection or to the presence of a second lesion that had not been previously diagnosed and surgically resected. On the other hand, in cases where the recurrence is observed within more than one year postoperatively, the fact is usually attributed to the development of a new lesion(2). Most of times, in cases of symptoms recurrence, MRI allows the differentiation between residual/recurrent tumors from postoperative fibrocicatricial alterations. Contrary to postoperative alterations that are characterized by ill-defined margins and low signal intensity on all the sequences, residual/recurrent glomus tumors correspond to well defined lesions with characteristics similar to the ones of non-treated tumors, likewise the case number 7 of the present study(1). As regards differential diagnoses, one should mention mucoid and epidermoid inclusion cysts which are avascular cystic lesions, i.e., presenting poor contrast uptake, with no flow at Doppler US and generally with no adjacent bone remodeling. Other rarer entities in this location, such as neuromas and angiomas, represent cases with difficult differential diagnosis through imaging methods. Inflammatory and deposition arthropathies, particularly gout, predominantly present alterations in the distal interphalangeal joint(6).
CONCLUSION Considering that the treatment of glomus tumors consists of complete surgical resection of the lesion(1,2), Imaging methods, especially US and MRI, have demonstrated a significant role in the diagnostic confirmation of this entity. Additionally, such methods allow an accurate determination of the tumor site, facilitating the surgical planning as well as ruling out other differential diagnoses. However, it is important to highlight the nonspecific nature of the imaging findings of these lesions and therefore, the diagnosis must be based on correlation with clinical findings(6).
REFERENCES 1. Theumann NH, Goettmann S, Le Viet D, et al. Recurrent glomus tumors of fingertips: MR imaging evaluation. Radiology. 2002;223:143-51. [ ] 2. Drapé JL, Idy-Peretti I, Goettmann S, et al. Subungual glomus tumors: evaluation with MR imaging. Radiology. 1995;195:507-15. [ ] 3. Vanti AA, Cucé LC, Di Chiacchio N. Tumor glômico subungueal: estudo epidemiológico e retrospectivo, no período de 1991 a 2003. An Bras Dermatol. 2007;82:425-31. [ ] 4. Wood W. On painful subcutaneous tubercle. Edinburgh Med J Surg. 1812;8:283-91. [ ] 5. Carroll RE, Berman AT. Glomus tumors of the hand: review of the literature and report on twenty-eight cases. J Bone Joint Surg Am. 1972; 54:691-703. [ ] 6. Fornage BD. Glomus tumors in the fingers: diagnosis with US. Radiology. 1988;167:183-5. [ ] 7. Al-Qattan MM, Al-Namla A, Al-Thunayan A, et al. Magnetic resonance imaging in the diagnosis of glomus tumours of the hand. J Hand Surg Br. 2005;30:535-40. [ ] 8. Van Geertruyden J, Lorea P, Goldschmidt D, et al. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br. 1996;21:257-60. [ ] 9. Matsunaga A, Ochiai T, Abe I, et al. Subungual glomus tumour: evaluation of ultrasound imaging in preoperative assessment. Eur J Dermatol. 2007;17:67-9. [ ] 10. Kale SS, Rao VK, Bentz ML. Glomus tumor of the index finger. J Craniofac Surg. 2006;17:801-4. [ ] 11. Chen SH, Chen YL, Cheng MH, et al. The use of ultrasonography in preoperative localization of digital glomus tumors. Plast Reconstr Surg. 2003;112:115-9. [ ] 12. Drapé JL, Idy-Peretti I, Goettmann S, et al. Standard and high resolution magnetic resonance imaging of glomus tumors of toes and fingertips. J Am Acad Dermatol. 1996;35:550-5. [ ] 13. Hsu CJ, Wang DY. Glomus tumors. Mid Taiwan J Med. 2002;7:222-7. [ ] 14. Drapé JL, Feydy A, Guerini H, et al. Vascular lesions of the hand. Eur J Radiol. 2005;56:331-43. [ ] 15. Holzberg M. Glomus tumor of the nail. A 'red herring' clarified by magnetic resonance imaging. Arch Dermatol. 1992;128:160-2. [ ] 16. Matloub HS, Muoneke VN, Prevel CD, et al. Glomus tumor imaging: use of MRI for localization of occult lesions. J Hand Surg Am. 1992;17:472-5. [ ] 17. Camirand P, Giroux JM. Subungual glomus tumor: radiological manifestations. Arch Dermatol. 1970;102:677-9. [ ] 18. Takemura N, Fujii N, Tanaka T. Subungual glomus tumor diagnosis based on imaging. J Dermatol. 2006;33:389-93. [ ] 19. McDermott EM, Weiss APC. Glomus tumors. J Hand Surg Am. 2006;31:1397-400. [ ] Received May 30, 2009. * Study developed at Clínica da Imagem and Clínica Multimagem Diagnósticos, Goiânia, GO, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554